Inflammatory Responses in Varicose Veins Surgery: Conventional Venous Stripping and Endovenous Radiofrequency Ablation (EV-RFA)
Nawaphan Taengsakul, Tanasit Saikaew, Norraporn Chaiaroon, Thatchawit Urasuk, Anucha Panoi, Thamrongroj Temudom and Pisake Boontham
DOI10.21767/2573-4482.19.04.9
Nawaphan Taengsakul1*, Tanasit Saikaew2, Norraporn Chaiaroon2, Thatchawit Urasuk1, Anucha Panoi2, Thamrongroj Temudom2 and Pisake Boontham2
1 Department of Surgery, Chulabhorn hospital, Bangkok, Thailand
2Division of Vascular Surgery, Department of Surgery, Phramongkutklao hospital, Bangkok, Thailand
- *Corresponding Author:
- Taengsakul N
Department of Surgery, Chulabhorn hospital, Bangkok, Thailand
Tel: 66839316688
E-mail: ploynawa@hotmail.com
Received date: March 20, 2019; Accepted date: April 01, 2019; Published date: April 15, 2019
Citation: Taengsakul N, Saikaew T, Chaiaroon N, Urasuk T, Panoi A, et al. Inflammatory Responses in Varicose Veins Surgery: Conven-tional Venous Stripping VS Endovenous Radiofrequency Abla-tion (EV-RFA). J Vasc Endovasc Therapy 2019, Vol.4 No.1:9.
Copyright: © 2019 Taengsakul N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Varicose veins surgery was evolved in the past decade. Many studies showed that endovenous ra-diofrequency ablation (EV-RFA), a novel method for varicose veins treatment, produced complications fewer than conventional venous stripping, particularly postoperative pain and ecchymosis. There were a lot of studies reported about inflammatory response but there were few studies compare inflammatory response between procedures. This study purpose compares preoperative and postoperative level of serum Interleukin 6 (IL-6) and C-reactive protein (CRP) to determine the inflammatory response of EV-RFA and conventional venous stripping. This study also compares visual analogue scale (VAS) and ecchymoses between these two procedures.
Methods: A prospective cohort study measuring IL-6 and CRP level at before and 24-hour after surgery in sympto-matic varicose vines patients who underwent either EV-RFA or conventional venous stripping.
Results: Fifty-nine patients were included, 27 patients were treated by conventional venous stripping and 32 pa-tients were treated by EV-RFA. There was no different in demographic characteristics among two groups. Twenty-four hour postoperative level of IL-6 and CRP significantly increased (p<0.001 and<0.001, respectively) in both EV-RFA group (p<0.001 and<0.001, respectively) and venous stripping group (p=0.043 and <0.001, respectively) com-pare to preoperative level. Increasing in 24 h postoperative level of IL-6 and CRP in EV-RFA group was significantly lower than in venous stripping group (p<0.001 and p=0.045, respectively). Postoperative VAS and ecchymosis were also significantly different between EV-RFA group and venous stripping group (p<0.001 and p<0.001, respectively).
Conclusions: EV-RFA produced inflammatory response, VAS and ecchymosis significantly lower than conventional venous stripping.
Keywords
Angiosome; Critical limb ischemia; Collateral circulation; Ulcer healing; Limb salvage; Diabetic ulcer
Introduction
Chronic venous insufficiency (CVI) is common lower extremity vascular pathologies with great medical and socioeconomic impact. It cost 1%-2.5% of health care budgets in developed countries. It affected worldwide population with prevalence of 73% in female and 56% in male. It significantly decreased quality of life of affected patients [1]. It presented with wide spectrum of clinical manifestations from varicose veins, limb edema, hyperpigmentation of skin, and finally, the development of venous ulcer. It also included deterioration in morphological and functional alterations of the venous system, occurred with signs and symptoms varying in type and severity that categorized by the clinical, etiological, anatomical, and pathological (CEAP) classification [2].
Main pathophysiologic mechanism of CVI is venous hypertension caused by shear stress and reflux from incompetent valves [3]. Venous hypertension caused venous dilatation, worsened valvular insufficiency, and increased intravenous pressure. Changing in hemodynamics interfered microcirculation, endothelial cells (ECs) and vessel microenvironment, leading to venous microangiopathy, and, dilation and tortuosity of capillary beds [3]. The mechanosensors of endothelial cells were triggered by altered hemodynamics, transduced physical signals into harmful pathways resulting in ECs damages. Particularly these complex biological processes activated inflammatory and proteolytic cascades in vascular microenvironment including leukocyte adhesion, degranulation, and releasing of cytoplasmic granules from neutrophils, macrophages, mastocytes, ECs, and platelets [4]. All of these mechanisms lead into impairing of both microcirculatory and macrocirculatory systems, caused remodeling of the venous walls and valves, venous hypertension, formation of varicosities, edema, and leg ulceration [3,5].
Inflammation was an essential immune response to pathogens and damaged cells. In varicose veins, there were refluxes and incompetent valves, and venous wall dilation resulting in increased venous pressure. Phenotypic modulation of vascular smooth muscle cells (VSMC) altered extracellular matrix (ECM) metabolisms. Angiogenesis was main mechanisms contributing morphological and functional modifications of varicose veins remodeling. Inflammatory cytokines and adhesion molecules included transforming growth factor beta (TGF-β), interleukin 6 (IL-6), interleukin 8 (IL-8) and vascular cell adhesion molecule 1 (VCAM-1) [6]. Increased venous wall tension created matrix metalloproteinases (MMPs) activities, which induced ECM degradation and affected structural integrity of the venous walls. ECs injury also triggered inflammation by leukocytes infiltration and activation, resulting in further venous wall damage and fibrosis, leading to progressive venous insufficiency and varicose veins formation. Monocytes and macrophages migrated into venous wall and valve turning patient into venous insufficiency. Venous stasis caused inflammatory cytokines releasing by monocyte and macrophage including interleukin-1b (IL-1b), IL-6 and tumor necrosis factor alpha (TNF-α). Refluxed vein activated ECs of luminal vein and vasa vasorum, indicated by up regulation of intercellular adhesion molecule 1 (ICAM-1), interleukin 1a (IL- 1a) and TNF-α [7].
Treatment of varicose veins was conventional surgery and endovenous treatment. Conventional surgical treatment was high ligation and stripping. Modern endovenous treatments were defined such as endovenous radiofrequency ablation (EV-RFA), endovenous laser ablation (EVLA), sclerotherapy, mechanochemical endovenous ablation, N-butyl-2-cyanoacrylate injection. High ligation and venous stripping (HL/VS) was traditional treatment that caused unsatisfactory cosmetic outcome for concerning patients due to multiple incisions. However, HL/VS still indicated in some situations including superficial saphenous tributary adherent closely to skin less than 1 cm, tortuous superficial veins, aneurysmal venous segment larger than 2.5 cm, chronic thrombophlebitis and acute superficial thrombosis [8]. Endovenous treatment was an alternative treatment giving better cosmetic result and faster recovery. Rasmussen et al. reported results of four-arm RCT and concluded that postoperative pain was higher in HL/VS and EVLA, although efficacy of four modalities was not significantly different [9]. In past decade, most of patients with varicose veins in our institute were treated by HL/VS and EV-RFA. We questioned in difference of inflammatory reaction between our both varicose veins treatment options. Study of inflammatory responses and clinical outcomes was designed. IL-6 secreted by T-cell and macrophage responded to tissue trauma. Smooth muscle cells produced IL-6 as a proinflammatory cytokine induced activities of B-lymphocyte and cytotoxic T-lymphocyte. C-reactive protein (CRP) is acutephased reactant protein produced by inflammation and tissue trauma response of hepatocyte. CRP level start increasing in 6 to 10 hours and peaked at 36-50 hours after inflammation or trauma. It returned to normal level within 1-2 weeks [10].
This study was designed to compare the difference of preoperative and 24-hour postoperative inflammatory response from tissue trauma after HL/VS and EV-RFA, identified by serum level of IL-6 and CRP.
Materials and Methods
Institutional review board of royal thai army medical department approved this prospective study. All patients gave inform consent to this protocol. A prospective cohort study was performed in patients who were diagnosed symptomatic varicose veins with reflux underwent operation from September 1st, 2013 to August 31st, 2015 in Phramongkutklao hospital. Included patients got symptomatic varicose vein with reflux in great saphenous vein (GSV). All of patients were 18 years of age or older, and were ask to consent to enroll in study. The patients with connective tissue disease, autoimmune disease, cirrhosis, end stage real disease and hematologic disease were excluded from study. Patients who presented with venous ulcer or elsewhere infection were also excluded. Patients with history of recent trauma were not enrolled in study.
Data collection
Demographic data including age, sex, clinical symptom, professional, underlying conditions, diameter of superficial vein and GSV. Preoperative and postoperative serum level of IL-6 and CRP were noted. Postoperative visual analogue scales and ecchymosis were evaluated. Serum level of IL-6 and CRP were compared preoperatively and 24-hour postoperatively.
Venous blood sampling
Venous blood samples were manually drawn by direct puncture using 23-gauge needle from antecubital vein. Five cubic milliliters of venous blood was collected into citrated tube and sent to laboratory under dry ice in air courier. Supernatant plasma was manually separated and stored at 20°C for batch analysis. Both preoperative and 24-hour postoperative blood samples were collected in the same technique.
Diagnostic of great saphenous vein (GSV) reflux
Venous duplex ultrasonography was done for diagnosis of GSV reflux and evaluating anatomy of vein by radiologist. Deep vein thrombosis (DVT) was ruled out under standard venous duplex examination. Venous duplex reflux examination included B-mode and color-flow imaging of deep and superficial vein, and pulsed doppler assessment of flow direction. Flow direction was evaluated with provocative maneuver either Valsava maneuver or augmenting flow with distal limb compression. Reversal of flow in superficial veins lasting more than 0.5 second indicated valvular incompetence and reversal of flow in superficial veins lasting more than 1 second indicated deep system reflux [11]. Diameter of GSV and superficial vein were collected.
High ligation with venous stripping
Operation was done under either general anesthesia or regional anesthesia. Oblique incision was done parallel to groin crease, or 1-2 cm below in obese patients. GSV was identified and its tributaries were ligated. High ligation was done closely to femoral vein. Proximal ligation was done with simple and suture ligation as double ligation. Transverse venotomy was done and stripper was pass distally until knee level. Small incision was done at area where stripper was palpated. GSV was stripped in either upward or downward direction. If cosmetic issue was concerned, stab avulsion was simultaneously performed.
Endovenous radiofrequency ablation
Operation was done under regional anesthesia. We used the Covidien ClosureFAST™ catheter that constructed with a 7 cm bipolar electrode affixed to distal end. Ablation of GSV was started below popliteal area. Patient was in reverse trendelenburg position. Access site was performed with percutaneous puncture by 21-gauge needle under ultrasound guidance. A 7-Fr, 10 cm sheath (Radiofocus Introducer II standard kit-Introducer sheath; Terumo intervention system) was advanced over the wire and 7-Fr ClosureFAST™ catheter was inserted. The catheter tip was advanced to optimal point at 2.0-2.5 cm from saphenofemoral junction (SFJ). Proper placement of the catheter tip was confirmed by ultrasound. Perivenous tumescent anesthesia was administered under ultrasound guidance along entire targeted venous segment creating a fluid layer around GSV. Sufficient tumescent anesthesia was injected until 10-mm diameter of fluid around GSV was created and forming a 10-mm distance between the targeted vein and skin. A representative mixture of 40 ml of 1% lidocaine with epinephrine in 450 ml of normal saline, neutralized by 10 ml of 7.5% sodium bicarbonate. After performing tumescent anesthetic, patient turned into trendelenburg position, making vein collapsed and exsanguinated. Location of catheter tip was confirmed with ultrasound before ablation. By segmental ablation technique of the ClosureFAST™ system, each 7 cm segment was treated independently for 20 seconds each interval. In each treatment cycle, temperature must be 120°C for 5 seconds after initiation of energy delivery. If proper temperature did not achieved, 20 seconds treatment cycle was repeated. Finally, duplex ultrasonography was performed to evaluate treated vein for absence of reflux and evidence of occlusion.
Postoperative evaluation and management
Postoperative pain was evaluated by visual analogue pain scale. The presence of ecchymosis and numbness were recorded at the morning after intervention. Postoperative compression with a 30 to 40 mm Hg graduated stocking was applied for at least 1 week. Patients were instructed to ambulate immediately after procedure. Follow-up evaluations were performed at 1 week.
Statistical analysis
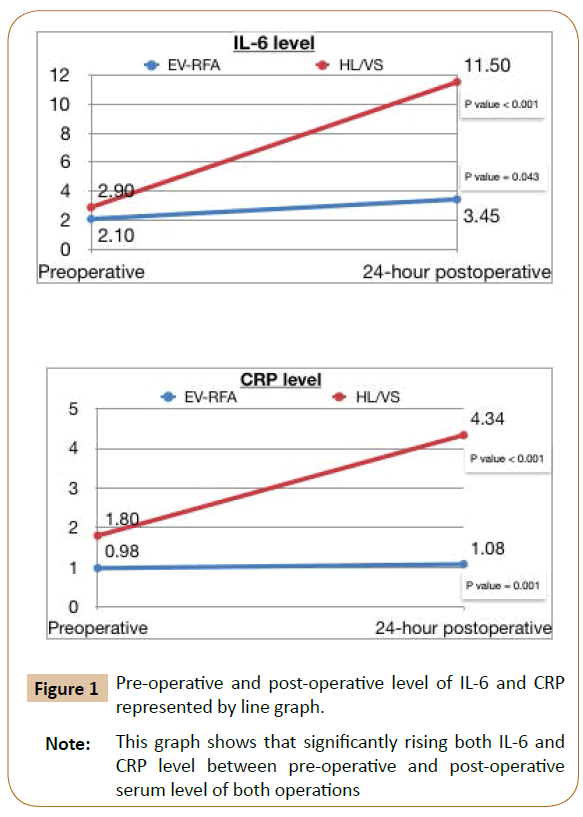
Demographic data, patient’s characteristics and clinical results were evaluated by Chi square test. Postoperative pain was defined by visual analogue scale. The presence of ecchymosis and numbness was compared by Chi square test. Preoperative and 24 h postoperative serum level of IL-6 and CRP were analyzed by Mann-Whitney U test and Fisher’s exact test. Difference in preoperative and postoperative serum level of IL-6 and CRP were compared between EV-RFA group and HL/VS group by Wilcoxon signed ranks test (Figure 1).
Results
59 patients were enrolled, 32 patients were in EV-RFA group and 27 patients were in HL/VS group. Mean age of patients were 56 and 52 years old in EV-RFA and HL/VS groups respectively. Male was 31.3% in EV-RFA group and 48.1% in HL/VS group. Most of patient’s professional were housewife, teacher and government officer. Three major underlying medical comorbidity were hypertension, diabetes mellitus and dyslipidemia. Most common clinical presentation was heaviness in legs for both groups. Average size of superficial vein and GSV was 3-5 mm and 5-10 mm respectively for both groups (Tables 1 and 2).
| Characteristics | EV-RFA (32) n (%) |
HL/VS (27) n (%) |
p-value |
|---|---|---|---|
| Age (years ) mean (SD) |
56.03 (14.46) | 51.89 (10.77) | 0.235 |
| Sex | 0.185 | ||
| male | 10 (31.3) | 13 (48.1) | |
| female | 22 (68.8) | 14 (51.9) | |
| Underlying disease | |||
| DM | 8 (25) | 2 (7.4) | 0.073 |
| HT | 10 (31.3) | 8 (29.6) | 0.893 |
| DLP | 3 (9.4) | 4 (14.8) | 0.520 |
| Career | |||
| Farmer | 1 | 1 | |
| Government officer | 6 | 4 | |
| Housewife | 6 | 7 | |
| Teacher | 9 | 8 | |
| Soldier | 4 | 4 | |
| Shopkeeper | 4 | 3 | |
| Symptom | |||
| Aching | 16 (50) | 14 (51.9) | 0.887 |
| Heaviness | 17 (53.1) | 16 (59.3) | 0.636 |
| Cramping | 6 (18.8) | 8 (29.6) | 0.328 |
| Edema | 9 (28.1) | 6 (22.2) | 0.604 |
| Hyperpigmentation | 5 (15.6) | 2 (7.4) | 0.331 |
| Superficial vein | 0.780 | ||
| 1-3 mm | 7 (21.9) | 4 (14.8) | |
| 3-5 mm | 21 (65.6) | 19 (70.4) | |
| >5 mm | 4 (12.5) | 4 (14.8) | |
| GSV | 0.513 | ||
| <5 mm | 0 (0) | 1 (3.7) | |
| 5-10 mm | 27 (84.4) | 21 (77.8) | |
| >10 mm | 5 (15.6) | 5 (18.5) | |
| Note: This table shows that both of EV-RFA group and venous stripping group were not significantly difference in demographic data. | |||
Table 1: Demographic data and patient characteristics (Total n=59).
| Clinical | EV-RFA (32) n (%) |
HL/VS (27) n (%) |
p-value |
|---|---|---|---|
| Pain score <0.001* | |||
| Mean ± SD | 1.41±1.1 | 3.89±1.53 | |
| Median (min-max) | 1 (0-4) | 4 (1-7) | |
| Ecchymosis | <0.001* | ||
| no | 29 (90.6) | 11 (40.7) | |
| yes | 3 (9.4) | 16 (59.3) | |
| Numbness | 0.456 | ||
| no | 31 (96.9) | 25 (92.6) | |
| yes | 1 (3.1) | 2 (7.4) | |
| Note: This table shows that EV-RFA group had better pain score and ecchymosis compares with HL/VS group. We found equivalent result of numbness in both groups. | |||
Table 2: Clinical results (Total n=59).
Mean VAS was significantly lower in EV-RFA group compare to HL/ VS (1.41 ± 1.1 vs. 3.89 ± 1.53, p<0.001). Postoperative ecchymosis was also significantly lower in EV-RFA (9.4% vs. 59.3%, p<0.001). Numbness was not significantly among two groups (3.1% vs. 7.4%, p=0.456). There was no significant difference of median baseline level of IL-6 between EV-RFA and HL/VS group (p=0.05), however, there was significant difference of median baseline level of CRP among two groups. (p=0.045). Both IL-6 and CRP level increased significantly from preoperative to 24-hour postoperative in both EV-RFA (p<0.001 and p=0.043, respectively) and HL/VS (p<0.001 and p =0.001, respectively) group. Rising of IL-6 and CRP level were lower in EV-RFA group compare to HL/VS group (p<0.001 and p=0.045, respectively) (Tables 3-5).
| EV-RFA | HL/VS | p-value | |
|---|---|---|---|
| Median | Median | ||
| IL-6 | 2.10 (1.5-9.39) | 2.90 (1.5-23.5) | 0.05 |
| CRP | 0.98 (0.0-7.13) | 1.8 (0.14-12.45) | 0.045 |
| Note: This table shows that no significantly of preoperative level of IL-6 and CRP in both groups. | |||
Table 3: Baseline of preoperative level of IL-6 and CRP.
| Median | p-value | |
|---|---|---|
| IL-6 | ||
| EV-RFA | <0.001 | |
| Preoperative | 2.10 (1.5-9.39) | |
| Postoperative | 3.45 (2.0-16.91) | |
| HL/VS | 0.043 | |
| Preoperative | 2.90 (1.5-23.5) | |
| postoperative | 11.50 (3.5-179.6) | |
| CRP | ||
| EV-RFA | <0.001 | |
| Preoperative | 0.98 (0.0-7.13) | |
| Postoperative | 1.08 (0.19-13.12) | |
| HL/VS | 0.001 | |
| preoperative | 1.8 (0.14-12.45) | |
| postoperative | 4.34 (0.17-93.46) | |
| Note: This table show preoperative and postoperative level of IL-6 and CRP of both operations. We found that IL-6 was significantly rising in EV-RFA groups but not increasing in Hl/VS group and CRP level was significantly rising in both groups. | ||
Table 4: Pre-operative and post-operative level of IL-6 and CRP.
| EV-RFA | HL/VS | p-value | |
|---|---|---|---|
| Median | Median | ||
| IL-6 | 1.15 (-3.44-12.2) | 8.61 (-1.1-174.8) | <0.001 |
| CRP | 0.11 (-1.11-11.25) | 0.7 (-3.49-86.98) | 0.045 |
| Note : This table show that inflammatory response ( Postoperative level- Preoperative level ) of IL-6 and CRP in both of operations. We found that significanly rising of IL-6 and CRP of both operations. | |||
Table 5: Comparison of pre-operative and post-operative inflammatory response between EV-RFA and venous stripping.
Discussion
Demographic data, consisted of age, sex, professional, clinical presentation, superficial vein diameter and GSV diameter, was similar in both EV-RFA and HL/VS group. EV-RFA group got ecchymosis and pain significantly lower than HL/VS group. In our study, we compared inflammatory mediator in symptomatic varicose veins patient between HL/VS and EV-RFA group. We excluded patients with venous ulcer patients, connective tissue disease, autoimmune disease, cirrhosis, end stage renal disease, hematologic disease, infection and trauma because these were other causes of inflammatory response. Chronic venous ulcer appeared relate to chronic inflammatory injury secondary to many causes such as sustained venous hypertension, and extravasation of macromolecules and iron-containing red blood cells from the microcirculation. Bacterial contaminations are thought to secondarily affect poor wound healing [8]. Chronic venous ulcer was excluded because there were multifactorial causes of inflammation. Although preoperative level of CRP was a little higher in HL/VS group but preoperative IL-6 were not difference among 2 groups. There were significant rising of 24 h postoperative level of IL-6 and CRP in both groups especially IL- 6. EV-RFA created thermal injury; however HL/VS created more tissue trauma and inflammatory responses.
Rasmussen et al. published four-arm RCT compared results of HL/VS, EVLA, EV-RFA and foam sclerotherapy. They found that postoperative pain was significantly lower and return to normal activity time was significantly shorter in EV-RFA and foam sclerotherapy group compared to HL/VS and EVLA group. However efficiency of treatment was not significantly difference among 4 modalities [9].
Kheirelseid et al. reported meta-analysis compared results between EV-RFA, EVLA, foam sclerotherapy and conventional HL/ VS and found that there was no significant difference in recurrent rate, reintervention, neovascularization, and GSV recanalization among 4 group [10]. Rasmussen published a four arm RCT comparing HL/VS with EVLA, RFA, and foam sclerotherapy. The post-operative average pain scores at 10 days were significantly lower in the groups treated with EV-RFA and foam sclerotherapy compared with HL/VS and EVLA, with a shorter time to resumption of normal activities and work. The efficiency of the four modalities was not significantly different [9]. Common adverse effects including ecchymosis (5.8%), paresthesis (3.4%), hyperpigmentation (2.4%), erythema (2.0%), hematoma (1.4%) and phlebitis (1%). Most of complications subsided within the first week [11]. Recent studies reported incidence of thrombotic events after EV-RFA and EVLA, called endovenous heat-induced thrombosis (EHIT). Systematic review and meta-analysis reported by Healy et al. including 52 published studies, show that there was rate of DVT and pulmonary embolism (PE) was 0.3% and 0.1%, respectively [12]. Risk factors of EHIT were large vein size (11.0 +/-4.3 mm) and concomitant sclerotherapy [13].
In this study, rate of numbness was comparable to other studies (3.1% vs. 3.4%) although rate of ecchymosis was higher (9.4% vs. 5.8%) [11]. However, rate of ecchymosis, and postoperative pain were lower in EV-RFA group compared to HL/VS group. There was no DVT and PE reported in our study.
CVI is a common condition with a wide spectrum of clinical presentations. Structural and functional alterations in healthy veins lead to symptoms and signs usually seen in CVI. There was published studies described pathophysiology of CVI in last 2 decades, recently, many studies focused on the role of inflammation, and subsequent localized endothelial activation and dysfunction. There was reducing in synthesis of anti-inflammatory agents, and enhancing the expression of proinflammatory and prothrombotic molecules [12-15]. Venous reflux was thought to be the cause of venous hypertension [16]. Its consequence was the reduction of shear stress, a key regulator of endothelial activation state [16,17], which promotes pathological change of venous wall and valve [7,18,19]. Shear stresses reduce activation triggers of ECs and leukocytes; enhance expression of adhesion molecules and inflammatory cells infiltration into venous wall and leaflets. This established an environment promoted local inflammation [7,19]. Changing in normal signaling of ECs through different pathways induced production of proinflammatory mediators including IL-6, IL1, TNF-α, IFN, IL-8, MCP-1. On the other hand, endothelial cells promoted releasing of agents that stimulate thrombosis such as von Willebrand Factor (Vwf) [20], plasminogen activator inhibitor-1 [20,21], and factor VIII [21,22], as well as inflammatory cytokine such as C reactive protein (CRP) [21] and interleukin-6 (IL-6) [21]. These agents are biomarkers of endothelial dysfunction, and their levels correlated with a higher cardiovascular risk [23-24]. It was described that normal venous endothelium was able to become dysfunctional, and release prothrombotic and proinflammatory factors when exposed to increased endoluminal pressure [24]. Since CVI is a condition characterized by a sustained increasing in venous pressure, stasis or reversal of blood flow affected vessels; this may promote a prothrombotic state of endothelium. Recent study showed that releasing of prothrombotic agents from activated endothelium may explain correlation established between varicose veins and DVT [25].
This study focused on 2 inflammatory mediators, IL-6 and CRP. IL-6 was produced by monocyte, macrophages, helper T-cells, ECs, VSMCs, fibroblasts and stromal cells that effect to other cells in various functions. It effected to activated B-cell in transformation to plasma cell, and activated plasma cell in antibody secretion. It was a key role for acute phase of inflammatory response, and also effected to VSMC and endothelial cell in proliferation and proatherogenic effect [26].
The relationship of IL-6 and varicose vein had been studied by Alexander et al. [26] compared serum inflammatory biomarker levels from varicose veins and antecubital vein of varicose veins patient and from leg vein and antecubital vein of healthy controls. They found that the most relevant inflammatory biomarkers in CVI were IL-6, IL-8, and MCP-1. IL-6 concentration was significantly greater in varicose vein compare to antecubital vein and healthy controls. This suggested that IL-6 released from the leg and diluted once it went to arm. Finding that IL-6 was elevated dominantly in the legs of varicose veins patients may explained that IL-6 was not directly related to systemic response CVI and may represent normal physiological response to higher venous pressures, typically in the gaiter region. This may reflected the higher sensitivity of IL-6 to local increased venous pressure contrast to IL-8 and MCP-1. However, IL-8 and MCP-1 may be more specific for systemic inflammation in CVI. Age and disease severity were shown to correlate significantly with increases in IL-6 concentration [27].
CRP is one of the acute-phase proteins. CRP is predominantly secreted by the liver at 4-6 hours after stimulation. It duplicates every 8 hours, and peaks within 36 to 50 hours. CRP has a plasma half-life of 19 hours, and even after a single stimulus, as in a trauma or surgery, it may take several days to return to the baselines [28]. There were 3 types of CRP assays consists of Conventional CRP, High sensitivity CRP (hsCRP) and Cardiac C-Reactive Protein (cCRP). There was diversity of clinical use example hsCRP was detected lower level of CRP that bring to use for healthy individuals, cCRP was used for identify cardiovascular risk and conventional CRP assays were indicated for use for evaluation of infection, tissue injury, and inflammatory disorders. CRP assays provide information for the diagnosis, therapy, and monitoring of inflammatory diseases [29]. CRP is a more sensitive and more reliable indicator of acute inflammatory processes than the erythrocyte sedimentation rate (ESR) and leukocyte count. Blood CRP levels rise more rapidly than ESR, and after the disease has subsided CRP values rapidly fall and reach the reference interval often days before ESR has returned to normal [30,31]. Thus, CRP assays was applied to this study.
There is a correlation between increasing levels of IL-6 during inflammation and increasing levels of CRP [32], with IL-6 inducing the CRP gene [33]. CRP gene was protein from pentraxin family that encode to serum level of CRP, There were many studies that focus association of CRP gene variant to CRP level example that the minor alleles of rs1205 and rs1800947 are associated with lower CRP levels and that the minor allele of rs1130864 is associated with higher CRP levels, There were many studies that give priority association of variant type of CRP gene and many disease especially cardiovascular disease, stroke, hypertension and metabolic disease [34-36]. On the other hand, When CRP levels become elevated in atheroma, this leads to the induction of IL-6 by macrophages indicating that CRP may have a direct effect on IL-6 release [37].
CRP has half-life of 19 hours and gets peak level at 36-50 hours [38], whereas IL-6 has half-life of 2-3 hours and gets peak level at 12-18 hours [39-43]. Because half-life of CRP is longer than IL-6, 24-hr postoperative level of CRP increased less than IL- 6. However both CRP and IL-6 level significantly increased 24 hour after surgery. Selection bias is main limitation of this study. There was no randomization of patients and no well control of postoperative program. Further well designed RCT need to confirm advantage of EV-RFA compare to other modalities in aspect of inflammatory response. However cost-effectiveness of each procedure is interesting issue to be concerned.
Conclusion
EV-RFA established significantly lower postoperative pain and the lower rate of ecchymosis compared to HL/VS but the rate of numbness was comparable in both group. There was no DVT and PE reported in our study. 24-hour postoperative level of CRP and IL-6 were also increased lower in EV-RFA group compared to HL/VS group. This results evidenced the lower rate of tissue trauma after EV-RFA. A little increasing of inflammatory marker in EV-RFA group may be implied that this operation had minimal tissue trauma causing barely interfere inflammatory response of human. EV-RFA had superior both of clinical results and inflammatory response.
References
- Varaki S, Gaetano D, Gargiulo, Penkala S, Breen P (2018) Peripheral vascular disease assessment in the lower limb: A review of current and emerging non-invasive diagnostic methods. Biomed Eng Online 17-61.
- Rabe E, Pannier F (2012) Clinical, aetiological, anatomical and pathological classification (CEAP): Gold standard and limits. Phlebology 27: 114-118.
- Raffetto JD, Mannello F (2014) Pathophysiology of chronic venous disease. Int Angiol 33: 212-221.
- Atta HM (2012) Varicose veins: Role of mechanotransduction of venous hypertension. Int J Vasc Med.
- Mannello F, Ligi D, Canale M, Raffetto JD (2014) Omics profiles in chronic venous ulcer wound fluid: Innovative applications for translational medicine. Expert Rev Mol Diagn 14: 737-762.
- Satokowa H, Hoshino S, Igari T, Iwaya F, Midorikawa H (2002) The appearance of cytokines and adhesion molecules in saphenous vein valves in chronic venous insufficiency. Phlebology 16: 106-110.
- Takase S, Bergan JJ, Schonbein GS (2000) Expression of adhesion molecules and cytokines on saphenous veins in chronic venous insufficiency. Ann Vasc Surg 14: 427-435.
- Sidawy AN, Perler B (2018) Rutherford vascular surgery and endovascular therapy. Elsevier Health Sciences, USA.
- Rasmussen LH, Lawaetz M, Serup J, Bjoern L, Vennits B, et al. (2013) Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy, and surgical stripping for great saphenous varicose veins with 3-year follow-up. J Vasc Surg Venous Lymphatics 1: 349-356.
- Kheirelseid, Crowe G, Sehga R, Liakopoulos D, Bela, et al. (2018) Systematic review and meta-analysis of randomized controlled trials evaluating long-term outcomes of endovenous management of lower extremity varicose veins. J Vasc Surg Venous Lymph Disorder 6: 256-270.
- Proebstle TM, Alm J, liver Göckeritz, Wenzel C, Noppeney T, et al. (2011) European closure fast clinical study group: three-year european follow-up of endovenous radiofrequency powered segmental thermal ablation of the great saphenous vein with or without treatment of calf varicosities. J Vasc Surg 54: 146-152.
- Healy DA, Kimura S, Power D, Elhaj A, Abdeldaim Y, et al. (2018) A systematic review and meta-analysis of thrombotic events following endovenous thermal ablation of the great saphenous vein. Eur J Vasc Endovasc Surg 56: 410-424.
- Sermsathanasawadi N, Pitaksantayothin W, Puangpunngam N, Chinsakchai K, Wongwanit C, et al. (2018) Incidence, risk factors, progression, and treatment of endovenous heat-induced thrombosis class 2 or greater after endovenous radiofrequency ablation. Dermatol Surg 1-8.
- Blake GJ, Ridker PM (2001) Novel clinical markers of vascular wall inflammation. Circ Res 89: 763-771.
- Hosoi Y, Zukowski A, Kakkos SK, Nicolaides AN (2002) Ambulatory venous pressure measurements: new parameters derived from a mathematic hemodynamic model. J Vasc Surg 36: 137-142.
- Bonetti PO, Lerman LO, Lerman A (2003) Endothelial dysfunction: A marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol 23: 168-175.
- Szmitko PE, Wang CH, Weisel RD, Almeida JR, Anderson TJ, et al. (2003) New markers of inflammation and endothelial cell activation: Part I. Circulation 108: 1917-1923.
- Carrasco OF, Ranero A, Hong E, Vidrio H (2009) Endothelial function impairment in chronic venous insufficiency: effect of some cardiovascular protectant agents. Angiology 60: 763-771.
- Constans J, Conri C (2006) Circulating markers of endothelial function in cardiovascular disease. Clin Chim Acta 368: 33-47.
- Nicolaides AN (2000) Investigation of chronic venous insufficiency: a consensus statement. Circulation 102: E126-E163.
- White SJ, Hayes EM, Lehoux S, Jeremy JY, Horrevoets AJ, et al. (2011) Characterization of the differential response of endothelial cells exposed to normal and elevated laminar shear stress. J Cell Physiol 226: 2841-2848.
- Anwar MA, Shalhoub J, Lim CS, Gohel MS, Davies AH (2012) The effect of pressure-induced mechanical stretch on vascular wall dif- ferential gene expression. J Vasc Res 49: 463-478.
- Poredos P, Spirkoska A, Rucigaj T, Fareed J, Jezovnik MK (2015) Do blood constituents in varicose veins differ from the systemic blood constituents? Eur J Vasc Endovasc Surg 50: 250-256.
- Blomgren L, Johansson G, Siegbahn A, Bergqvist (2001) Coagulation and fibrinolysis in chronic venous insufficiency. Vasa 30: 184-187.
- Takase S, Schmid-Schonbein G, Bergan JJ (1999) Leukocyte activation in patients with venous insufficiency. J Vasc Surg 30: 148-156.
- Criado PR, Alavi A, Kirsner RS (2014) Elevated levels of coagulation factor VIII in patients with venous leg ulcers. Int J Low Extrem Wounds 13: 130-134.
- Nozaki T, Sugiyama S, Koga H, Sugamura K, Ohba K, et al. (2009) Significance of a multiple biomarkers strategy including endothelial dysfunction to improve risk stratification for cardiovascular events in patients at high risk for coronary heart disease. J Am Coll Cardiol 54: 601-608.
- Colombo PC, Onat D, Harxhi A, Demmer RT, Hayashi Y, et al. (2014) Peripheral venous congestion causes inflammation, neurohormonal, and endothelial cell activation. Eur Heart J 35: 448-454.
- Muller-Buhl U, Leutgeb R, Engeser P, Achankeng EN, Szecsenyi J, et al. (2012) Varicose veins are a risk factor for deep venous thrombosis in general practice patients. Vasa 41: 360-365.
- prague AH, Khali RA (2009) Inflammatory cytokines in vascular dysfunction and vascular disease. Biochem Pharmacol 78 : 539-552.
- Lattimer CR, Kalodiki E, Hoppensteadt D, Fareed J, Geroulakos G (2016) Are Inflammatory Biomarkers Increased in Varicose Vein Blood?. Clin Appl Thromb 22: 656-664.
- Mitaka C (2005) Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta 351: 17-29.
- Kind CRH, Pepys MB (1984) The role of C-reactive Protein (CRP) measurement in clinical practice. Int Med 5: 112-151.
- Dixon JS, Bird HA, Sitton NG, Pickup ME, Wright V (1984) C-reactive protein in the serial assessment of disease activity in rheumatoid arthritis. Scand J Rheum 13: 39-44.
- Gambino R (1989) C - reactive protein: an underutilized test. Lab Rep Phys 11: 41.
- Szalai AJ, van Ginkel FW, Dalrymple SA, Murray R, McGhee JR, et al. (1998) Testosterone and IL-6 requirements for human C-reactive protein gene expression in transgenic mice. J Immunol 160: 5294-5299.
- Weinhold B, Bader A, Rütehr U (1997) Interleukin-6 is necessary, but not sufficient, for induction of the human C-reactive protein gene in vivo. Biochem J 325: 617-621.
- Miller DT, Zee RY, Suk Danik J, Kozlowski P, Chasman DI, et al. (2005) Association of common CRP gene variants with CRP levels and cardiovascular events. Ann Hum Genet 69: 623-638.
- Danik SJ, Chasman DI, Cannon CP, Miller DT, Zee RY, et al. (2006) Influence of genetic variation in the C-reactive protein gene on the inflammatory response during and after acute coronary ischemia. Ann Hum Genet 70: 705-716.
- Lee CC, You NC, Song Y, Hsu YH, Manson J, et al. (2009) Relation of genetic variation in the gene coding for C-reactive protein with its plasma protein concentrations: findings from the Women’s Health Initiative Observational Cohort. Clin Chem 55: 351-360.
- Han KH, Hong KH, Park JH, Ko J, Kang DH, et al. (2004) C-reactive protein promotes monocyte chemoattractant protein-1-mediated chemotaxis through upregulating CC chemokine receptor 2 expression in human monocytes. Circulation 109: 2566-2571.
- Gerhartz C, Dittrich E, Stoyan T, Rose-John S, Yasukawa K, et al. (1994) Biosynthesis and half-life of the interleukin-6 receptor and its signal transducer gp130. Eur J Biochem 223: 265-274.
- Kuribayashi T (2018) Elimination half-lives of interleukin-6 and cytokine-induced neutrophil chemoattractant-1 synthesized in response to inflammatory stimulation in rats. Lab Anim Res 34: 80-83.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences