Anatomical Variations of the Sapheno-Femoral Junction and its Role in Early Recurrence after Laser Ablation of Vena Saphena Magna
Draganov T, Zhelev G, Nikolov G, Lozev I and Zahariev T
DOI10.21767/2573-4482.19.04.8
1Vascular Surgery Clinic, UMBAL Deva Maria General University Hospital, Burgas, Bulgaria
2General, Abdominal, and Vascular Surgery Clinic, Medical Institute of the Ministry of Internal Affairs, Sofia, Bulgaria
3Vascular and Angiology Surgery Clinic UMBAL St. Ekaterina General University Hospital, Sofia, Bulgaria
- Corresponding Author:
- Todor Draganov
Vascular Surgery Clinic, UMBAL Deva Maria General University Hospital
Alexander Stamboliyski Street, Vetren Housing District, Bulgaria
Tel: +359888410730
E-mail: draganov.todor@gmail.com
Received date: March 13, 2019; Accepted date: March 29, 2019; Published date: April 5, 2019
Citation: Draganov T, Zhelev G, Nikolov G, Lozev I, Zahariev T (2019) Anatomical Variations of the Sapheno-Femoral Junction and its Role in Early Recurrence after Laser Ablation of Vena Saphena Magna. J Vasc Endovasc Therapy Vol.4 No.1:08.
Copyright: © 2019 Draganov T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The laser ablation of vena saphena magna/VSM/is a minimally invasive method which has become a common procedure in the treatment of varicose veins thanks to the fact that the complications reported after its application are rare and intermittent. Recurrence of varicose veins after this procedure is quite infrequent. In this discussion we will lay out our observations and results from the treatment of recurrent varicose veins after laser ablation of VSM due to variations in the anatomy of the saphenofemoral junction. We discuss the role of the high entry point of the anterior accessory saphenous vein/AASV/ along with some of the constant tributaries forming the sapheno-femoral junction/SFJ/or its autonomous drainage directly in vena femoralis/VF/in the manifestation of early recurrence of varicose veins.
Keywords
Sapheno-femoral junction; Anatomical variations; Recurrent varicose veins; Laser ablation
Introduction
Recent years have witnessed dynamic development in the minimally invasive methods used in the treatment of varicose veins. Ever since the first reports in 1989 and the results published 10 years later referring to the laser treatment of varicose veins, endovenous laser ablation has become one of the most frequently applied methods of treatment [1,2].
During the laser ablation, the patient is lying in the reverse Trendelenburg position, the vein is approached percutaneously under ultrasound control by micropuncture and a needle placed in the area below the knee or in front of the medial malleolus. Normally, the treatment is limited to the venous segment above the knee in order to avoid damaging the n. saphenus which is positioned close to the vena saphena in the lower leg. Access to the vein is gained with a mini guide and then an introducer. The laser optic fiber is introduced in the VSM with the help of the guide until it reaches the area proximal to the SFJ. The tip of the catheter is placed 1 cm below the entry point of the ESV or 2 cm distally to the SFJ. After that the patient is placed in the Trendelenburg position and the vein is emptied by elevating and compressing the limb and by introducing perivenously 100-300 ml solution for tumescent anesthesia along the course of the vein. To prepare 500 ml of this solution, we mix 445 ml of 0.9% saline solution with 50 ml of 1% lidocaine with 1:100000 epinephrine, and 5 ml of 8.4% sodium bicarbonate. The tumescent anesthesia allows contact of the venous wall with the catheter or the laser fiber to achieve therapeutic effectiveness, provides analgesia, and serves as a cooling agent around the treated vein, thus diminishing the thermal damages to the surrounding tissues, which is reflected in the reduced number of skin burns and paresthesias. Then we perform the ablation of the vein by a retrograde method to the place right above the puncture. The first 10 cm of the laser optic fiber are removed at a speed of 1 to 2 mm/s, and the rest is removed at a speed of 2 to 3 mm/s. For optimal effects of the treatment, we apply energy of 50 to 80 J/cm at 1,470 nm, diode laser. At the end of the procedure, vena saphena is visualized in order to confirm the successful obliteration and the absence of protrusion of a thrombus in the femoral vein or, if we treat the VSP, in the VP. If a patent segment is identified, it is recommended to perform another procedure.
Unfortunately, despite the advancement of the minimally invasive methods of treatment, recurrence of varicose veins remains a serious problem. The rate at which it manifests itself after correction of the venous reflux in the treatment of varicose veins varies from 13%-65% to 20%-80% three years after surgery [3,4]. Scientific literature uses different terminology to describe it which complicates even further the understanding of its etiology, pathogenesis, and its clinical manifestations. In 1998, in Paris, an international consensus group defined and adopted the REVAS classification which is consistent with the CEAP classification and aims to achieve a detailed definition of the etiology, pathogenesis, and clinical manifestations of varicose vein recurrence [5].
Varicose vein recurrence is defined as the presence of lower limb varicose veins which have been previously surgically treated due to varicosis with minimally invasive methods of treatment including laser or radiofrequency ablation, sclerotherapy, or open surgery, with or without adjuvant therapy. It refers to recurrent veins, residual veins, or new varicose veins resulting from the advancement of the condition.
There are three types of recurrent varicose veins:
The first type
It includes residual veins. These are veins that were identified during the follow-up checks one month after surgery. They were not treated during the surgery because they were not identified before the procedure or detected during the surgery or, alternatively, they may have been left untreated on purpose [6].
The second type
It includes the truly recurrent varicose veins. They were not registered during the follow-up examination one month after surgery but rather manifested themselves later in the same places that were treated during the surgical procedure [7].
The third type
It includes varicose vein recurrence includes newly formed varicose veins detected after the first month post surgery in places which were not treated during the procedure.
An attempt for an in-depth analysis of the causes of varicose vein recurrence was made by Kostas et al., who outlined four main causes for the recurrence of varicose veins after surgical treatment of varicosis [8].
• Neovascularization: Formation of small convoluted abnormal veins, most often located around the SFJ which renew the pathological reflux between the surface venous network and the VF after the endovascular or surgical treatment of the VSM. It appears to be a cause of recurrent varicose veins that is very difficult to assess and analyse. The formation of new veins out of the newly generated granulation tissue after earlier VSM stripping or ligation has been reported as the main cause in 8%-60% of the cases. The endovenous laser and radiofrequency ablation are consistently reported with a lower percentage of recurrent varicose veins as a result of neovascularization or renewal of the pathological reflux in the area of the VSM which has already been treated. The clinical symptoms may appear a couple of months or years after the treatment. The reported data varies from 22.7% to 51.7% in a five-year follow-up [9].
• Disease advancement: A natural evolvement of the already existing condition leading to the emergence of a reflux in areas that were not treated during the surgical procedure. This, unfortunately, remains a constant factor in the recurrence of varicose veins [10-13].
• A technical error resulting in the unsuccessful treatment of the venous reflux due to inadequate or poor surgical technique [14].
• A tactical error resulting in the unsuccessful treatment of the venous reflux of the VSM due to inadequate preoperative evaluation or unsuitable surgical procedure.
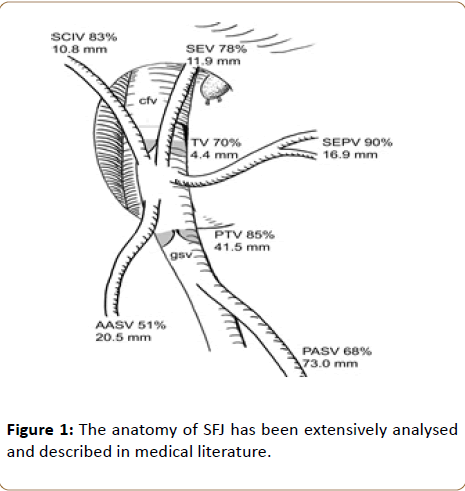
Tactical and technical errors have been reported as the leading cause in up to 80% of the cases of recurrent varicose veins [15]. These data must be subjected to serious reassessment after the introduction of the preoperative Doppler ultrasound scanning which has become a standard procedure in the clinical practice. It plays a major role in preoperative diagnostics and contributes to the significant reduction in recurrences resulting from tactical errors made during the assessment of the type and scope of the planned surgical intervention [16]. Along with procedures such as VSM stripping, phlebectomy, endovenous laser and radiofrequency ablation, and USGS, other methods, such as GHIVA and ASVAL have become common practice, relying completely on the proper evaluation of the hemodynamics and the sources of venous reflux in which the Doppler ultrasound scanning is of great help. Unfortunately, ignoring the anatomical variations of SFJ also falls in the category of the tactical errors causing early onset of recurrent varicose veins (Figure 1).
The sapheno-femoral junction has 5 significant branches which are most often situated in the femoral triangle: the superficial external pudendal vein/SEPV/and the posterior accessory saphenous vein/ PASV/.
Three lateral branches: the superficial epigastric vein/SEV/, the superficial circumflex iliac vein/SCIV/and the anterior accessory saphenous vein/AASV/.
AASV is formed by the suprapatellar system including the branches from the anterior and lateral femoral surface of the thigh. It joins directly the VSM: in 36% to 74% of the cases [17,18]. There are 8 methods of entry described-autonomous or having a common trunk with VSM or another one of its tributaries, the most common/22.1%/being the direct emptying into the VF in Asians [19]. Regardless of the fact that this frequency is significantly inconsistent with the instances reported about Anglo-Saxons, as little as 1%/Glasser 22, the existence of this anatomical variation is a fact which needs to be taken into account in the determination of the scope of the planned surgical intervention.
An important role in the functional anatomy of the lower limb vascular system is played by the terminal and the preterminal valve of the VSM, as well as the place of entry of the constant branches forming the SFJ and, in particular, the AASV. Considering the hemodynamics of the venous reflux, the high entry point of AASV-above ESV-through a common trunk with some of the constant tributaries, or autonomously in the VF above or below the SFJ, can be a cause for renewal of the venous reflux, compromising the entire surgical treatment. This is due to the fact that the laser ablation preserves the SFJ and ESV to allow the stump of the VSM to drain through it [20]. In the cases of crossectomy and stripping of the VSM, ignoring the autonomous entry of the AASV into the VF either above or below the SFJ could also result in a recurrence of the reflux and of the varicose veins.
Material and Methods
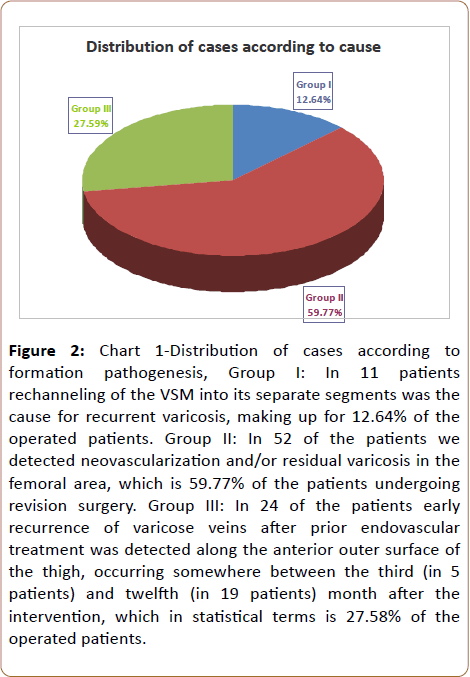
In the period from September 2016 to September 2018, 87 surgical interventions were carried out for 87 patients at the Vascular Surgery Clinic of UMBAL Deva Maria General University Hospital due to recurrence of varicose veins after laser ablation of the VSM. Of those 56 were women and 31 were men. The average age of the patients was 51 years (21 to 74 years) divided into Classes 2 to 4 under CEAP. All patients were subjected to preoperative duplex ultrasound scanning. The classifications used in the assessment were ÃÆÃÂÃâáÃÆÃÂÃâââ¬Â¢ÃÆÃÂÃâÃÂÃÆÃÂÃâàand REVAS, as well as the revised VCSS. The preoperative analysis helped in the differentiation of three groups of patients with recurrent varicose veins after endovascular laser treatment of varicosis (Figure 2 and Table 1).
Figure 2: Chart 1-Distribution of cases according to formation pathogenesis, Group I: In 11 patients rechanneling of the VSM into its separate segments was the cause for recurrent varicosis, making up for 12.64% of the operated patients. Group II: In 52 of the patients we detected neovascularization and/or residual varicosis in the femoral area, which is 59.77% of the patients undergoing revision surgery. Group III: In 24 of the patients early recurrence of varicose veins after prior endovascular treatment was detected along the anterior outer surface of the thigh, occurring somewhere between the third (in 5 patients) and twelfth (in 19 patients) month after the intervention, which in statistical terms is 27.58% of the operated patients.
| Group | Number of patients | Age | Men,% | Women,% | ÃÆÃÂÃâáÃÆÃÂÃâââ¬Â¢ÃÆÃÂÃâÃÂÃÆÃÂÃâàclassification | REVAS classification | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | S | R | N | C | |||||||||||||
| C2-C4 | C4-C6 | g | t | l | 2 | 3 | + | - | sS | dS | AK | BK | |||||
| First | 11 | 21-43 years | 36.40% | 63.60% | 10 | 1 | 0 | 8 | 3 | 3 | 8 | 9 | 2 | 10 | 1 | 8 | 3 |
| Second | 52 | 39-74 years | 34.60% | 65.40% | 48 | 4 | 12 | 39 | 1 | 41 | 11 | 47 | 5 | 37 | 15 | 41 | 11 |
| Third | 24 | 36-54 years | 29.20% | 70.80% | 23 | 1 | 1 | 18 | 5 | 15 | 9 | 24 | 0 | 23 | 1 | 23 | 1 |
Table 1: Distribution of operated patients with recurrence of varicosis.
Results
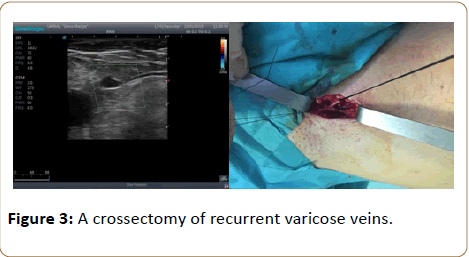
For the twenty-four patients with registered early recurrent varicosis along the anterior outer surface of the thigh, the Doppler ultrasound scan revealed insufficient varicose modification of the AASV, torqued and having a diameter of 0.5-0.7 cm. It was located in the suprafascial area along the anterior lateral surface of the thigh and it was drained into the lateral perforant of the lower leg. This required another surgical treatment, a crossectomy and phlebectomy of the recurrent varicose veins under proximal and distal control of the VF to prevent the risk of intraoperative bleeding (Figure 3).
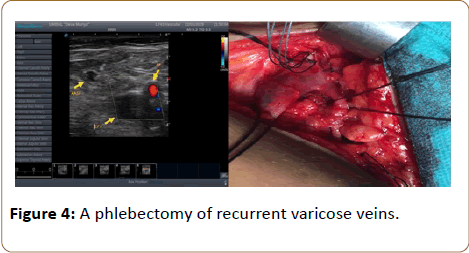
During the crossectomy, the following anatomical variations discussed above were identified in five of the patients:
In one patient: autonomous entry of the insufficient AASV directly above SFJ along the anterior lateral surface of the VF.
In four patients: high entry point of AASV through a common trunk with SEV and SCIV into the sapheno-femoral junction (Figure 4).
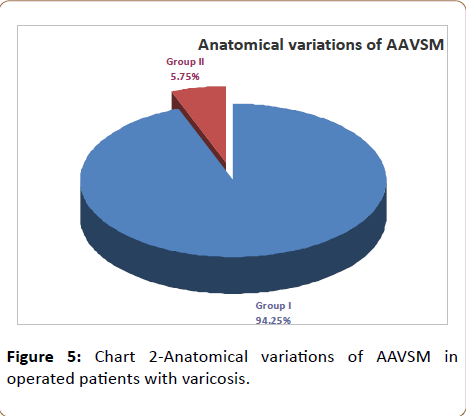
This corresponds to 5.75% of the 85 patients who underwent surgery due to recurrence of their varicose veins after the laser ablation of the VSM. The postoperative period was unproblematic for all five patients. During the control checkups at 1, 6 and 12 months, the patients had no subjective complaints (Figure 5).
The patients were examined at follow-up checks 1, 6 and 12 months after surgery. We used the revised Venous Clinical Severity Score (VCSS) to determine the severity of the chronic venous insufficiency, and in order to trace and record the results of the treatment (Table 2). In VCSS each of the ten parameters pain, varicose veins, venous flow, pigmentations, inflammation, indurations, fatigue, cramps, varicose ulcers, and application of compressive therapy was assessed from 0 to 3, with a maximum score of 30 points. Patients were divided into three groups depending on their score-light (0-10), moderate (11-20) and severe (21-30).
| Group | Number of patients | Light CVI, 78.16% | Moderate CVI, 20.69% | Severe CVI, 1.15% | |||
|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | ||
| First | 11 | 7 | 2 | 2 | 0 | 0 | 0 |
| Second | 52 | 21 | 18 | 8 | 4 | 0 | 1 |
| Third | 24 | 16 | 4 | 2 | 2 | 0 | 0 |
Table 2: Table of postoperative severity of chronic venous insufficiency.
Discussion
An important factor for the success of the endovenous laser ablation of the VSM is the complete preoperative ultrasound mapping of the vascular network of the treated limb. Failing to recognize the autonomous entry of the AASV into the VF or of its high point of entry through a common trunk along with some of the constant tributaries forming the SFJ leads to early reoccurrence of the varicose veins compromising the treatment. In four of the five patients with early recurrence of varicose veins due to the anatomical variation of the AASV discussed above, we applied crossectomy in combination with phlebectomy of the recurrent veins with good postoperative results. In the fifth case we performed a laser ablation of the AASV and phlebectomy of the recurrent varicose veins in the lower leg.
As an alternative to the revision surgery, we can point out the primary laser ablation of the VSM followed by the same procedure applied to the AASV at the same stage in case of preoperatively diagnosed anatomical variation of the SFJ.
Conclusion
The laser ablation of the VSM is a method of choice in the surgical treatment of varicose veins. The successful results at the earlier and later postoperative stages and the infrequent complications have turned it into the golden standard of treatment among the minimally invasive methods. A full preoperative ultrasound mapping of the vascular system needs to be made in connection with the affected limb. If the patient turns out to have the anatomical variation of the saphenofemoral junction described above, the application of a crossectomy combined with a subsequent laser ablation of the VSM and ÃÆÃÂÃâÃÂÃÆÃÂÃâÃÂÃÆÃÂÃâáÃÆÃÂÃâââ¬â¢ may help prevent early recurrence of the condition.
References
- Boné C (1999) Tratamiento endoluminal de las varices con laser de diodo: Estudio preliminary. Rev Patol Vasc 5: 35-46.
- Perrin MR, Labropoulos N, Leon LR Jr (2006) Presentation of the patient with recurrent varices after surgery (REVAS). J Vasc Surg 43: 327-334.
- Guarnera G, Furgiuele S, DI Paola PM, Camilli S (1995) Recurrent varicose veins and primary deep venous insufficiency: Relationship and therapeutic implications. Phlebolog 10: 98-102.
- Negus D (1993) Recurrent varicose veins: a national problem. Br J Surg 80: 823-824.
- Allaert FA, Perrin M (2006) Intra-and inter-observer reproducibility of the recurrent varicose Veins after Surgery (REVAS) classification. Eur J Vasc Endovasc Surg 32: 326-332.
- Browse NL, Burnand KG, Irvine AT, Wilson NM (1999) Disease ofthe Veins, 2nd edn. London: Arnold 191-248.
- Jones L, Braithwaite BD, Selwyn D, Cooke S, Earnshaw JJ (1996) Neovascularisation is the principal cause of varicose vein recurrence: Results of a randomised trial of stripping the long saphenous vein. Endovasc Surg 12: 442-445.
- Kostas T, Ioannou CV, Touloupakis E, Daskalaki E, Giannoukas AD, et al. (2004) Recurrent varicose veins after surgery: A new appraisal of a common and complex problem in vascular surgery. Eur J Vasc Endovasc Surg 27: 275-282.
- Merchant RF, Pichot O, Closure Study Group (2005) Long-term outcomes of endovenous radiofrequency obliteration of saphenous reflux as a treatment for superficial venous insufficiency. J Vasc Surg 42: 502-509.
- Almgren B, Eriksson I (1990) Vascular incompetence in superficial, deep and perforator veins of limbs with varicose veins. Acta Chirurgia Scandinavia 156: 69-74.
- Almgren B, Eriksson I (1989) Primary deep venous incompetence in limbs with varicose veins. Acta Chirurgia Scandinavia 155: 455-460.
- Puglisi R, Tacconi A, Sanfilippo S (1989) L’application du laser ND-YAG dans le traitment du syndrome variquex. In: Proceedings of the 10th World Congress of Phlebologie: Strasbourg, 25-29 September. Paris: John Libbey Eurotext; 1992. p. 677-679
- van Rij AM, Jiang P, Solomon C, Christie RA, Hill GB, et al. (2003) Recurrence after varicose vein surgery: A prospective long-term clinical study with duplex ultrasound scanning and air plethysmography. J Vasc Surg 38: 935–943.
- Myung-Hoon, Chun MD, Seung Ho, Han MD, chung JW, et al. (1992) Anatomical observation on draining patternsof safenous tributaries in korean adults 1: 25-33.
- Lozev I (2008) Impact of preoperative and intraoperative triplex ultrasound scanning on the results of the surgery for chronic vascular insufficiency of the lower limbs. Doctoral dissertation 1-206.
- Daseler EH, Anson BJ, Reimann AF, Beaton LE (1946) The Saphenous tributaries and related structures in relation to the technique of high ligation. Surg Gyn Obst 82: 53-63.
- Glasser TS (1943) An anatomic study of variations at the fossaovalis; significance of recurrences following ligations. Arch Surg 46: 289-295.
- Donchev N, Petrov V, Angelov A, Panayotov P (2015) Laser ablation with crossectomy. Angiology and Vascular Surgery 1: 5-8.
- Tibbs, DJ (ed) (1992) Vancose Veins and Related Disorders. Butterworths and Heinemann, London, p. 110-123; 379385; 446-448.
- Yang CH, Chou HS, Lo YF (2006) Incompetent great saphenous veins treated with endovenous 1,320-nm laser: results for 71 legs and morphologic evolvement study. Dermatol Surg 32: 1453-1457.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences