Anterior Tibial Artery Pseudoaneurysm Post-Endovascular Atherectomy and Revascularization
Tushar Menon1, Ameera C Mistry2*, Shahin Bhagwagar1, Bryant Kao1, Rahul Malhotra3 and Perminder Sanghera1
1Abrazo Health Network, Internal Medicine Residency Program, Glendale, Arizona, United States
2Arizona Medical Association, Phoenix, Arizona, United States
3Arizona Heart and Vascular Clinic, Glendale, Arizona, United States
- *Corresponding Author:
- Ameera C Mistry
Arizona Medical Association, Phoenix, Arizona,
United States
E-mail: ameeracmistry@gmail.com
Received date: February 17, 2023, Manuscript No. IPJVES-23-15920; Editor assigned date: February 20, 2023, PreQC No. IPJVES-23-15920 (PQ); Reviewed date: March 06, 2023, QC No. IPJVES-23-15920; Revised date: March 09, 2023, Manuscript No. IPJVES-23-15920 (R); Published date: March 13, 2023, DOI: 10.36648/2471-9943.8.1.138
Citation: Menon T, Mistry AC, Bhagwagar S, Kao B, Malhotra R, et al. (2023) Anterior Tibial Artery Pseudoaneurysm Post-Endovascular Atherectomy and Revascularization. J Vasc Endovasc Therapy Vol.8 No.1:138.
Abstract
Anterior tibial arterial pseudoaneurysms are a rare form of pseudoaneurysms that are not often reported in literature and are caused by injury to the arterial wall with resultant contained hematoma and turbulent blood flow. Presented here is a case of an anterior tibial arterial pseudoaneurysm that developed following surgical atherectomy and revascularization in a 63-year-old patient. On presentation, the patient had left lower extremity pain that worsened with palpation and that revealed an expanding pseudoaneurysm over two days from 8 mm × 5 mm to 1.6 cm × 2 cm that required open surgery and had patch angioplasty.
Keywords
Revascularization; False aneurysms; Artherectomy
Introduction
Pseudoaneurysms are false aneurysms caused by injury to the arterial wall, resulting in a locally contained hematoma with turbulent blood flow (Figure 1) [1]. Pseudoaneurysms are usually secondary to trauma or iatrogenic injury after surgical procedures while true aneurysms are a result of infections, inflammatory, congenital causes, etc. [2]. Pseudoaneurysms have an incidence of less than 1%, with most cases located in the popliteal artery [2]. Formation of anterior tibial arterial pseudoaneurysms is extremely rare, with few cases reported in literature.
Case Report
Patient is a 63-year-old male with history of ESRD on hemodialysis, diabetes mellitus, hypertension, hypercholesterolemia, coronary artery disease, carotid artery stenosis, peripheral vascular disease, Rutherford stage IV, status-post multiple lower extremity interventional procedures was transferred to the ED from an outpatient vascular lab for iatrogenic aneurysm statuspost left anterior tibial artery atherectomy and revascularization.
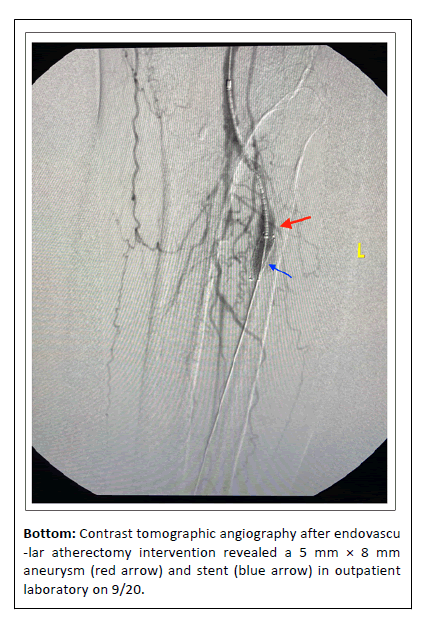
Prior to the outpatient procedure, the left anterior tibial artery showed 70%-75% stenosis proximally and occlusion distally, left peroneal artery 100% occluded proximally, and left posterior tibial artery 100% occlusion. Patient underwent Turbo- Hawk atherectomy. Post-atherectomy, Intravascular Ultrasound (IVUS) revealed 5 mm × 8 mm aneurysmal dilation (Figure 1). Immediately a covered stent was introduced to repair the aneurysmal dilation due to injury to intimal, medial layer. However it could not be positioned in the optimum location due to tracking issues. The procedure was terminated after final angiography revealed patency of the left anterior tibial artery proximally and still good flow via collaterals into the peroneal artery. Due to the size and pulsatile nature, and instability of the aneurysmal dilation, the patient was transferred to the hospital.
The patient was given nitro by EMS en route to the hospital for his chest pain. Patient’s EKG in the ED showed ST depression in the lateral leads and aVR but no acute ST elevation. Patient had troponin drawn which were flat trending with an initial being .05 and the second troponin being .05. Patient had a CXR that revealed bilateral diffuse infiltrate and he was started on empiric azithromycin and ceftriaxone.
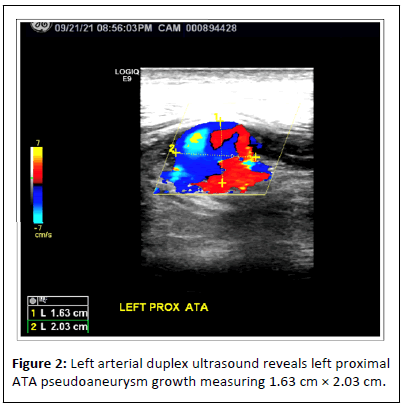
Patient’s chest pain resolved with IV morphine and dual antiplatelet therapy. Patient had a bilateral lower extremity venous doppler which was negative for DVT bilaterally. The next day, the patient had a bilateral lower extremity arterial doppler ultrasound, which revealed left mid Superficial Femoral Artery (SFA) with 50% stenosis and increased velocity, minimal flow to the left dorsalis pedis artery and left proximal ATA pseudoaneurysm measuring 1.6 cm × 2 cm, which had grown significantly since the initial study of 5 mm × 8 mm (Figure 2). Vascular surgery was consulted and the patient underwent a left anterior tibial artery aneurysm repair with saphenous vein patch angioplasty and explanation of stent.
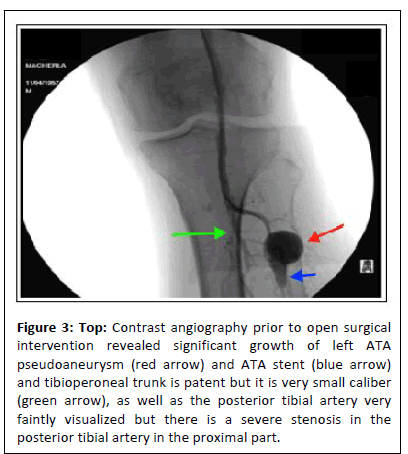
During the procedure, below-knee the patient trifurcation was visualized and showed a left ATA takeoff with a large pseudoaneurysm (Figure 3). The tibioperoneal trunk was patent but very small caliber, while the peroneal artery and posterior tibial artery were very faintly visualized and severe stenosis in the posterior tibial artery in the proximal part was noted (Figure 3). A left groin incision was made and a short segment measuring about 12 cm of left greater saphenous vein was harvested and preserved in heparin normal saline solution.
Figure 3: Top: Contrast angiography prior to open surgical intervention revealed significant growth of left ATA pseudoaneurysm (red arrow) and ATA stent (blue arrow) and tibioperoneal trunk is patent but it is very small caliber (green arrow), as well as the posterior tibial artery very faintly visualized but there is a severe stenosis in the posterior tibial artery in the proximal part.
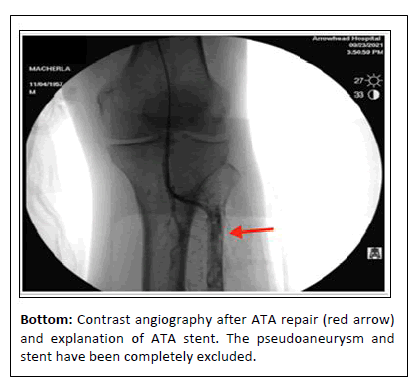
A selective angiogram of the left distal popliteal artery anterior tibial artery and the tibioperoneal trunk was done and the morphology of the aneurysm was clearly delineated. Left lower extremity anterior compartment incision was made. The skin, subcutaneous tissue was divided and the fascia was opened revealing a sizable pseudoaneurysm and clot. The mouth of this aneurysm was found to be very large; and half the ATA stent was exposed, which was explanted and sent for pathology. Saphenous vein patch was fashioned to the defect and patch angioplasty was carried out, including de-airing in standard fashion and anastomosis completed. Completion angiogram shows an excellent repair and as mentioned earlier the patient’s very poor distal runoff remained unchanged.
Patient’s left lower extremity pain improved significantly after open repair of the left anterior tibial artery pseudoaneurysm. The patient was continued on dual anti-platelet therapy. At postoperative follow-up, the patient made an excellent recovery and did not have any rest pain.
Results and Discussion
Anterior tibial artery pseudoaneurysm is a rare pathology that is not well described, with very few cases reported in the literature. Pseudoaneuryms are formed when the integrity of the arterial wall is compromised, leading to extravasation of blood into the tissue, forming a localized hematoma. The hematoma can communicate with the intravascular space freely, resulting in a pulsating visualization on IVUS [3]. Pseudoaneurysms are distinguished from true aneurysms by a wall composed of hematoma rather than the layers of a normal arterial wall. For this reason, pseudoaneurysms are more likely to expand and rupture. Rupture of the pseudoaneurysm can result in multiple complications, including hemorrhage into the surrounding soft tissue resulting in hemodynamic instability, hemarthrosis of the ankle, and even severe cases of compartment syndrome have been reported [4].
Currently, the main therapeutic modalities in the management of traumatic anterior tibial artery pseudoaneurysm include, open surgery with ligation, aneurysmectomy and reconstruction with either end-to-end anastomosis with saphenous vein grafting, or vein patch angioplasty [5]. The optimal treatment for this patient was pseudoaneurysm repair with angioplasty using the greater saphenous vein. The latest technique of using endovascular stent-grafts has shown promising results. De Roo, et al. showed that repair with covered stent graft was patent for one year [6]. Golledge, et al. also showed a patient withan ATA pseudoaneurysm that had undergone endovascular repair with two covered stents that, at the 6 week follow up, both decreased in size and was no longer pulsatile [7].
Conclusion
This patient was not a candidate for endovascular repair since earlier attempts were unsuccessful due to tracking issues, vessel tortuosity and small caliber of the native anterior tibial artery. He was followed up post-operatively and continued on dual antiplatelet therapy. The patient made an excellent recovery with resolution of rest pain and ischemia.
References
- Rivera PA, Dattilo JB (2021) Pseudoaneurysm. In: StatPearls [Internet], Treasure Island (FL): StatPearls Publishing.
- Berard X, Bodin R, Saucy F, Deglise S, Pailler A, et al. (2011) Current management of true aneurysm of the dorsalis pedis artery. Ann Vasc Surg 25: 265.
- Jacobs E, Groot D, Das M, Hermus JPS (2011) Pseudoaneurysm of the anterior tibial artery after ankle arthroscopy. J Foot Ankle Surg 50: 361–363.
- Tonogai I, Matsuura T, Iwame T, Wada K, Takasago T, et al. (2017) Pseudoaneurysm of the anterior tibial artery following ankle arthroscopy in a soccer player. Case Rep Orthop 2017: 2865971.
[Crossref] [Google Scholar] [Indexed]
- Darius Aw KL, Tan CC, Ch’ng JK, Chng SP (2017) A case report of an anterior tibial artery pseudo-aneurysm open surgical management: A rare complication post total knee arthroplasty. Int J Surg Case Rep 37: 196–199.
[Crossref] [Google Scholar] [Indexed]
- De Roo RA, Steenvoorde P, Schuttevaer HM, Den Outer AJ, Oskam J, et al. (2004) Exclusion of a crural pseudoaneurysm with a PTFE-covered stent-graft. J Endovasc Ther 11: 344-7.
[Crossref] [Google Scholar] [Indexed]
- Golledge J, Velu R, Quigley F (2008) Use of a covered stent to treat two large false aneurysms of the anterior tibial artery. J Vasc Surg 47: 1090.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences