Anticoagulation in the Surgical Management of Peripheral Arterial Embolic Disease
Martha E Nixon, Keith Gomes Pinto, Marcos S Kostalas, David J Williams and John V Taylor
DOI10.21767/2573-4482.100064
Affiliated with North Devon District General Hospital, Raleigh Park, Barnstaple, EX31 4JB, UK
- *Corresponding Author:
- Martha Nixon
General Surgical Registrar, South Devon and District Hospital
Newton Road, Torbay, TQ2 7AA, UK.
Tel: 400447411006623
E-mail: martha.nixon@nhs.net
Received date: September 28, 2017; Accepted date: October 25, 2017; Published date: October 31, 2017
Citation: Nixon ME, Pinto KG, Kostalas MS, Williams DJ, Taylor JV (2017) Anticoagulation in the Surgical Management of Peripheral Arterial Embolic Disease. J Vasc Endovasc Surg. 2:31. doi: 10.21767/2573-4482.100064
Abstract
Introduction: Low-molecular-weight heparin has been showed to be effective for veno-occlusive disease and acute coronary syndrome. It is frequently used for peripheral arterial embolic disease but this is not a licensed use and there is little evidence or guidelines for this. This article aims to review the peri-operative use and outcomes of LMWH and unfractionated heparin (UFH) following arterial embolectomy in a district general hospital.
Methods: Retrospective case review of peri-operative anticoagulation in 55 patients undergoing peripheral arterial embolectomy between 2007-2012 in North Devon District Hospital.
Results: Patients received a wide variety of anti-coagulation in the peri-operative period. The overall complication rate was 38%. The total complication rate was 70% in patients receiving UFH compared to 42% in those receiving LMWH (p=0.16). The risk of re-occlusion was 60% in the UFH group compared to 18% in the LMWH group (p=0.21). The risk of amputation was higher in the UFH group (30% compared to 12% p=0.32).
Conclusion: LMWH is a safe and convenient alternative to UFH in acute peripheral arterial thromboembolic disease.
Keywords
Low-molecular-weight; Heparin; Peripheral arterial disease
Introduction
Peripheral arterial embolic disease is a common vascular emergency. Surgical management with embolectomy is the treatment of choice [1,2]. Current evidence suggests that rapid embolectomy can improve the outcome of this condition and should happen within 24 h [3-6]. Despite this, time to surgery can be prolonged secondary to delayed patient presentation, centralisation of vascular services resulting in patient transfer between hospitals and pressure on provision of emergency theatre. In circumstances where surgery is delayed pre-operative anticoagulation is commonly administered. Post-operative anticoagulation is used to prevent complications associated with surgery, including re-occlusion [6,7]. In the peri-operative period options for anticoagulation include unfractionated heparin (UFH) and low molecular weight heparin (LMWH). There is currently good evidence to support the use of LMWH over UFH in thromboembolic conditions such as deep venous thromboembolism and acute coronary syndrome [8-14]. LMWH has now replaced the use of UFH in these conditions due to a lower complication rate [9]. LMWH is an attractive treatment option as it is easily dosed and does not require regular blood tests to monitor levels required with UFH. Not only does this make it more convenient but it also has important cost implications [15,16]. Despite the current evidence supporting the use of LMWH instead of UFH in veno-occlusive conditions there is no current guidance in patients with peripheral arterial embolic disease. LMWH is commonly used in arterial embolic disease but it has yet to be granted a licence for use in this situation.
The aim of this study was to review the peri-operative use and outcomes of LMWH and UFH following peripheral arterial embolectomy in our institution.
Methods
A retrospective case review was performed on all patients undergoing peripheral arterial embolectomy over a five year period in North Devon District Hospital, Barnstaple UK. The theatre database was used to identify all patients undergoing peripheral arterial embolectomies between 1st December 2007 and 31st December 2012. A thorough review of patient notes was performed which included gathering information from clerking proformas, daily entries during admission, operation notes, drug charts, anaesthetic charts, electronic discharge summaries and outpatient clinic letters. In instances where information was missing General Practitioners were contacted in order to obtain this. The outcomes between those groups of patients receiving LMWH and UFH post operatively were compared for statistical significance using Fischer’s exact test.
Results
From the 1st December 2007 to 31st December 2012 seventy eight patients were coded as having undergone emergency arterial embolectomy. Fourteen patients were excluded due to incorrect coding. Nine patients were excluded from the review as their notes were either unavailable or did not contain sufficient information for inclusion in this review. Fifty five patients were therefore included in this case review.
Of the 55 patients, 33 were male (60%) and 22 were female (40%). The mean age of the cohort was 73 years (range 39-100 years).
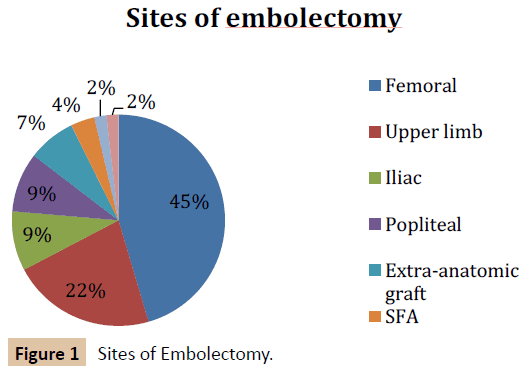
Sites of embolectomy were as follows: 25 femoral (45.5%), 12 upper limb (21.8%), 5 iliac (9.1%), 5 popliteal (9.1%), 4 extraanatomic grafts (7.3%), 2 superficial femoral artery (3.6%), 1 profunda artery (1.8%) and 1 tibial artery (1.8%) (Figure 1).
It was noted that in this cohort of patients the comorbidity rate was high, with 96% of patients having at least one comorbidity (range 0-3). The most common number of comorbidities was one. When the patients were separated according to the postoperative anticoagulation that they received there was no statistically significant difference between the comorbidities in the two main groups of those receiving LMWH and heparin (p=0.67, Mann Whitney U test).
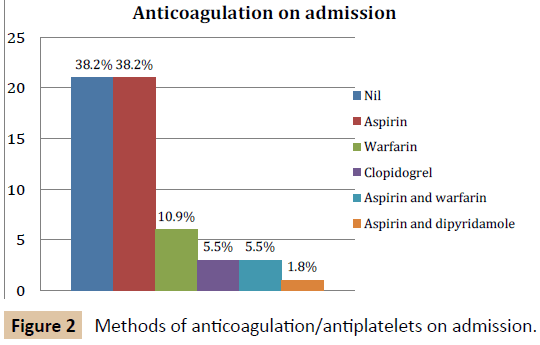
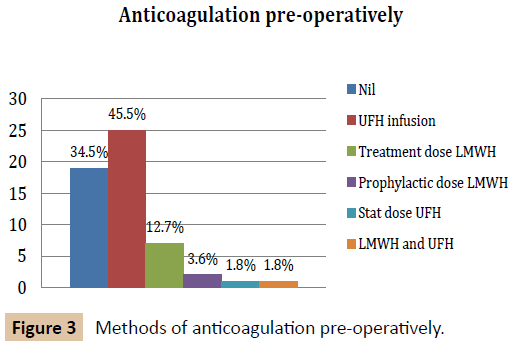
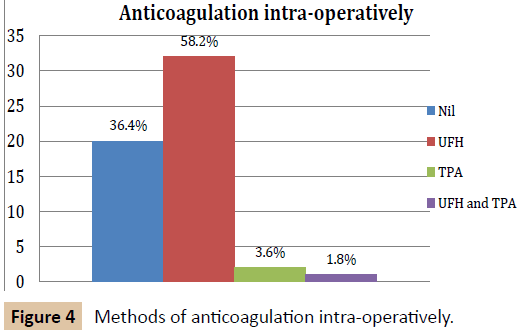
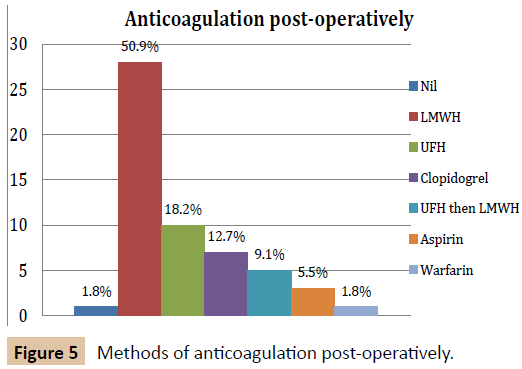
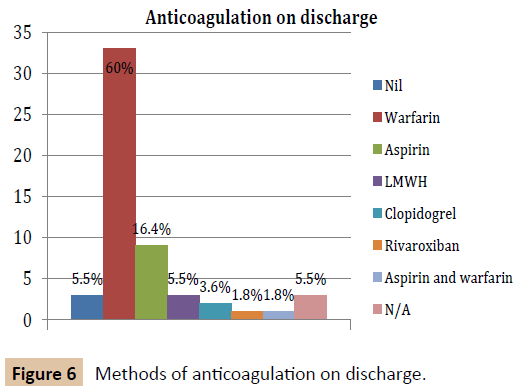
There was marked variation in peri-operative anticoagulation in this group of patients (Figures 2-6). All patients except for one received some form of anticoagulation post-operatively. This patient was placed on a palliative care pathway at the end of the procedure instead of continuing with active treatment.
There were a total of 21 (38%) complications in this case review. There were 3 peri-operative deaths (5%). The complications included amputations, re-occlusion, haematomas and infections (Table 1). No patients had any problems with active bleeding.
| Complication | LMWH | UFH | LMWH + UFH | Oral anticoagulants | Overall |
|---|---|---|---|---|---|
| Haematoma | 3 (9%) | 0 | 1 (25%) | 0 | 4 (7%) |
| Wound infection | 2 (6%) | 1 (10%) | 0 | 0 | 3 (5%) |
| Re-occlusion | 2 (6%) | 1 (10%) | 0 | 0 | 3 (5%) |
| Amputation | 4 (12%) | 3 (30%) | 0 | 0 | 7 (13%) |
| Claudication | 0 | 2 (20%) | 0 | 0 | 2 (4%) |
| 30 day mortality | 2 (6%) | 0 | 0 | 0 | 3 (4%) |
| Total | 13 (33%) | 7 (70%) | 1 (25%) | 0 | 21 (38%) |
Table 1: Post-operative complications.
The overall complication rate was 38%. The complication rate in the group receiving post-operative UFH was 70% whilst the complication rate in those receiving LMWH was 42% (p=0.16 using Fischer’s exact test). The complication rate in those receiving UFH and then LMWH was 25% and on those receiving oral anticoagulants was 0%. Risk of re-occlusive problems (re-occlusion, amputation and claudication) was 60% in those receiving UFH compared to 18% in those receiving LMWH (p=0.21). The risk of amputation was 30% in the UFH group compared with 12% in the LMWH group. This difference was not significant (p=0.32). The risk of haematoma was highest in the group receiving UFH and LMWH (25%). The haematoma rate for LMWH was 9%. There were no haematomas in the UFH group.
The one year mortality of this study was 23.8% with a two year mortality rate of 35.9%.
Discussion
Patients with acute arterial embolic disease received a range of anti-coagulation in the peri-operative period. Choice was dependent on the preference of the admitting surgeon and was markedly varied. This variation reflects the current lack of sufficient evidence and guidance on the subject. In a larger hospital with more doctors the variation may be even more pronounced.
A large number of patients did not receive any anti-coagulation (34.5%) pre-operatively. This is likely to be due to a rapid transit from admission to emergency surgery at our hospital and therefore lessening the importance of pre-operative anticoagulation.
Patients were also discharged on a variety of anti-coagulation regimens. This may be partly due to surgeon preference but is most heavily influence by patient factors. Some would argue that this group of patients has such complex needs and varying comorbidities producing an agreed protocol would be difficult. Patients suffering with strokes are a similar group of patients and clear guidance regarding secondary prevention has been formulated [14,17]. It has been recognised that further research into patients with arterial embolic disease is needed [6]. This would then allow clear guidance to be produced. This study has highlighted how useful this would be in order to optimise care in this select group.
The overall complication rate in this review was 38% with an overall 30 day mortality rate of 4%. Whilst this figure is high, it is consistent with the range of mortality rates found in similar studies (mortality ranges from 3.76%-38% [18-22]. The one year mortality rate was 23.8%. The two year mortality rate was 35.9%. This reflects the high rate of comorbidities in this group of patients. The overall rate of amputation was 13%. This is line with other studies [18-20]. The high risk nature of the condition and surgery should be conveyed when counselling patients and family members in the peri-operative period.
The overall complication rate in the group receiving postoperative UFH was 70% compared to 33% in the group receiving LMWH. This difference was not found to be statistically significant (p=0.16). The risks secondary to further occlusion was higher in the UFH group compared with that of the LMWH group, but this was not statistically significant (UFH 60% vs. LMWH 18%, p=0.21). The risk of amputation was higher in the UFH group, but again this difference was not shown to be significant (30% compared to 12%, p=0.32). Our finding of a higher incidence of re-occlusive disease in those receiving UFH is consistent with findings of a study performed by Robinson et al. In this study the dose of UFH was found to be subtherapeutic 30% of the time [23]. Unlike some previous studies we found that there was a higher incidence of haematoma and death in the LMWH group than the UFH group [24-26]. A recent Cochrane review showed a higher risk of major bleeding in medical patients treated for DVT with UFH than LMWH, in line with our study [9]. The authors wish to highlight that although this study shows a trend towards improved outcomes with LMWH in line with other studies this cannot be confirmed as the numbers were very low. This study cannot be used to show any advantage of one treatment modality over the other. Instead the authors believe that it highlights the need for additional, larger studies in this area. Currently many centres are using LMWH off licence due to the benefits proven in other diseases and due to positive clinical experiences. If better quality evidence proved this to be the case in peripheral arterial embolic disease then the recommendations and licencing could be changed.
Conclusion
LMWH has been shown to provide a more convenient and cheaper alternative to UFH in other conditions. This study has shown that LMWH is a safe alternative to UFH in peripheral arterial thromboembolic disease. The widespread use of LMWH in this group of patients could have important financial implications.
This study has highlighted the haphazard approach to anticoagulation peri-operatively and on discharge and the need for further good quality research and guidelines in this area.
References
- Constantini V, Lenti M (2002) Treatment of acute occlusion of peripheral arteries. Thrombosis Research 106: 285-294.
- Baxter-Smith D, Ashton F, Slaney G (1998) Peripheral arterial embolism. A 20 year review. J Cardiovasc Surg 29: 453-457.
- Dag O, Kaygin MA, Erkut B (2012) Analysis of risk factors for amputation in 822 cases with acute arterial emboli. Scientific World J.
- Mutirahgura P, Ruangsetakit C, Wongwanit C, Sermsathanasawadi N, Chinsakchai K (2008) Acute arterial embolism of the lower extremities: impact of 24-hour duration on the outcome of management. J Med Assoc Thai 91: 1360-1367.
- Vohra R, Zahrani H, Lieberman DP (1991) Factors affecting limb salvage and mortality in patients undergoing femoral embolectomy. J R Coll Surg Edinb 36: 213-215.
- American Heart Association and American College Cardiology (2016) 2016 AHA/ACC Guideline on the management of patients with lower extremity peripheral arterial disease: executive summary. Vascular Medicine 22: 1-43.
- Winkler MS, Larena-Avellaneda A, Diener H, Kolbel T, Debus ES (2012) Risk-adjusted strategies in the prevention of early arterial thrombosis following extremity arterial reconstruction: a comparison of unfractionated versus low molecular weight heparin. J Cardiovasc Surg 54: 183-192.
- Alikhan R, Cohen AT (2009) Heparin for the prevention of venous thromboembolism in general medical patients (excluding stroke and myocardial infarction). Cochrane Database Syst Rev.
- Alikhan R, Bedenis R, Cohen AT (2014) Heparin for the prevention of venous thromboembolism in acutely ill medical patients excluding stoke and myocardial infarction. Cochrane Database Syst Rev 7: CD003747.
- Constantino G, Ceriani E, Rusconi AM, Podda GM, Montano N (2012) Bleeding risk during treatment of acute thrombolic events with subcutaneous LMWH compared to intravenous unfractionated heparin; a systematic review. PLoS One 7: e44553.
- Erkens PM, Prins MH (2010) Fixed dose subcutaneous low molecular weight heparins versus adjusted dose unfractionated heparin for venous thromboembolism. Cochrane Database Syst Rev.
- Magee KD, Sevcik W, Moher D, Rowe BH (2003) Low molecular weight heparins versus unfractionated heparin for acute coronary syndromes. Cochrane Database Syst Rev.
- Latour-Perez J, de-Miguel-Balsa E (2012) Cost effectiveness of anticoagulation in acute coronary syndromes. Pharmacoeconomics 30: 303-321.
- Santos-Gallego CG, Bayron J, Badimon JJ (2010) Thrombi of different pathologies: implications for diagnosis and treatment. Curr Treat Options Cardiovasc Med 12: 274-291.
- Argenta C, Ferreira MA, Sander GB, Moreira LB (2011) Short-term therapy with enoxaparin or unfractionated heparin for venous thromboembolism in hospitalized patients: utilization study and cost-minimization analysis. Value Health 14: S89-S92.
- Merli G, Ferrufino CP, Lin J, Hussein M, Battleman D (2010) Hospital-based costs associated with venous thromboembolism prophylaxis regimens. J Thromb Thrombolysis 29: 449-458.
- Warburton E, Alawneh JA, Clatworthy PL, Morris RS (2010) Stroke management. BMJ Clin Evid Apr.
- Schumann R, Rieger J, Ludwig M (2007) Acute peripheral arterial occlusive disease. Med Klin 102: 457-471.
- Gossage JA, Ali T, Chambers J, Burnand KG (2006) Peripheral arterial embolism: prevalence, outcome, and the role of echocardiography in management. Vasc Endovasc Surg 40: 280-286.
- Hu HD, Chang Q, Chen z, Liu C, Ren YY, et al. (2011) Management and prognosis of acute arterial embolism: a multivariable analysis of 346 patients. National Medical Journal of China 91: 2923-2926.
- Braithwaite BD, Davies B, Birch PA, Heather BP, Earnshaw JJ (1998) Management of acute leg ischaemia in the elderly. Br J Surg 85: 217-220.
- Pentti J, Salenius JP, Kuukasjarvi P, Tarkka M (1995) Outcome of surgical treatment in acute upper limb ischaemia. Ann Chir Gynaecol 84: 25-28.
- Robinson T, Hunter I, Wathes R, Keeling D, Hands L (2009) Audit of anticoagulation after embolectomy for acute ischaemia. Ann of Surg 91: 470-472.
- Chen LY, Ying KJ, Hong WJ, Zhou P (2005) Comparison of low-molecular-weight heparin and unfractionated heparin for acute PTE. Journal of Zhejiang University. Med Sci 6: 1195-1199.
- Junqueira DR, Perini E, Penholati RR, Carvalho MG (2012) Unfractionated heparin versus low molecular weight heparin for avoiding heparin-induced thrombocytopenia in post-operative patients. Cochrane Database Syst Rev.
- Akl EA, Labedi N, Terrenato I, Barba M, Sperati F, et al. (2011) Low molecular weight heparin versus unfractionated heparin for perioperative thromboprophylaxis in patients with cancer. Cochrane Database Syst Rev.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences