A COVID-19 Case Complicated by Acute Pulmonary Embolism Underwent EKOS Thrombolysis with Favorable Outcome
Lifen Cao, John Liuzzo, Anjali Ratnathicam, Massimo Napolitano, Gregory Simonian and David O’Connor
DOI10.21767/2573-4482.20.05.28
1Department of Vascular and Endovascular Surgery, Hackensack University Medical Center, Hackensack, US
2Department of Cardiology, Hackensack University Medical Center, Hackensack, US
- *Corresponding Author:
- David O’Connor
Department of Vascular and Endovascular Surgery
Hackensack University Medical Center, Hackensack, US
E-mail: David.Oconnor@hackensackmeridian.org
Received Date: November 06, 2020; Accepted Date: November 18, 2020; Published Date: November 25, 2020
Citation: CLifen C, John L, Anjali R, Massimo N, Gregory S, David O (2020) A COVID-19 Case Complicated by Acute Pulmonary Embolism Underwent EKOS Thrombolysis with Favorable Outcome. J Vasc Endovasc Ther. 5 No. 5: 28.
Abstract
We report a case of a 53 year-old man who presented with simultaneous COVID-19 infection and acute saddle pulmonary embolus with right heart strain. He underwent bilateral pulmonary artery ultrasound accelerated (EKOS) thrombolysis with successful resolution of pulmonary artery thrombus.His respiratory status significantly improved and follow-up echocardiography demonstrated normalization of right ventricular function and size.In the setting of critically ill COVID-19 patients who demonstrates respiratory deterioration with other clinical evidence of venous thrombosis, pulmonary embolism and subsequent ultrasound assisted catheter-directed thrombolysis (USAT) may be considered.
Keywords
COVID-19; Deep venous thrombosis; Pulmonary embolism; EKOS thrombolysis; Ultrasound assisted catheter-directed thrombolysis (USAT)
Introduction
Coronaviruses are important pathogens in humans and animals. First identified in Wuhan, the novel coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), rapidly spread resulting a pandemic worldwide [1]. The disease caused by SARSCov- 2 is designated the coronavirus disease 2019 (COVID-19). The spectrum of symptomatic SARS-Cov-2 infection ranges from mild to critical. Most COVID-19 infections, however, are not severe. Serious illness predominantly occurs in adults with advance age or underlying medical comorbidities including cardiovascular disease, diabetes mellitus, hypertension, chronic lung disease, cancer, chronic kidney disease, liver disease, severe morbid obesity (body mass index >40) and immunocompromising conditions [2]. While pneumonia appears to be the most frequent serious manifestation of this infection, it is still an evolving process in understanding the course and complications of COVID-19.
Acute pulmonary embolism may develop in patients with mycoplasma pneumonia due to acquired prothrombotic factors [3] and in patients with severe influenza [4]. Xie et al. [5] reported two COVID-19 cases complicated by acute pulmonary embolism, here we reported a case with COVID-19 who developed acute pulmonary embolism and underwent USAT which showed favorable outcome. The patient’s agreement to publish the case details and images was obtained.
Case Report
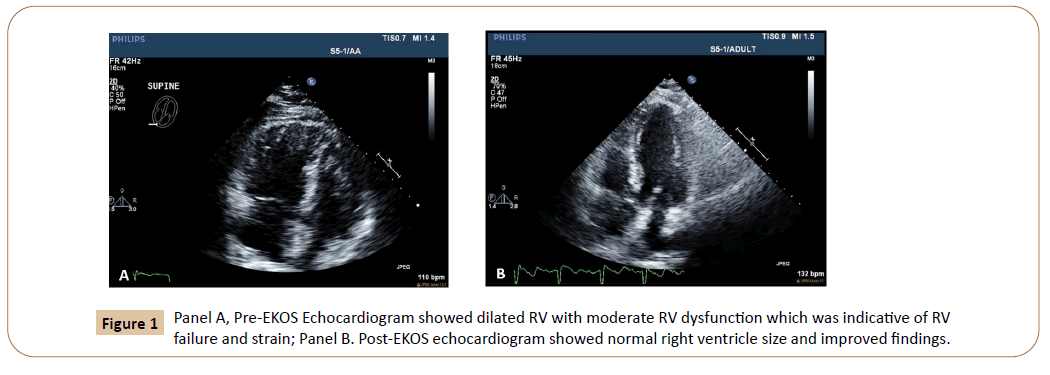
We report a 53 y.o. male with past medical histories of hypertension, Diabetes Mellitus type 2, hyperlipidemia, Stage III chronic kidney disease and obstructive sleep apnea on CPAP who presented to the emergency room on 04/01/2020 with worsening chest pain for 1 day accompanied by shortness of breath, persistent fever and non-productive cough. The patient works as a salesman in New York. He denies any recent travel or any sick contacts. An electrocardiogram was performed on presentation and demonstrated sinus tachycardia and a right bundle branch block. Due to these findings a transthoracic echocardiogram was soon ordered showing normal left ventricular systolic function, but a dilated right ventriclewith moderate dysfunctionindicative of failure and strain (Figure 1). There pulmonary artery pressures were also significantly elevated.
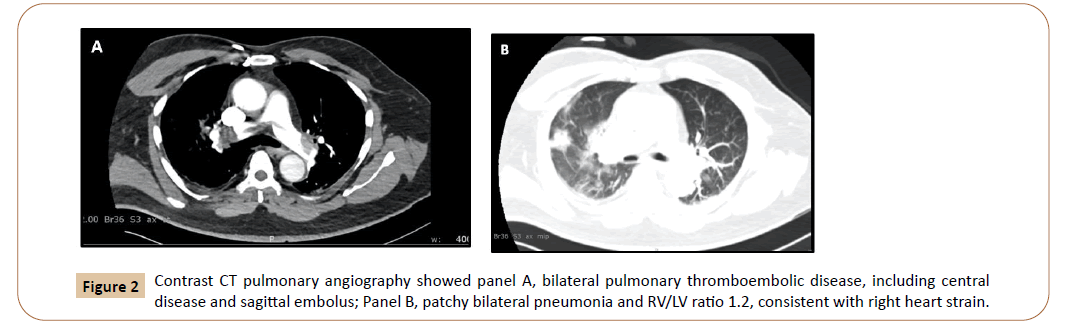
His initial chest x-ray showed a focal area of patchy consolidation within the right midlung, concerning for an infectious process. Novel Coronavirus 19 by RT PCR-nasal test came back positive on the same day. Venous dopplers lower extremity 4/1/2020 showed that Left Lower Extremity was positive for acute deep venous thrombosis with dilatedmid to distal femoral vein occluded with echo-lucent thrombus shown no venous return. Intravenous heparin anticoagulation was started with a presumed diagnosis of saddle pulmonary embolus. He was alsogiven azithromycin, doxycycline, and hydroxychloroquine during his hospital course.Computed tomography with intravenous contrast of the chest was initially delayed due to renal insufficiency, and was subsequently obtained after intravenoushydration and renal function improvement on 04/03/2020.Anacutesaddle pulmonary embolus with an RV/LV ratio of 1:2 and bilateral pulmonary infiltrates were noted (Figure 2). At this timehe continued to have tachypnea, oxygen saturations in the low 90’s and need for high dose supplemental oxygen.
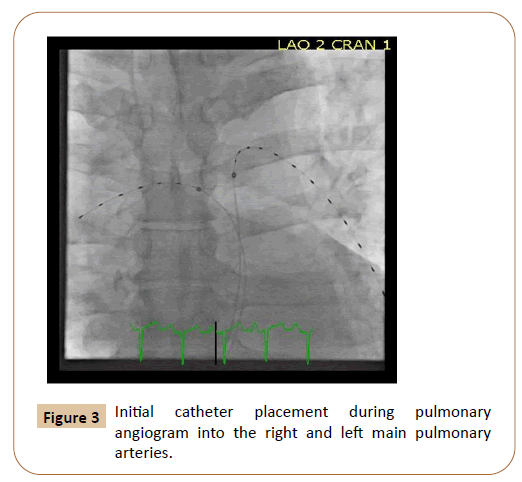
Vascular consultation was subsequently requested and the patient was brought urgently to the cardiac cath lab on 04/03/2020 for catheter-directed pulmonary artery intervention given his respiratory symptoms and right heart strain.Under local anesthesia, percutaneousbilateral common femoral vein access was obtained and an Option Elite (Argon Medical, Frisco,Tx) IVC filter was first inserted in the infrarenal vena cava.The right and left main pulmonary arteries werecannulated with aGlidewire and Glidecatheter (Terumo Medical, Somerset, NJ).After confirmatory pulmonary angiography, insertion of bilateral pulmonary artery EKOS (Boston Scientific, Maple Grove, MN) thrombolysis catheters was performed (Figure 3). Once secured in place, ultrasound accelerated thrombolysis was performed by administering 1mg of tPA per hour through each catheter for twenty fourhours. Duringthis time the patient was observed in the intensive care unit with serial measurement serum measurements of fibrinogen, coagulation, and hemoglobin levels.
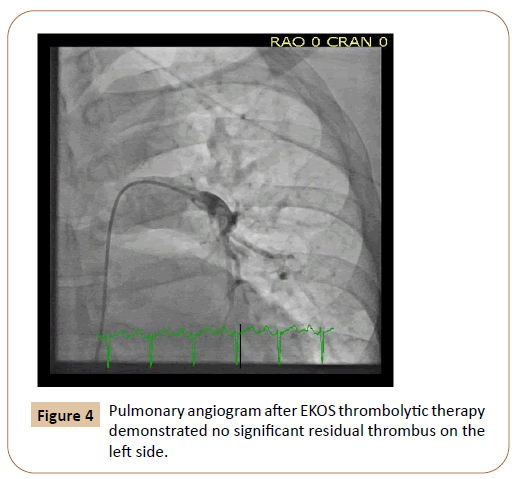
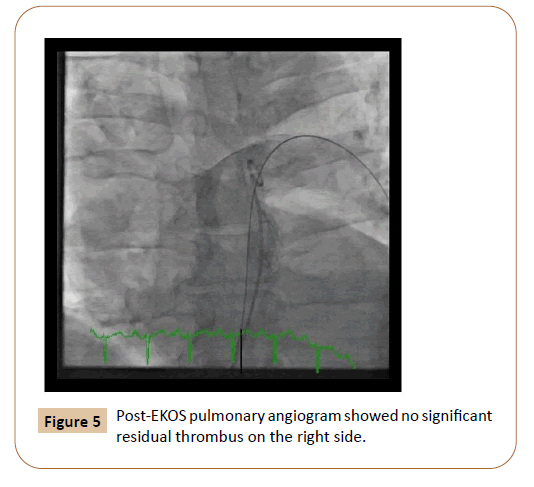
On 04/04/2020, the patient returned to the cardiac catheterization laboratory for exchange of the femoral sheaths and EKOS thrombolysis catheters and follow-up pulmonary angiography. Imaging demonstrated complete resolution of the pulmonary embolus (Figure 4), andall wires and sheaths were subsequently removed.Intravenous heparin was started immediately after the procedure and the patient’s respiratory status subsequently improved to allow transfer out of the intensive care unit later in the day. Anticoagulation was converted to apixaban on 04/05/2020 to be continued for a six-month course, and a follow up echocardiogram 04/06/2020 showed normal Left Ventricular Ejection Fraction (LVEF) normal Right Ventricular Ejection Fraction (RVEF), normal RV size and improved findings (Figure 1). The patient was subsequently discharged home on 04/07/2020 without the need for supplemental oxygen.
Discussion
A high incidence of deep vein thrombosis and acute pulmonary thromboembolism has been reported in patients with virus infection like influenza [4,6] The development of severe vascular events in influenza has been attributed, in part, to a heightened innate immune response, which include platelet-endothelial activation, loss of barrier function and consequent microvascular leak as the mechanistic roles [7].
With COVID-19, as a new coronavirus infection, there is still limited knowledge about the pathogenesis of this disease.The virus causing COVID-19 infection, SARS-Cov2, is an enveloped virus with non-segmented, single stranded, positive-sense RNA genome [8]. After ligand binding to angiotensin-converting enzyme 2 (ACE2) protein, which is highly expressed in lung alveolar cells and also serves a role in lung protection, SARS-Cov2 enters cells via receptor-mediated endocytosis in a manner akin to human immunodeficiency virus (HIV) [9]. COVID-19 patients are likely at increased risk of venous thromboembolism (VTE) [10]. Although most evidence is preliminary, there are reports showing that abnormal coagulation parameters in hospitalized patients with severe COVID-19 disease, presented as significantly elevated D-dimer levels and higher fibrin degradation products (FDP) [11,12]. Vascular inflammation may also contribute to the hypercoagulability and endothelial dysfunction in the course of COVID-19 [10].
Here we reported a COVID-19 case complicated by acute pulmonary embolism underwent USAT with excellent outcome. The catheter-directed thrombolytic therapy has been examined in several trials for patients with acute pulmonary embolism. In the ULTIMA trial, patients with intermediate-high risk pulmonary embolism, which was defined as PE of the main or lower lobe pulmonary artery and echocardiographic evidence of RV enlargement (RV/LV ratio > 1), were randomized to USAT followed by intravenous heparin or to intravenous heparin alone. Compared with conventional anticoagulation, USAT supported a hemodynamic benefit with a statistically significantly improved RV/LV ratio [13]. In a single-arm prospective trial of patients with massive and intermediate-high risk PE, USAT resulted in favorable reduction of RV/AV ratio and mean pulmonary artery systolic pressure [14] The USAT tPA doses and infusion durations were then optimized in the subsequently designed OPTALYSE trial [15].
Although the optimal thrombolytic regimen for patients hospitalized with COVID-19 related acute pulmonary embolism is still unknown, the USAT showed great outcome in our COVID-19 patient. Contemporary guideline endorsed strategies will be continuously observed.
Conclusion
We reported a case of COVID-19 complicated by severe vascular events. In the setting of critically ill COVID-19 patients who demonstrates respiratory deterioration with other clinical evidence of venous thrombosis, pulmonary embolism should be considered.
Conflict of Interest
none
References
- https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- Chan JF, Yuan S, Kok KH, To KK, Chu H, et al. (2020) A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395:514-523.
- Brown SM, Padley S, Bush A, Cummins D, Davidson S, et al. (2008) Mycoplasma pneumonia and pulmonary embolism in a child due to acquired prothrombotic factors. Pediatr Pulmonol 43: 200-202.
- Ishiguro T, Matsuo K, Fujii S, Takayanagi N (2019) Acute thrombotic vascular events complicatinginfluenza-associated pneumonia. Respir Med Case Rep 28: 100884.
- Xie Y, Wang X, Yang P, Zhang S (2020) COVID-19 Complicated by acute pulmonary embolism. Radiol: Cardiothorac Imaging 2: e200067.
- Ishiguro T, Kagiyama N, Uozumi R, Odashima K, Takaku Y, et al. (2017) Clinical characteristics of influenza-associated pneumonia of adults: clinical features and factors contributing to severity and mortality. Yale J Biol Med 90: 165-181.
- Armstrong SM, Darwish I, Lee WL (2013) Endothelial activation and dysfunction in the pathogenesis of influenza a virus infection. Virulence 4: 537-542.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506.
- Wang H, Yang P, Liu K, Guo F, Zhang Y, et al. (2008) SARS coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Res 18: 290-301.
- Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, et al. (2020) Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol 75: 2352-2371.
- Tang N, Li D, Wang X, Sun Z (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18: 844-847.
- Fan BE, Chong VCL, Chan SSW, Lim GH, Lim KGE, et al. (2020) Hematologic parameters in patients with COVID-19 infection. Am J Hematol 95: E131-E134.
- Kucher N, Boekstegers P, Muller OJ, Kupatt C, Beyer-Westendorf J, et al. (2014) Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 129: 479-486.
- Piazza G, Hohlfelder B, Jaff MR, Ouriel K, Engelhardt TC, et al. (2015) A prospective, single-arm, multicenter trial of ultrasound-facilitated, catheter-directed, low-dose fibrinolysis for acute massive and submassive pulmonary embolism: the SEATTLE II study. JACC Cardiovasc Interv 8: 1382-1392.
- Tapson VF, Sterling K, Jones N, Elder M, Tripathy U, et al. (2018) A randomized trial of the optimum duration of acoustic pulse thrombolysis procedure in acute intermediate-risk pulmonary embolism: the OPTALYSE PE trial. JACC Cardiovasc Interv 11: 1401-1410.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences