The fate of "Saphena"-Views into the past
W Lahl and Ulf Th Zierau
DOI10.21767/2573-4482.18.03.26
W Lahl and Ulf Th Zierau*
Founder and CEO of SAPHENION®- Surgeon, Vascular Surgeon, Phlebologist, Endovascular Specialist Artery, Endovenous Specialist Berlin/Rostock, Germany
- *Corresponding Author:
- Ulf Th Zierau
Founder and CEO of SAPHENION®- Surgeon
Vascular Surgeon, Phlebologist
Endovascular Specialist Artery
Endovenous Specialist Berlin/Rostock, Germany
E-mail: dr.zierau@yahoo.de
Received Date: November 26, 2018; Accepted Date: December 17, 2018; Published Date: December 21, 2018
Citation: Lahl W, Th Zierau U (2018) The Fate of "Saphena"-Views into the Past. 3:26.
Abstract
We will try to give an overview of the historical development of the varicose vein treatment. All You will agree after a short time with the words of Minkiewicz (1862) "Comparative studies of all surgical procedures recommended against varices" that "the quantity of some healing methods proposed in surgical and therapeutic practice against certain diseases either proves that the former have not yet been sufficiently researched or that the actual healing method is yet to be discovered. This applies to a large extent to varices and the usual "operation methods", And we will try to describe our personal way from the radical surgery to the endovenous therapy of varicose veins. We will show our ideas, our mistakes and our experiences considering the historical developement.
Keywords
History of varicose veins therapy; sclerotherapy vs. Babcock; Surgery vs. endoluminal ablation; Begin of endovenous therapy; Last century discussion stripping vs. sclerotherapy
Introduction
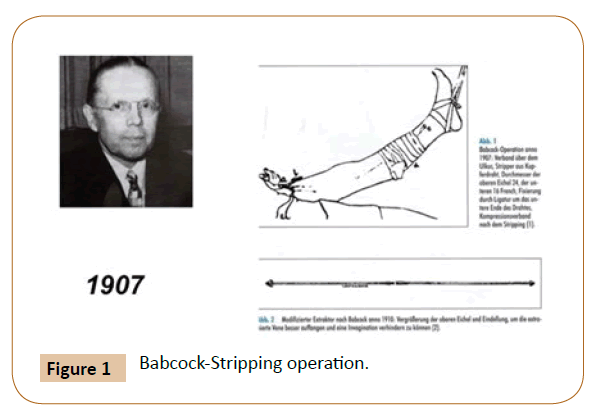
Almost exactly 50 years ago, Dr. W. Lahl entered the Surgical Clinic as a training assistant. He was immediately entrusted with the care of varicose vein patients. Also Dr. Ulf Zierau he began in his residency in 1988 at the Charitè with the radical therapy of varicose veins (Figure 1).
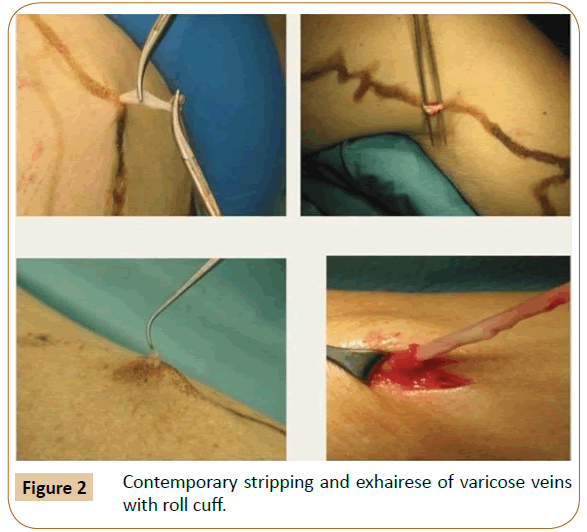
At that time, the patients were mainly treated as hospital patients. The hospital stay was approximately 7 days. The old-timers were glad that they no longer had to worry about the unspectacular clinical picture, the operations were without exception at the end of the surgery program. The boss appeared regularly in the room to ask what keeps me so long with the patient. He said "It is a disease and not cosmetics". He was most disturbed by small incisions [1]. At this time, the saying still applied "Major incisions, major surgeons, minor incisions, minor surgeons (Figure 2).
However, We have to add that the majority of patients were patients with pronounced chronic venous insufficiencies, often in combination with ulcer cruris. Cosmetic aspects were actually not in the foreground at that time. Even today, We remember the first operation reports, which were stereotypical: Skin incision hand wide below the groin, searching for the saphena and severing between ligatures. Then a button cannula was bound in and retrograde instillation of a calorose solution, a 60% invert sugar, took place. The patient lying under local anesthesia had to indicate as soon as he noticed a feeling of warmth in the ankle area. This completed the procedure and compression bandaging was performed. Ultimately, this procedure corresponded to the procedure proposed by Moszkovicz in 1927 [2].
Were We Already Pioneers of Chemical Endovenous Therapy?
Looking back, We have to ask ourself whether we were among the pioneers of chemical endovenous therapy at the time, or whether the treatment was based on an antiquated procedure. Unfortunately, revascularization of the stem vein and thrombosis due to the transfer of the high percentage solution into the deep vein system were possible complications.
We therefore dedicated ourself to the stripping procedure after a short time. The existing, approx. 60 cm (23.6 inches) long original Babcock probes were, however, only conditionally suitable. They were too rigid as well as too short and the vein material often slipped over the probe olive. At that time, we were still far away from an invaginating or stage-appropriate stripping, the exhairese up to the malleolus was the rule. Stripper probes could not be acquired in the former GDR. Necessity is the mother of invention, we obtained flexible piano sides from the Hochschule für Musik "Hanns Eisler", Berlin, and manufactured slide-on cylinders of various diameters.
Historical review
If you try to get an overview of the historical development of the varicose vein treatment, after a short time you agree with the 1862 of Minkiewicz "Comparative studies of all surgical procedures recommended against varices" [1] that "the quantity of some healing methods proposed in surgical and therapeutic practice against certain diseases either proves that the former have not yet been sufficiently researched or that the actual healing method is yet to be discovered. This applies to a large extent to varices and the usual "operation methods". In order to be able to appreciate the changes in dealing with the insufficient V. saphena, which have taken place over the course of centuries, we have to take a look back into the more distant past.
The last centuries
Descriptions and illustrations of varicose veins and their complications are already available from pre-Christian times as well as the following centuries. However, therapeutic measures consisted mostly only of relieving interferences with complications.
The basement of our knowledge of venous circulation was laid by Farbricius Aquapendente, who discovered the venous valves around 1584 and also pointed out the functional importance of these valves for venous circulation. His student William Harvey incorporated this early knowledge into his scientific concept of the entire bloodstream. Two centuries later, Tomasso Rima first described the role of Saphena magna (GSV) varicosis as a trigger of venous reflux and concluded logically that Saphena must be stopped at its junction. This demand for a radical OP was not enforceable in the 18th century [3,4].
Pro and contra saphenectomie
Only with the introduction of anaesthesia, anti- and asepsis in the middle of the 19th century you come across an almost unmanageable number of different treatment proposals to eliminate the pathologically dilated saphenous septum and the varicose side branches. For a long time though, leading surgeons generally spoke out against surgical intervention.
Johann Friedrich Dieffenbach [5], who held a chair at the Charité until his death in 1847, formulated this as follows: "These in many cases doubtful, rarely only by the urge of circumstances varicose vein surgery is performed according to the various methods that have been recommended to be easier than to protect the patient from the adverse consequences of the same".
The Lyons surgeon Charles Gabriel Pravaz injected in 1851 iron chloride solution in arteries and encouraged his students at the same time to try this method in varicose veins [4].
Theodor Billroth [3,4] also pointed out in his book in 1863 "General Surgical Pathology and Therapy."
"We have to explain ourselves incompetently in the treatment of varicose veins, because we do not know of any means that would be able to destroy the disposition to these venous diseases... If we also removed one or more of these diseased veins, other paths would soon develop. For this only reason, I reject operations that have the purpose of removing one or more varicose nodules from the lower leg. Remember that the individual varicose veins themselves make almost no complaint at all, that any operation on the veins can become life-threatening through complication with thrombosis and embolism. So, I must consider the varicose vein operation to be completely unmotivated. Nevertheless, these operations are carried out especially in France and often with fatal outcomes."
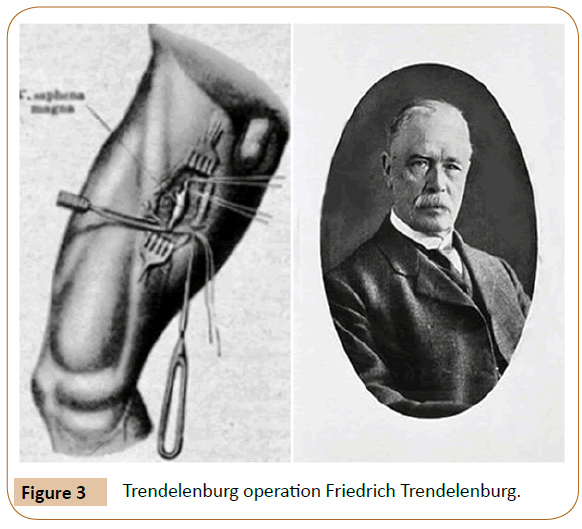
It is certainly justified to date the modern pathophysiology of venous insufficiency to Friedrich Trendelenburg (1844-1924). He introduced the concept of the "private cycle" and thus founded the solitary ligature of the saphena to eliminate reflux. In 1891 he described his procedure in Brun's contributions to clinical surgery under the title: "On the prevention of the saphenous vein magna in lower leg varicosities" [6]. At that time Trendelenburg was in Bonn, but had also worked at the University of Rostock from 1875-1882.
Neither an extirpation of the stem vein nor a crossectomy was associated with this procedure (Figure 3).
He also processed the findings of Aquapendente from the 16th century and those 100 years earlier from Rima to the ligature of the saphenous vein.
However, no extirpation of the trunk vein or crossectomy was associated with this procedure. The considerable number of recurrences prompted his former chief physician in Bonn, Georg Perthes, four years later to demand that the saphenous ligature be placed as far as possible proximally and that a saphenous segment should be resected [7].
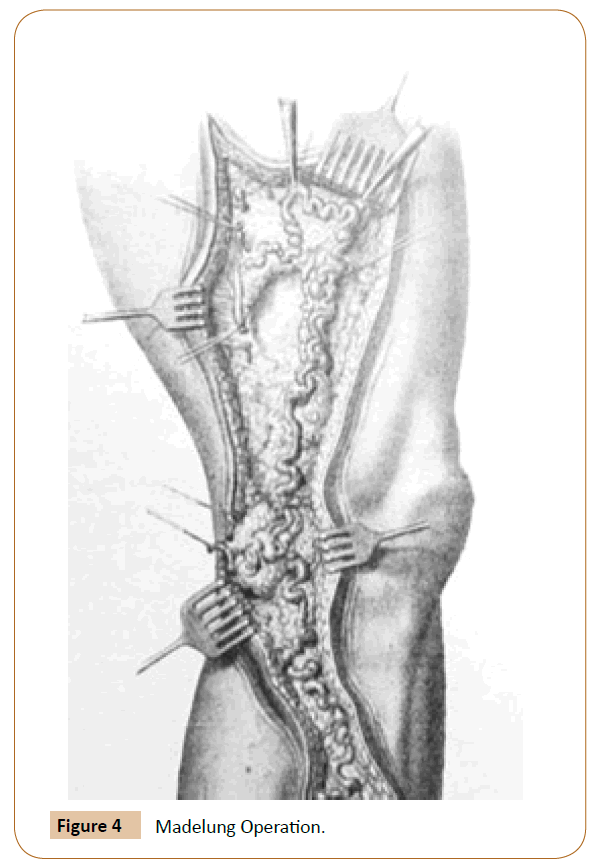
Rostock can boast of another vein pioneer. In 1884, the Ordinarius Madelung [8] presented his method at the 13th Congress of the German Society of Surgery, in which the varicose veins and perforators were extirpated from two skin incisions on the upper and lower leg as well as after back- preparation of both skin flaps in addition to the stem vein. This method was practiced well into the 20th century (Figure 4).
Also worth mentioning are the spiral incision of the Stendal surgeon Rindfleisch 1906 [9,10] and the resection of the Utrecht surgeon Narath 1908 [11], often called "finger stripping". He mobilized and removed the stem vein subcutaneously via several small skin incisions (Figure 5).
Numerous surgeons then attempted to eliminate saphena and its branches at the end of the 19th and beginning of the 20th century. Most well - known were external compressions according to Schede, Kuzmik or Kocher, spiraling beef, open deletion after Madelung and Narath resection (Figure 6) [4].
Noteworthy, because much practiced at that time, is the percutaneous incisions and ligatures of varicose veins of the Swiss surgeon Emil Theodor Kocher. Per session up to 200 (!) incisions of veins were created on one leg [12].
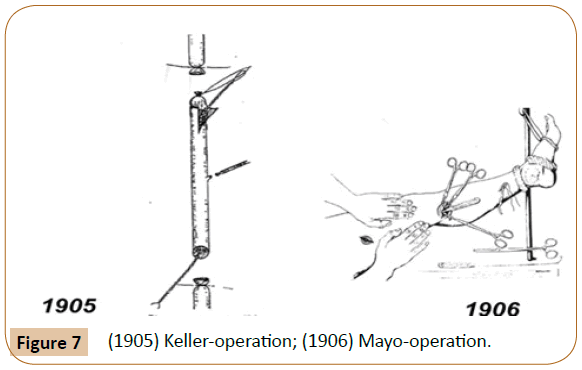
The instrumental removal of the truncal vein began with a kind of invagination of short vein segments by the American Keller in 1905 (Figure 7) [13].
In 1906, Charles Mayo succeeded in the first promising saphenous extirpation in Rochester with a ring - curette developed by him, with which he triggered the extraluminal truncal vein [14].
In 1907, William Wayne Babcock [15] was able to introduce the intravascular procedure with his stripper probe, which is still practiced today. However, the Mayo method, described in 1916 in Boston by John Homans with a combination of crossectomy, stripping and ulcer excision as radical surgery, remained the preferred method for many years [16].
The first crossectomies that meet the demands of our day are attributed to the Italians Navaro and Moro [17] of Genoa around 1910 and the Boston John Homans [16] mentioned in 1916. The French surgeon Pierre Delbet of Paris suggested in his book "Surgery arterial et veineuse" published in 1906, the transplantation of the saphenous vein in the femoral vein below the crosse at the level of the first functional venous valve. He can be considered the founder of the valve plastic. However, this procedure has not been done frequently [4].
The radicality-the complications
The radical use of Saphena and the associated complications, admittedly, led to a limited spread of the stripping method in Germany in the first half of the 20th century. There were numerous opponents who were even carried away by exaggerated statements. Let us quote the royal fountain doctor Professor Winkler from 1917 [18] "Babcock has indicated a method for cases where the dilated vein is rather straight, which surpasses everything that has been tried in this field in terms of crudeness. Before a patient gets involved in this graft, he should make his will". Dermatologists, in particular, have tried to achieve varicose veins or chronic venous insufficiency by intravascular occlusion of the saphenous septum and its lateral branches.
Begin of sclerotherapy
The actual starting point of the sclerotherapy were observations during a lues epidemic in the First World War. Both the French dermatologist Jean Sicard, as well as the German Paul Linser [19,20] made the discovery that arm veins at the injection of Salvarsan deserted. This then led to the actual sclerotherapy on the leg veins. First, both doctors injected sublimate, then hypertonic saline. The successes of Linser and Sicard, as well as Sicard's assistent Raymond Tournay brought the surgical procedures in the background, also numerous surgeons left now the operational treatment (Figure 8). The method of Moszkovicz combined at least with an operative elimination of the GSV (V. saphena magna) as well as successes of the sclerosings made with the most different medications led M. Ratschow 1931 to the following statement: "The popularization of injection therapy, the sport and the fashion of the silk stocking have caused doctors to be swamped by younger patients as well. The varicose, almost always symptom - free in the initial stage and therefore not considered, were now perceived as a cosmetic defect "[21].
Unfortunately, reports about recanalizations and critical opinions about the lack of long - term results of dermatologists became more frequent:
"Dermatologists always report on successes but rarely on long - term successes", Moszkowicz complained in 1934.
And Zeller suggested already in 1927, "to combine "the well - founded bloody surgical therapy with the conservative method that is now so much in the process of being adopted" [22].
However, many years were to pass before the surgical therapy of the insufficient saphena was again accepted by the surgeons themselves.
Differentiated therapy
In 1932, a survey showed that 11 out of 12 surgical university hospitals performed sclerotherapy! Just after the Second World War did an increasing differentiation begin between cases suitable for sclerotherapy and classical truncal varicosis.
Dr. Lahl Immediately experienced this period of departure and was able to dedicate himself to questions about the Saphena until his age-related retirement from clinical everyday life and also afterwards through work in SAPHENION Venencentrum after emeritation. It was only after the Second World War that an increasing differentiation of the cases suitable for sclerotherapy and of classical truncal varicose veins began.
The American babcock stripping process became increasingly popular.
Contributing to this were:
• The development of flexible probes
• The conscientious crossectomy
• One required in particular by Hach-operation to protect healthy saphenous segments [23-25]
• The departure of coarse release varicose side branches towards mini incisions with the appropriate instrumentation as well
• The much improved diagnostics
Unforgotten for Dr. Lahl is the statement by the Nestor of German Vascular Surgery, Prof. Vollmar, at the Surgeons' Congress in 1969 that "The claim to sole representation of the sclerotherapy experts and leg wrappers as well as that of the exclusive strippers". Nonetheless, it was an expression of the still subliminal rivalry between surgeon and dermatologist for professional competence with regard to the clinical picture. Unfortunately, the longstanding disregard of many surgeons for the value of varicose vein disease has not helped us [26].
Our own experiences
In this period of departure, Dr. Lahl was thrown into it and was able to devote himself to questions about the therapy of the GSV (Vena saphena magna) even after his age-related departure from the clinical routine by working in the SAPHENION venous centers.
A great benefit was the introduction of duplex or color Duplex sonography. Previously, we were always faced with the question of the indication for a phlebography, the decision for or against which could have legal consequences.
We do not like to say many words about the various procedures to tear poor Saphena out of the tissue. Whether ante or retrograde stripping, whether CHIVA, cryo or trivex procedures, invaginating or PIN-stripping according to Oesch, whether with or without bloodlessness etc., in the end all methods more or less injured the surrounding tissue and always contained the danger of damage to neighbouring structures.
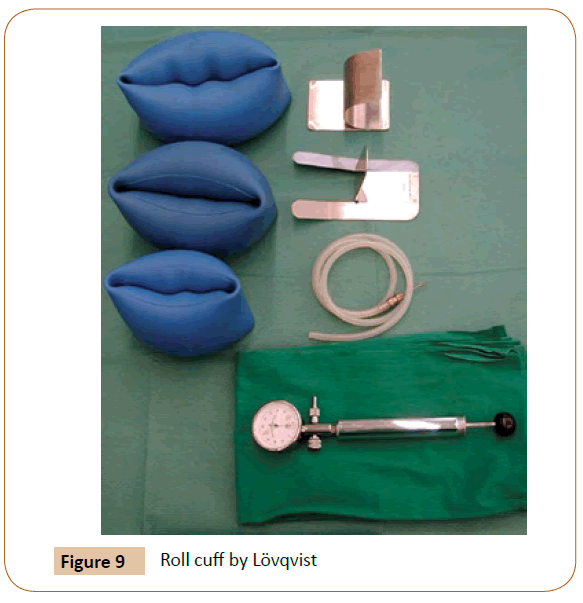
To minimize this risk, our variceal interventions have been carried out since 1995 exclusively by applying the 1988 roll cuff recommended by Lövqvist [27]. Already in 1965 Robert Fischer had used a pneumatic cuff with 550 mmHg. Because of possible nerve damage, however, she was rejected by the many practitioners. The roll cuff needed only a pressure of 120 mm Hg and led in any case to an intra - or postoperative injury. In a doctorate, one of my employees was able to prove the safety by exact measurements including blood gas analysis [28]. The bloodfree Op.feld as well as the missing postoperative hematomas were the invaluable advantage of the method (Figure 9).
Therefore, Dr. Lahl would like to touch on another area that is only given little attention in the publications of conventional varicose vein surgery.
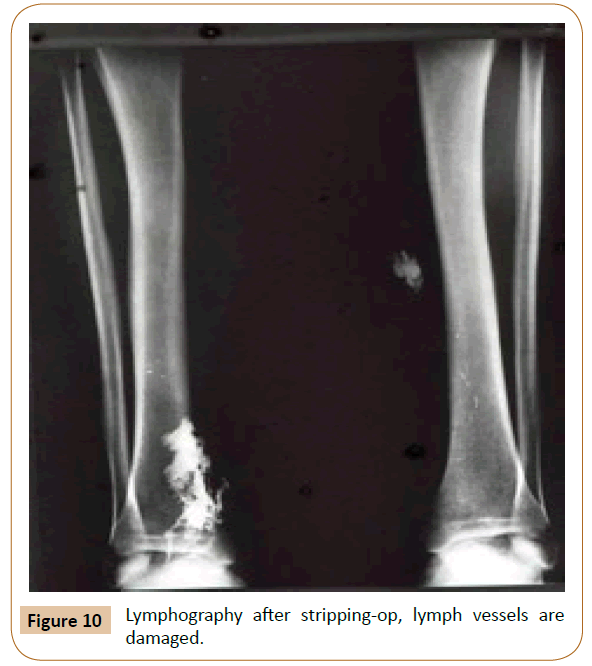
Already in the seventies, Dr. Lahl was interested in lymphological questions, especially under the aspect of iatrogenic damage after arterial reconstructions or stripping procedures. The ventromedial lymph vessel bundle runs parallel to the V. saphena magna (GSV) and is therefore directly endangered during stripping. The extent of a possible intraoperative injury was only poorly documented. At that time, lymphographies with the oily contrast medium lipoiodol were still allowed. Thus, we were able to perform postoperative examinations on selected patients, whose surprising results we also published. They showed how invasive the stripping procedure can be despite all caution and, on the other hand, they represent a not to be underestimated advantage of endovenous methods (Figure 10) [29].
We must also point out the possible nerve damage. While an injury in the saphenous region can be observed relatively frequently and is usually tolerated by the patient, it can never be safely avoided in the course of the sural nerve and is extremely unpleasant for the patient in the long term. We are not aware of any really reliable data on the frequency of suralis lesions [30].
A large repertoire of surgical instruments has been developed for the gentle handling of the saphenous tissue and the perivasal tissue. Almost every surgeon had his preferred instrument, often named after him. Despite the optimization of surgical therapy, the use of sclerosing drugs by our dermatological colleagues was unbroken. With the introduction of ultrasound-supported sclerotherapy and the use of microfoam, new possibilities arose to include not only side branch varices but also an inefficient saphena in the therapy concept.
Modern ways in treatment of varicose veins
Later, surgeons and phlebologists developed the various endovenous techniques at the beginning of the 1990s. Hence, they followed the demand of a nestor of phlebology, Urs Brunner, who already three decades ago formulated the desired treatment of Saphena as follows "Today's concept is conservative, reflux-oriented, aesthetic".
It is easy to answer the question of what led to the rapid development of endovenous forms of therapy that today replace the stripping method:
• They avoid larger wound areas, haematomas and infections
• There is a general trend towards minimally invasive surgery
• The patients demand a rapid rehabilitation, preferably without inability to work as well as optimal cosmetic results.
• Suitable technologies have been developed and modern catheter techniques also developed for phlebology
• Preferably radical approach in the conventional varicose vein surgery could not prevent the recurrence, with the actual recurrence rate after operative remediation of truncal varicose veins has not yet been clearly proven. The information on this varies between 7 and 60 per cent [31-33].
After a period of 20 years working with foam, with laser or RFA we today have a new discussion - what s better, thermal ablation or non thermal ablation? Microfoam or MOCA [34-43]? Its`s also very interesting to following the newest therapy option-sealing veins [34,36,41-43], and we have international guidelines for therapy of varicose veins [44-46]. Here we can find the new way of therapy, the new standards. Endoluminal, catheter based, minimally invasive.
We will see, how the German guidelines are beeing revised by the German Society of phlebology [47-51]. The german guidelines were updated 7 years ago and the radical surgery is playing a great role also today. We have to determine, that nearly 80% of all patients in Germany get a radical stripping-op also today (Figure 11) [47,52-58].
Conclusion
And so, through the use of the new procedures adapted to the findings, the Saphena's long path of suffering also seems to have come to an end, in which it can remain closed but without damage to the surrounding structures and for the benefit of its bearers in its traditional place.
We would like to conclude with Rudolf Klapp's statements made in 1923 and still valid today, at that time Head of the Surgical University Polyclinic in Berlin "In the case of a pains so widespread as the varices are, the operative treatment would have to be so successful that a patient who is satisfied with the operation always sends 10 others". Rudolf Klapp, 1923 [59-62].
Dr. Ulf Th. Zierau send many thanks to Dr. Wolfgang Lahl for ten years intensive collaboration with Saphenion.
References
- Minkiewicz J (1862) Vergleichende Studien über alle gegen Varices empfohlenen Operationsverfahren. Virchows Archiv 25: 193-267.
- Moszkowicz L (1927) Behandlung der Krampfadern mit Zuckerinjektionen kombiniert mit Venenligatur. Zbl Chir 54: 1732-1736.
- Billroth T (1882) Die allgemeine chirurgische Pathologie und Therapie.
- Budde W, De La Camp EB, Lang M (1958) Operationen an den Blutgefäßen. in: Bier, Braun, Kümmell: Chirurgische Operationslehre, J. A. Barth, 7. Auflage. 6: 353-358
- Dieffenbach JF (1845) Die Operative Chirurgie. Band 1, Leipzig, F. A. Brockhaus.
- Trendelenburg F (1890) Ueber die Unterbindung der Vena saphena magna bei Unterschenkelvaricen. Verlag der H. Laupp'schen Buchhandlung 7: 195-210.
- Perthes G (1895) Ueber die operation der unterschenkelvaricen nach Trendelenburg. DMW-Deutsche Medizinische Wochenschrift 21: 253-257.
- Madelung O (1884) Verh Dtsch Ges Chir. 13: 114-117.
- Meyer F (1914) Die Behandlung des varikösen Symptomenkomplexes nach Rindfleisch-Friedel und deren Erfolge. Btrg klin Chir 89: 276-289.
- Meyer FG (1924) Zur Varizenbehandlung, insbesondere nach Rindfleisch. DMW-Deutsche Medizinische Wochenschrift 50: 1410-1411.
- Narath A (1906) Über die subkutane exstirpation ektatischer Vener der unteren Extremität. Deutsche Zeitschrift für Chirurgie 83: 104-110.
- Kocher T (1916) Vereinfachung der operativen Behandlung der Varicen. Deutsche Zeitschrift für Chirurgie 138: 113-151.
- Keller WL (1905) A new method of exstirpating varicose veins of the leg. New York Med J 82: 365.
- Mayo CH (1906) Treatment of varicose veins. Surg Gynaec Obstetr. 385-388.
- Babcock WW (1907) A new operation for the extirpation of varicose veins of the leg. NY Med J 7: 153-156.
- Homans J (1916) The operative treatment of varicose veins and ulcers, based upon a classification of these lesions. Surg Gynecol Obstet 22: 143.
- Moro G (1910) Über die Pathogenese und die zweckmäßigste Behandlung der Krampfadern der unteren Extremitäten. Beitr Klin Chir 71: 420-435.
- Hohlbaum GG (1998) Pathogenetische Theorien und chirurgische Therapie der Varizen im 19. und 20. Jahrhundert. Phlebologie 27: 138-146.
- Linser P, Schneider W, Vohwinkel KH (1955) Moderne therapie der varicen, hämorrhoiden und varicocele. Enke.
- der Molen Van HR (1981) The development of phlebology in the last 30 years. Phlebol 34: 313-332.
- Ratschow M (1931) Über die Kausale Genese der Varicenkrankheit. Klinische Wochenschrift 10: 2226-2228.
- Zeller A Zur Behandlung der Varizen (1927) Jahreskalender Ärztl. Fortb 18: 1-9.
- Hach W, Hach-Wunderle V (2013) Die Rezirkulationskreise der primären Varikose: pathophysiologische Grundlagen zur chirurgischen Therapie. Springer-Verlag, USA.
- Hach W (2001) Gefäßchirurgie. 7: 111-118.
- Hach W, Hach-Wunderle V (2008) One hundred years of Babcock's stripping. Phlebol 37: 55-60.
- Vollmar J (1969) Langenbecks Arch Chir. 325: 669-672.
- Lövqvist J (1988) Chirurg. 59: 853-854.
- Lehmann GM (2003) Die Werwendung der Löfqvistschen Rollmanschette bei der minimalinvasiven Varizenchirurgie Auswirkungen auf Herzkreislaufparameter, den Säure/Basenhaushalt und Blutgase.
- Lahl W (1974) Dt Gesundh. Wesen 34: 2184-2189.
- Sam RC, Silverman SH, Bradbury AW (2004) Nerve injuries and varicose vein surgery. Eur J Vasc Endovasc Surg 27: 113-120.
- Dwerryhouse S, Davies B, Harradine K, Earnshaw JJ (1999) Stripping the long saphenous vein reduces the rate of reoperation for recurrent varicose veins: five-year results of a randomized trial. J Vasc Surg 29: 589-592.
- Fischer R, Linde N, Duff C, Jeanneret C, Seeber P (2000) The cochlear recurrence-a follow-up after 34 years. Phlebol 29: 17-22.
- Fischer R, Linde N, Duff C, Jeanneret C, Chandler JG, et al. (2001) Late recurrent saphenofemoral junction reflux after ligation and stripping of the greater saphenous vein. J Vasc Surg 34: 236-240.
- Almeida JI, Javier JJ, Mackay EG, Bautista C, Cher DJ, et al. (2017) Thirty-sixth-month follow-up of first-in-human use of cyanoacrylate adhesive for treatment of saphenous vein incompetence. J Vasc Surg 5: 658-666.
- Fleck K (2018) Bye bye Stripping: Zur Behandlung von Varizen ist der Katheter oft die bessere Wahl. medscape.
- Gibson K, Minjarez R, Gunderson K, Ferris B (2018) Need for adjunctive procedures following cyanoacrylate closure of incompetent great, small and accessory saphenous veins without the use of postprocedure compression: Three-month data from a postmarket evaluation of the VenaSeal System (the WAVES Study). Phlebology.
- Goode SD, Chowdhury A, Crockett M, Beech A, Simpson R, et al. (2010) Laser and Radiofrequency Ablation Study (LARA study): A Randomised Study Comparing Radiofrequency Ablation and Endovenous Laser Ablation (810nm). Eur J Vasc Endovascular Surg 40: 246-253.
- Hamann SA, Giang J, De Maeseneer MG, Nijsten TE, van den Bos RR (2017) Five Year Results of Great Saphenous Vein Treatment: A Meta-analysis. Eur J Vasc Endovasc Surg 54: 760-770
- Lahl W, Zierau U (2008) Laserbehandlung bei Varikosis. Technik und Ergebnisse. Chirurgische Praxis 69: 267-268.
- Lawaetz M, Serup J, Lawaetz B, Bjoern L, Blemings A, et al. (2017) Comparison of endovenous ablation techniques, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Extended 5-year follow-up of a RCT. J Vasc Surg Venous Lymp Disorders 5: 907-908.
- Park I (2017) Initial Outcomes of Cyanoacrylate Closure, VenaSeal System, for the Treatment of the Incompetent Great and Small Saphenous Veins. Vasc Endovasc Surg 51: 545-549.
- Proebstle T, van den Bos R (2017) Endovenous ablation of refluxing saphenous and perforating veins. Vasa 46: 159-166.
- Tekin AI, Tuncer ON, Memetoğlu ME, Arslan Ü, Öztekin A, et al. (2016) Nonthermal, nontumescent endovenous treatment of varicose veins. Ann Vasc Surg 36: 231-235.
- https://www.phlebology.org/member-resources/clinical-guidelines
- Wittens CDAH, Davies AH, Bækgaard N, Broholm R, Cavezzi A, et al. (2015) Editor's choice-management of chronic venous disease: clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 49: 678-737.
- https://www.nice.org.uk/guidance/cg168
- https://www.phlebology.de/leitlinien-der-dgp-mainmenu/280-leitlinie-zur-diagnostik-und-therapie-der-krampfadererkrankung#kap10_3
- Klapp R (1924) Über Krampfaderbehandlung. Klin Wschr. 3: 156-158.
- Klapp R (1930) Fortschritte in der Behandlung der Krampfadern. Fortschr Therap 39-42.
- https://www.saphenion.de/news/arbeiten-rostocker-chirurgen%20-%20in-der-geschichte-der-gefaesschirurgie/
- Zierau UT (1995) Die Geschichte der Gefäßchirurgie in Berlin. vasa.
- Boros MJ, O'brien SP, McLaren JT, Collins JT (2008) High ligation of the saphenofemoral junction in endovenous obliteration of varicose veins. Vasc Endovasc Surg 42: 235-238.
- Almeida JI (2009) Recovery Trial-Final Results. J Vasc Interv Radiol
- Almeida JI (2007) Current state of endovenous ablation. Endovasc Today 6: 73-76.
- Almeida JI (2006) Options for treating the saphenous vein. Endovascular Today 3: 36-39.
- Mackay EG, Almeida JI, Raines JK (2006) Saphenous vein ablation. Endovasc Today 45-48.
- Paravastu SCV, Horne M, Dodd PDF (2016) Endovenous ablation therapy (laser or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins. The Cochrane Library.
- Timperman PE (2005) Prospective evaluation of higher energy great saphenous vein endovenous laser treatment. J Vasc Interven Rad 16: 791-794.
- Negus D (1993) Recurrent varicose veins: a national problem. British J Surg 80: 823-824.
- Schadeck M (2017) Sclerotherapy of varicose veins. Phlebol 46: 55-59.
- Schede M (1877) Klin. Wochenschr.14: 85-89.
- Stemmer Robert (1988) Die Varizenverödung. Ganzonie & Cie AG.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences