Treatment of Abdominal Aortic Endograft Infolding
Martijn van Dorp, Wilhelmina HJ van Vierssen Trip, Herman Rijna, Leonard J van Boven, Abraham Rijbroek and Erik GJ Vermeulen
DOI10.21767/2573-4482.100052
Martijn van Dorp1*, Wilhelmina HJ van Vierssen Trip1, Herman Rijna1, Leonard J van Boven2, Abraham Rijbroek1 and Erik GJ Vermeulen1
1Department of Vascular Surgery, Spaarne Gasthuis Hospital, Haarlem, The Netherlands
2Department of Interventional Radiology, Spaarne Gasthuis Hospital, Haarlem, The Netherlands
- *Corresponding Author:
- Martijn van Dorp
Department of Vascular Surgery, Spaarne Gasthuis Hospital
Boerhaavelaan 22, 2035 RC Haarlem, The Netherlands.
Tel: +31615364657
E-mail: martijnvandorp@icloud.com
Received date: June 13, 2017; Accepted date: July 04, 2017; Published date: July 07, 2017
Citation: Dorp MV, Trip WHJVV, Rijna H, Boven LJV, Rijbroek A, et al. (2017) Treatment of Abdominal Aortic Endograft Infolding. J Vasc Endovasc Surg. 2:20. doi: 10.21767/2573-4482.100052
Abstract
Aortic endograft infolding is considered a rare endograft related complication and is mostly reported after deployment in the thoracic aorta. We report a case of early abdominal endograft infolding with luminal obliteration and acute bilateral limb ischemia after endovascular treatment of a common iliac aneurysm. Even though completion Computed Tomography (CT) angiography, three days prior, revealed no apparent mismatch of the stent graft to the aortic wall. This report aims to describe an overview of the different treatment modalities and focuses on the endovascular techniques for inducing re-expansion of the infolded graft and allowing for improved sealing of the endograft.
Keywords
Abdominal aneurysm; Collapse; Endograft; Endovascular aortic repair; Infolding
Introduction
The variety and extent of endograft related complications form the downside of Endovascular Aortic Repair (EVAR), these complications allow for considerable re intervention rates, with a freedom of re intervention of 65% for endovascular repair versus 86% for open repair [1,2]. Thereby, the applicability of endovascular repair for abdominal aneurysms with a hostile anatomy could be limited [3]. One of the reported endograft related complications is device infolding, characterized as collapse, and is predominantly described in thoracic aortic endografts [4]. Hereby the endoprosthesis collapses, narrowing or obliterating the lumen of the endograft, with potentially detrimental consequences.
We present a case of early, symptomatic abdominal endograft infolding in which the patient presented with severe bilateral acute limb ischemia. The patient underwent an endovascular repair and this report aims to describe the different techniques for the treatment of abdominal aortic endograft infolding.
Case Report
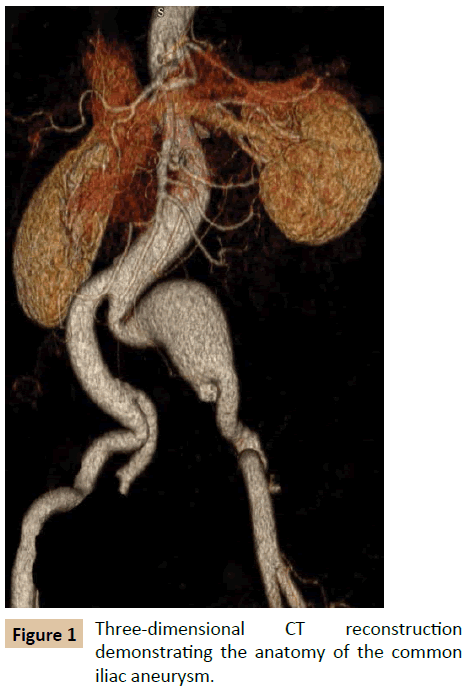
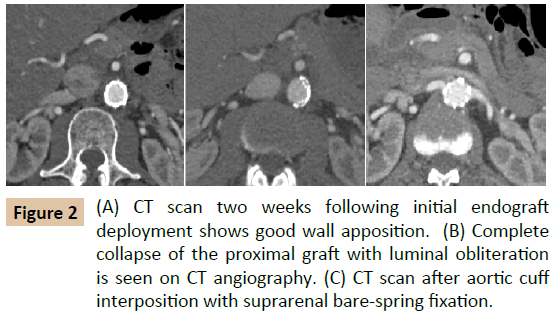
A 54-year-old male underwent elective Endovascular Aortic Repair (EVAR) with iliac-branched device (IBD) for the treatment of an aneurysm of the left common iliac artery with a diameter of 4.2 cm (Figure 1). Otherwise, the patient was healthy and led an active life. The pre interventional measurements by CT scan revealed a large aortic neck length of more than 10 cm with a straight configuration without angulation or calcifications. The distal neck diameter was 20 mm. We opted for the smallest diameter trunk, thereby allowing for 15% oversizing. Under a standard procedure, an endovascular bifurcated graft of 23 mm in main body diameter, 14 mm in iliac limb diameter and 12 cm in length was implanted (Excluder; W.L. Gore and Associates Inc., Flagstaff, Ariz) and an iliac-branched device was deployed for the perfusion of the left hypogastric artery. Balloon remodeling was performed in a standard manner. Completion angiography revealed adequate graft interposition, with exclusion of the iliac aneurysm and no signs of endoleak. The patient had an uneventful recovery and was discharged on the second postoperative day. A completion CT angiography, two weeks postoperatively, revealed accurate positioning of the endoprosthesis with correct wall apposition of the endograft (Figure 2).
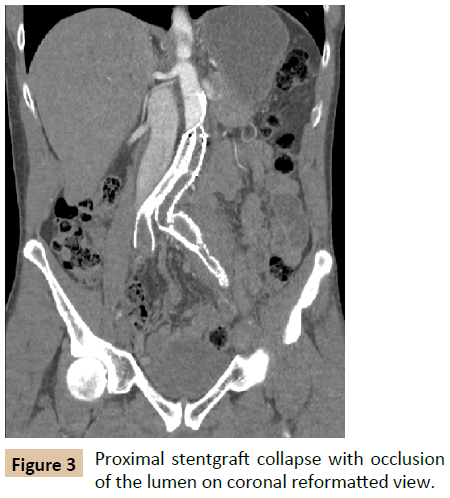
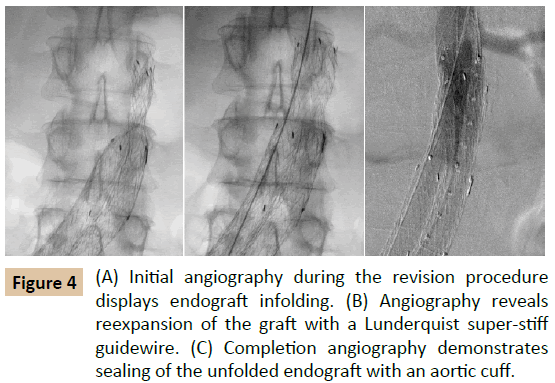
Three days later, the patient presented at the emergency department with bilateral acute limb ischemia Rutherford classification IIb, after a period of speed cycling. No palpable femoral pulses were present and patient had bilateral lower extremity motor and sensory loss. CT angiography revealed infolding of the endoprosthesis with proximal collapse of the graft with luminal obliteration (Figure 3). We opted for an endovascular repair (Figure 4). After obtaining bilateral femoral access, retrograde angiography confirmed the collapse of the endoprosthesis. We were able to pass a standard 0.035 Terumo followed by a 5 Fr pigtail through the collapsed body of the endoprosthesis. Passage of a 260 cm long, 0,035-inch diameter Lunderquist super-stiff guide wire (Cook, Winston, NC) through the pigtail catheter already resulted in unfolding and re-expanding of the endograft. If the infolding would not have been corrected by the Lunderquist, our next step would have been ballooning of the infolded part of the endoprosthesis. To fixate the proximal part of the endograft, we implanted a Medtronic proximal aortic cuff (Medtronic, Minneapolis, Minn) infrarenal with a 25 mm diameter. After ballooning, we obtained a completion angiogram displaying adequate apposition of the cuff and the endoprosthesis. The completion CT angiography two days postreintervention showed a patent endograft lumen without signs of infolding or endoleak, and a small non-flow-limiting dissection of the left external iliac artery. Initially, high levels of Creatine Kinase (CK) were present due to rhabdomyolysis, for which generous amounts of intravenous fluids were administrated. The patient was bothered by weakness of the right upper leg and impotence, however all symptoms completely disappeared after six weeks and follow-up CT angiography at one year revealed no signs of infolding and shrinkage of the iliac aneurysm.
Discussion and Conclusion
In this case, we were presented with a proximal abdominal endograft collapse after apparently sufficient primary endovascular repair for an iliac aneurysm. If infolding of endovascular prosthesis (thoracic of abdominal position) occurs, most patients present themselves with acute ischemic symptoms due to flow diminishing or obstruction. The need for emergency repair is usually at hand. Our case provides endovascular solutions and considerations to correct infolding of endovascular prosthesis.
Apart from a handful of case reports [5-8], infolding is a known complication of the thoracic aortic endoprosthesis. The recent Gore Excluder annual clinical update presented all reported events over a 16-year period and represents more than 190,000 devices distributed worldwide [9]. This review documents 27 cases of proximal trunk infolding, however does not provide specified information regarding these endograft related complications. Still much is unknown regarding the pathophysiology of endograft infolding in EVAR.
Several treatment options are available for the treatment of abdominal aortic endograft infolding. Endovascular repair is based on two stages. In the first stage, the infolded abdominal endoprosthesis has to re-expand and realign with the aortic or iliac wall. For this we used a Lunderquist super-stiff guidewire to push the collapsed proximal endoprosthesis open, however other stiff guidewires like the Amplatz (Boston Scientific, Natrick, Mass), Archer (Medtronic), or Back-up Meier (Boston Scientific) can also be used. In case of inadequate or incomplete re-expansion, or when there is narrowing of the lumen without a complete collapse of the graft, balloon angioplasty is the preferred method of re-expansion. A compliant balloon, like the Reliant balloon (Medtronic), can be used to force the endoprosthesis to unfold and realign with the aortic wall. Unfortunately, the balloon can have the propensity to slip from the collapsed site, thereby preventing graft remodeling. Support of the balloon could be obtained with a long introducer sheath or with a femoral-brachial guidewire, also known as the body floss maneuver, to obtain more stability upon dilatation [10].
In the second stage, the unfolded endograft has to be fixated or supported to the aortic wall to allow for sealing with greater radial force, to prevent recurrence. In this case, we used a Medtronic cuff with suprarenal bare-spring fixation through the Excluder endoprosthesis to increase the radial force at the renal level. Alternatively, a balloon expandable Giant Palmaz stent (Cordis Endovascular, Warren, NJ) and to a lesser extent the self-expanding Gianturco Z stent (Cook) can be placed in the proximal endograft [4]. Care has to be taken to avoid placement of the stent within the aorta to prevent injury of the aortic wall. In case of hostile neck anatomy, Endoanchors (Aptus, Sunnyvale, Calif) can increase the sealing and stabilization of the graft by penetrating the aortic wall [11]. Infolding can also present as an asymptomatic finding during standard CT surveillance, thereby possibly allowing for a more complex and delayed reconstruction by means of branched or fenestrated endovascular repair. Hereby using covered suprarenal fixation to increase the sealing of the graft and can be useful in short, conically shaped, largediameter, or highly angulated aortic neck configuration [12]. Refraining to perform the second stage of endovascular repair, in improving endograft sealing, can prove to be a crucial mistake. Balloon angioplasty as a stand-alone re-intervention in TEVAR has a 50% failure rate and should therefore be avoided [4].
In this case, we obtained bilateral femoral access using an open cut down approach, thereby being able to perform bilateral limb thrombectomy with a Fogarty catheter at the end of the procedure, although percutaneous access could have been a possibility. Due to the excruciating rest pain, we were forced to perform the procedure under general anesthesia, however in case of asymptomatic infolding treatment under local anesthesia remains possible. As an alternative to the described methods of endovascular repair, there is open conversion with aortic crossclamping and endograft explanation.
We advocate this only to be used as a bailout procedure. In this case, we were presented with a proximal abdominal endograft collapse despite favorable neck anatomy, lack of excessive oversizing, absence of angulation and a well-anchored aspect of the concomitant iliac-branched device. A possible arched posture of the back during cycling could have facilitated a posturedependent type Ia endoleak, however more research is needed regarding the significance of intermittent posture-dependent endoleaks [13]. As documented by the adequate endograft wall apposition three days prior to the collapse, endograft infolding was not likely to be caused by intra procedural graft malexpansion and can be seen as an instant event. In this case, we can only speculate on the cause(s). If a posture dependent type Ia endoleak did exist, we might have to take into consideration, that we did not choose the right size of endoprosthesis. However, the next available size endograft would have exceeded 20% oversizing. Another aspect might be the fact that the endoprosthesis was positioned 1-1.5 cm below the renal arteries in a not dilated abdominal aorta. Whether or not this promotes posture dependent endoleak in conjunction with or without (in) adequate oversizing of the endoprosthesis remains also unclear. Despite the severity of this endograft related complication, the (endo) vascular surgeon is provided with a broad armamentarium to deal with abdominal endograft infolding.
References
- The United Kingdom EVAR Trial Investigators (2010) Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med 362: 1863-1871.
- Van Schaik TG, De Bruin J, Van Sambeek M, Verhagen H, Prinssen M, et al. (2016) Very long-term follow-up (12-15 years) of the Dutch randomized endovascular aneurysm repair management (DREAM) trial. J Vasc Surg 63.
- Sweet MP, Fillinger MF, Morrison TM, Abel D (2011) The influence of gender and aortic aneurysm size on eligibility for endovascular abdominal aortic aneurysm repair. J Vasc Surg 54: 931-937.
- Kasirajan K, Dake MD, Lumsden A, Bavaria J, Makaroun MS (2012) Incidence and outcomes after infolding or collapse of thoracic stent grafts. J Vasc Surg 55: 652-658.
- Matsagas MI, Papakostas JC, Arnaoutoglou HM, Michalis LK (2009) Abdominal aortic endograft proximal collapse: successful repair by endovascular means. J Vasc Surg 49: 1316-1318.
- Sfyroeras GS, Maras D, Andrikopoulos V (2011) Abdominal endograft collapse with acute bilateral lower limb ischemia. J Vasc Interv Radiol 22: 570-572.
- Loh SA, Jacobowiz GR, Rockman CB, Veith FJ, Cayne NS (2010) Endovascular repair of a collapsed abdominal aortic endograft due to bird-beaking. J Vasc Surg 52: 813-814.
- McCready RA, Bryant MA, Divelbiss JL, Philips JL (2009) Complete endograft collapse 9½ years following endograft repair of an abdominal aortic aneurysm. Vasc Endovasc Surg 43: 627-630.
- Gore Excluder AAA Endoprosthesis (2014) Annual clinical update.
- Kotelis D, Lopez-Benitez R, von Tengg-Kobligk H, Geisbusch P, Bockler D (2008) Endovascular repair of stent graft collapse by stent-protected angioplasty using femoral-brachial guidewire. J Vasc Surg 48: 1609-1612.
- Jordan WD, Mehta M, Varnagy D, Moore WM, Arko FR, et al. (2014) Results of the ANCHOR prospective, multicenter registry of EndoAnchors for type Ia endoleaks and endograft migration in patients with challenging anatomy. J Vasc Surg 60: 885-892.
- Eagleton MJ, Follansbee M, Wolski K, Mastracci T, Kuramochi Y (2016) Fenestrated and branched endovascular aneurysm repair outcomes for type II and III thoracoabdominal aortic aneurysms. J Vasc Surg 63: 930-942.
- May J, Harris JP (2012) Intermittent, posture-dependent, and late endoleaks after endovascular aortic aneurysm repair. Semin Vasc Surg 25: 167-173.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences