Comparison Open and Endovascular Popliteal Aneurysm Repairs in a Single Center Experience
Ascoli Marchetti A, Martinelli F, Pratesi G, Di Giulio L, Battistini M and Ippoliti A
DOI10.21767/2573-4482.19.04.24
Vascular Surgery Biomedicine and Prevention Departement, University of Rome Tor Vergata, Italy
- *Corresponding Author:
- Ascoli Marchetti A
Vascular Surgery Biomedicine and Prevention Departement
University of Rome Tor Vergata, Italy
Tel: +39 06 2090 2837
E-mail: ascolimarchetti@med.uniroma2.it
Received Date: October 18, 2019; Accepted Date: December 20, 2019; Published Date: December 27, 2019
Citation: Marchetti AA, Martinelli F, Pratesi G, Di Giulio L, Battistini M, et al. (2019) Comparison Open and Endovascular Popliteal Aneurysm Repairs in a Single Center Experience. J Vasc Endovasc Therapy, Vol.4 No.4:24
Abstract
Background: The treatment of the popliteal artery aneurysm is feasible with conventional and endovascular methods. However, there is no unanimous agreement on the best choice both in asymptomatic and symptomatic cases. The purpose of this retrospectively study was to compare perioperative and mid-term results of open and endovascular repair on both symptomatic and asymptomatic patients, in our clinical experience.
Method: Altogether 49 surgical interventions were retrospectly reviewed, OPEN treatment was used in 20 cases and in 29 cases endovascular treatment. The procedures were made from August 2011 to May 2018.
Result: Primary patency at the medium follow up 28 months was 80% in the OPEN group and 83% in the ENDO group (P=0.8, log-rank: 0.7, 95% CI: 0.2-0.3). The secondary patency was 90% (18/20 pts) in the OPEN group and 93% (27/29 pts) in the ENDO group (P=0.7, log-rank: 0.5, 95% CI: 0.1-0.2). Freedom from amputation was 100% in the OPEN group and 93% in the ENDO group (P=0.2, log-rank: 0.2, 95% CI: 0.2-0.3). Survival was 80% in the OPEN group and 86% in the ENDO group (P=0.6, log-rank: 0.6, 95% CI: 0.2-0.3).
Conclusion: Endovascular treatment represents a safe alternative to OPEN surgery, for treating the aneurysms of the popliteal artery. In addition, the advancement of technology, that has improved the available stent characteristics, and the correct selection of patients, have allowed to improve outcomes, making it comparable to OPEN surgery; in our series symptomatic patients too.
Keywords
Registry; Outpatient; Endovascular interventional office procedures
Introduction
Popliteal artery aneurysms (PAAs) are the most common peripheral arterial aneurysms and is the second most frequent localization of arterial aneurysm, with an incidence of 7.4 of 100.000 people [1]. Commonly accepted indications for repair include size >2cm in asymptomatic patient. The most commonly symptoms are acute thrombosis or embolism with limb ischemia, or pain and/or swelling associated with axtrinsic popliteal vein compression. This condition, if untreated, can lead to high rate of complications, include risk of limb loss and death [2].
The first description of surgical repair of a PAA was in 1795 by John Hunter, who succesfully legated a large aneurysm at the adductor canal [3]. During the last five decades, open repair of PAAs (OPAR) has proved to be extremely durable with ecxellent long term patency (primary patency up to 76% at 5 years) [4-6]. For this reason open repair with PAA exclusion and bypass or direct endoaneurysmorrhaphy has been the gold standard management strategy. Marin et al. First described the use of covered stent as means of PAAA repair in 1994 [7]. Since this date, endovascular intervention has become an attractive altrnative to open repair cause offers many potential advantages, including the use of local anestesia, shorter hospital stay and decreased blood loss. It can also represent alternative therapy in patients with relevant comorbidities and choice in case of non ideal indication for open surgery as in case of proximal involvement to the superficial femoral artery Although early reports yelded modest results with high thrombotic complications [8].
The aim of this retrospectively study was to compare perioperative (<30 days) and mid-term (36 months) results of open and endovascular repair on both symptomatic and asymptomatic patients, in our clinical experience. The outcomes of the study was primary patency at 6 months, at 1 year and then annually, secondary patency, freedom of amputation and mortality.
Methods
The patients, who underwent a surgical or endovascular repair of PAA from August 2011 to May 2018, were retrospectly reviewed. All procedures were performed at the “Policlinico Tor Vergata” of Rome, in the angiographic room or in the operating room. Altogether 49 surgical interventions were performed in 41 patients, 39 men and 2 women, with an average age of 73 years. OPEN treatment was used in 20 cases and in 29 cases endovascular treatment. 25 patients had bilateral aneurysm with an average transverse diameter of 35 mm. Both elective and emergency patients were included in the study.
All patients were subjected to ecocolorDoppler and angio-Tc before surgery, except the patients with acute ischemia IIb and III, according to Rutherford, who were submitted to operating room after performing ecocolorDoppler.
The asymptomatic patient was treated for aneurysm with a maximum transverse diameter greater than 2.5 cm. While in the asymptomatic the indication was related to the clinical condition of the patients.
OPEN treatment was performed both with a posterior approach, aneurysmectomy and packing of an inverted autologous saphenous vein, when a caliber>5 mm was measured with preoperative ecocolordoppler, as with a medial approach by performing autologous synthetic bypass (Dacron knitted or PTFE heparin bonded 7 and 8 mm). The choice of the method took into account the extent of the pathology, the comorbidity of the patient, the presence of insufficient venous assests and the operator's preference are have been shown in Table 1. In the selection criteria, the preference for ENDO intervention was suggested by the absence of outflow and the onset of symptoms <12 hours. We evaluate, for the endovascular feasibility, the proximal and distal landing zones, which should in both cases be at least 2 cm. Even the distal run-off has been of great importance in the choice, in fact there must be at least one tibial vessel. The choice of diameter was performed on the basis of ultrasound appearance and based on angiographic evidence after fibrinolysis. An endograft oversized of at least 10-15% of the landing zone was performed. When more than one stent was needed, an overlap of about 2 cm was repeated to prevent the onset of endoleak III. Overlapping stents differed in diameter for not more than 2 mm. In the presence of incomplete proximal sealing, ballooning and / or stenting was performed if necessary.
Endovascular interventions were performed both in the angiographic room and in the operating room. Patients with mild to moderate acute ischemia (Rutherford classification I-IIa), with acute thrombosis of the aneurysmatic sac, were subjected to urokinase preoperative local-regional thrombolysis. Thrombolytic treatment provided a bolus of 100,000 U.I. Followed by a continuous infusion of 70,000 U.I./h and 1000 to 1500 U.I./h of sodium heparin with the objective of doubling the normal value of partial thromboplastin. The continuous infusion of thrombolytic occurred for 24, 48 or 36 hours, according to the restoration of the patency of the poplite artery and at least one tibial vessel. OPEN surgery was performed at least 24 hours after cessation of thrombolytic infusion. If thrombolysis was unsuccessful, however, an OPEN surgical intervention was performed (Table 1).
Table 1: Comparison of preoperative symptoms and clinical findings in the OPEN and ENDO groups.
| Variable | OPEN | ENDO | P |
|---|---|---|---|
| Thrombosed PAA | 12 (60%) | 14 (48%) | 0.2 |
| Asymptomatic PAA | 5 (25%) | 14 (48%) | 0.5 |
| Symptomatic PAA | 15 (75%) | 15 (52%) | 0.1 |
| Claudicatio | 9 (45%) | 1 (3.5%) | |
| Critic Ischemia | 3 (15%) | 10 (35%) | |
| Acute Ischemia | 3 (15%) | 10 (35%) | |
| Blue Toe Syndrome | 0 | 10 (3.5%) | |
| Venous Compression | 2 (10%) | ||
| Run off <2 vessels | 7 (35%) | 8 (28%) | 0.8 |
| Urgent | 3 (15%) | 11 (38%) | 0.07 |
| Acute Ischemia | 8 (40%) | 11 (38%) | 0.07 |
| Fibrinolysis pre | 1 (5%) | 7 (24%) | 0.05 |
All patients in the postoperative period undergoing OPEN treatment followed antiplatelet therapy with acetylsalicylic acid 100 mg/day. Patients undergoing ENDO treatment received double anti-aggregation with acetylsalicylic acid 100 mg/day and clopidogrel 75 mg or ticlopidine 250mg.
The surveillance program consisted of a clinical and ecocolorDoppler evaluation at 1, 6, 12 months and then each year. During the study, the patency of the graft, the anastomosis status, inflow and outflow vessels, and the controlateral femoro-popliteal axis were analyzed. In addition, the complete exclusion of the aneurysmal sac was also examined in patients undergoing vascular surgery.
Demographic and clinical data were evaluated by T-test for independent samples and statistically significant values were considered with P value <a 0.05.
The primary outcome of the study was analyzed by survival curves according to Kaplan-Meier, with a comparison of the two groups according to log-rank test. Statistical analyzes were performed with dedicated SSPS software.
Primary patency begins with the execution of the first revascularization, when the patency of the segment is reestablished; Determines how long the segment continues to run without the need for further procedures at the margins and within the segment previously treated. Secondary patency begins with the second successful treatment and establishes the duration of the treatment itself. Freedom from amputation is defined as absence of amputation above or below the knee. Total survival is the absence of death at follow-up.
Results
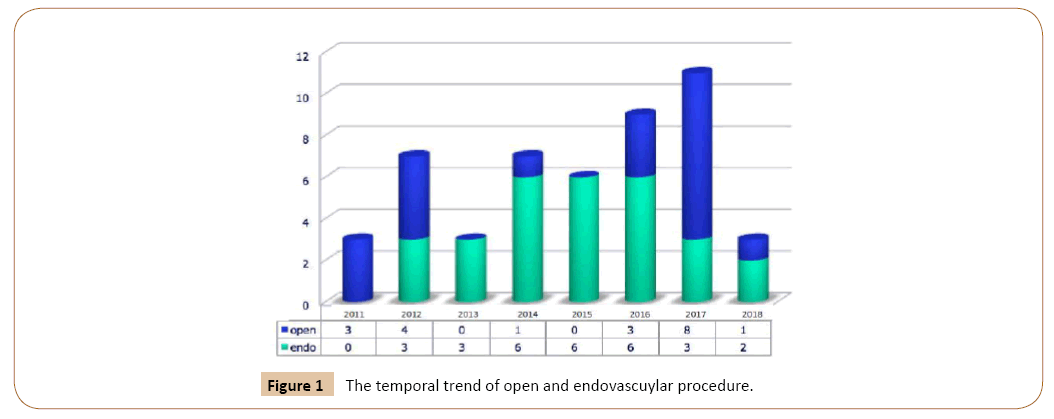
There are no statistically significant differences between the two groups regarding demographic characteristics, risk factors and the anesthesiological risk. This meant that it was not taken into consideration for the decision on the treatment to be adopted (Figure 1). While there is a significantly higher percentage of patients with acute ischemia (0.07 and 95% 0.5-0.2), patients undergoing urgent intervention (P 0.07 and 95% 0.5-0.2) and subjected to pre-operative thrombolysis in the endovascular group (P-value 0.05 and CI 95% 0.4-0) (Table 2).
Table 2: Demographic data and comorbidity of the patients.
| Variable | OPEN | ENDO | P |
|---|---|---|---|
| Mean age | 71.95 | 75.07 | 0.3 |
| Gender | F (1) M (19) | F (2) M (27) | 0.8 |
| Arterial hypertension | 20 (100%) | 29 (100%) | |
| Hyperlipidemia | 16 (65%) | 18 (62%) | 0.8 |
| Diabetes | 6 (30%) | 7 (24%) | 0.7 |
| Smoker or past somker | 20 (100%) | 28 (97%) | |
| Coronary artery disease | 9 (45%) | 10 (34%) | 0.5 |
| COPD | 12 (60%) | 19 (65%) | 0.7 |
| Mean PAA Diameter | 37.8 mm | 34.3 mm | |
| Bilateral | 9 (45%) | 16 (55%) | 0.5 |
| Others aneurysms | 8 (40%) | 12 (41%) | 0.9 |
In 11 cases (22%) there was bilateral intervention, 3 cases in the OPEN group and 8 cases in the ENDO group. Another aneurysm was present in 20 cases (21%) and aneurysm was located in ascending aorta in 1 case (1%), thoracic abdominal iliac in 1 case (2%), abdominal aorta in 14 cases (29%), abdominal aorta and iliac arteries in 1 case (2%), iliac-femoral tract in 2 cases (4%) and iliac isolated in 1 case (1%). One patient had an entrapment of the popliteal artery (2%), which was inspired by popliteal aneurysms. Three patients (6%) had previously been subjected to TEA carotid.
Eight patients with acute ischemia grade I and IIa according to Rutherford (however with symptomatic symptoms within 72 hours) due to complete thrombosis of the aneurysm were subjected to preoperative thrombolysis, 7 (24%) in the endo group and 1 (5%) in the OPEN group (P-value 0.05 and CI 95% 0.4-0). In the OPEN group only in one patient, 1/20 (5%) was contraindicated the fibrinolytic therapy for an antecedent of cerebral haemorrhage Fibrinolysis was successful demonstrated by angiographic control in 7 (88%) out of eight patients, all of whom belong to the endovascular group in 7 (88%) out of eight patients, all of whom belong to the endovascular group. The average time of thrombolysis was 31 hours. No major complications were associated with fibrinolytic and anticoagulant treatment, while a patient belonging to the ENDO group reported pseudoaneurysm of the common femoral as a percutaneous complication of Mcnamara catheter’s positioning
In the surgical group in 6 cases (30%) there was aneurysmectomy and a large autologous inverted vein extracted from the contralateral artery. In 14 cases (70%), a medial access was chosen, ten times a saphenous autologous vein was used and in four times a PTFE prosthesis. In 1 case (5%) the inflow vessel was the femoral joint, in 17 cases (85%) the surface femoral, and in only 2 cases (10%) the artery poplitea. The outflow vessel was in 19 cases (95%) in the poplite artery and in only 1 case (5%) the tibio-peroniero trunk. In 1 case (5%) intraoperative poplitea entrapment was diagnosed, caused by abnormal insertion of mediastinal gastrocnemio, with vessel occlusion and consequent post-stenotic poplite aneurysm. The tendon and subsequent aneurysmatic prosthesis in VSA were then removed. In 3 cases (15%) it was necessary to perform an embolectomy according to Fogarty of the leg vessels, in 1 case (5%) at the level of the femoral surface and leg vessels, in 1 case (5%) at the vessels of Leg with associated fasciotomie intervention of the leg leg lodge. All patients were given heparine 5000 UI , in bolo All patients were treated postoperative with anti-aggregate therapy (1 drug in 16 cases and double anti-aggregation in 4 cases).
In the endovascular group, a flow diversion stent (Cardiatis stent) was placed two time (7%), and in the remaining cases, 27 (93%) were placed Viabhan coated stents. In 2 cases (7%) surgical access was required and in one case a second a embolectomy of the surface femoral. In 27 cases (97%), a percutaneous access was performed, 15 times with anterograde access and 13 with controlateral access. In 21 cases (72%) the inflow vessel was superficial femoral, in the remaining cases, 8 (28%), the proximal landing area of the stent was the popliteal artery. The distal landing area of the stent was the popliteal artery in 27 cases (93%) and the tibial peroniero trunk in 2 cases (7%). In one case a baloon kissing of the tibio-peroniero trunk was performed, in one case (3.5%) a PTA of the tibial vessels associated with thrombussuction, in 5 cases (18%) an isolated PTA and In 1 case (3.5%) an isolated thrombo-aspiration of the leg vessels. All patients in the endovascular group were subjected to 5000 U.I. sodium heparin bolus at the insertion site.
Perioperative outcomes (<30 days)
Technical success has been achieved in 100% of the interventions of the OPEN and Endovascular groups.
In the OPEN group in 1 case (5%), on postoperative day 5, an occlusion of VSAI bypass was happened. For this reason, the patient was subjected to re-intervention with replication of femoral-poplite by-pass with PTFE medial access. Three patients (15%) died cause of postoperative myocardial infarction, one for acute pulmonary edema in the postoperative day 8, and one for postoperative riperfusion syndrome on postoperative day 10.
In two case (6.8%), on the first postoperative day, an amputation of the thigh for acute occlusion of Viabahn stent was required and in 10 postoperative day the other, amputation was necessary due to severe acute ischemia In the ENDO group, the amputation liberty was 93%. In fact, in 2 cases, on the postoperative day 1 one, and 10 the other, amputation was necessary due to severe acute ischemia. There were 2 deaths (7%), in the endovascular group, one for sepsis on postoperative day 10, and one for riperfusion syndrome in the postoperative day 25.
Follow-up outcomes
It was possible to collect data of all 49 interventions during follow-up, with an average of 28.9 months (min 1, max 75).
In the OPEN group a further death for acute pulmonary edema occurred 72 months after the surgery. In the ENDO group there were another 2 deaths, one for myocardial infarction at 20 months from surgery and one for acute 31-month pulmonary edema from surgery. The follow-up was similar in the two groups (28.61 months in OPEN and 29.41 months in the ENDO).
Primary patency at 28 months (medium follow up) was 80% in the OPEN group and 83% in the ENDO group (P=0.8, log-rank: 0.7, 95% CI: 0.2-0.3) (Table 3). In the OPEN group a dacron bypass in one case, on the fifth day after surgery, the by-pass was removed for the suspicion of greater thrombogenicity and to use the same anatomical conduit, a fuhrer PTFE by-pass was packaged In one case, after 3 months of surgery, due to an infection in the proximal anastomosis, the prosthesis was removed and replaced with a new PTFE prosthesis. In two cases, 7 and 10 months after surgery, a locally-regional thrombolysis was performed; In either case, a proximal anastomosis PTA was required.
Table 3: Primary patency at 28 months in the two groups.
| OPEN | ENDO | P | CI 95% | |
|---|---|---|---|---|
| Amputation | 0 | 1 (3%) | 0.3 | 0.1-0.3 |
| Reintervention | 1 (5%) | 1 (3%) | 0.8 | 0.1-0.1 |
| Thrombosis | 1 (5%) | 1 (3%) | 0.8 | 0.1-0.1 |
| Death | 2 (10%) | 0 | 0.2 | 0.4-0.2 |
In the ENDO group in 3 cases, fibrinolysis was required at 3, 5 and 21 months after endovascular intervention. In one of the 3 cases it was necessary to perform a concomitant PTA with drug coated ballon.
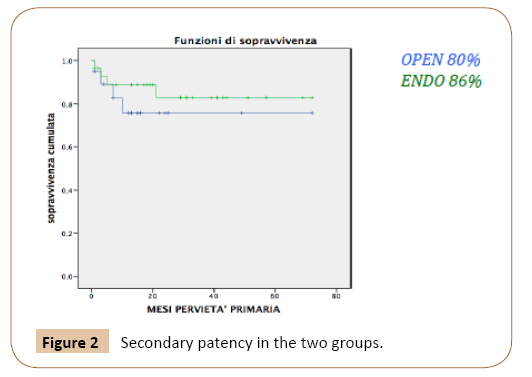
The secondary patency was 90% in the OPEN group and 93% in the ENDO group (P=0.7, log-rank: 0.5, 95% CI: 0.1-0.2) (Figure 2). Of patients undergoing OPEN surgery in 2 cases there was a recurrence of graft thrombosis. One was treated with fibrinolysis and subsequent placement of Viabahn stent, within the by-pass, second to relining technique. While the other one, 10 months after the previous advent, was treated with fibrinolysis and subsequent PTA of proximal anastomosis. In the endovascular group there has been a recurrent thrombosis on two occasions. In one case on post-operative day 1, amputation was necessary due to severe ischemia. While in another case, 25-months after procedure, a patient was subjected a re-intervention to localregional thrombolysis for acute stenosis occlusion.
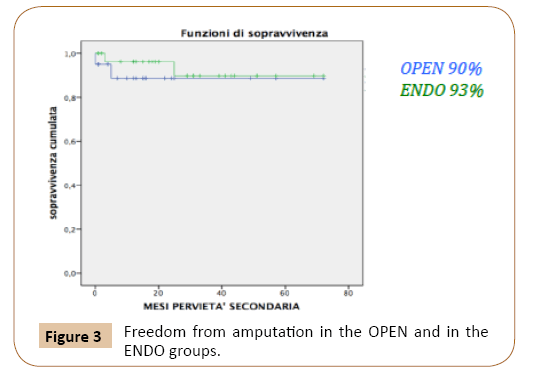
Freedom from amputation was 100% in the OPEN group and 93% in the ENDO group (P = 0.2, log-rank: 0.2, 95% CI: 0.2-0.3), in fact, in 2 cases, both within one month of intervention, amputation was necessary due to severe acute ischemia (Figure 3).
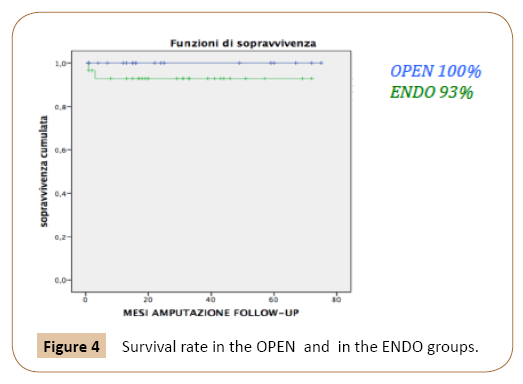
Survival was 80% in the OPEN group and 86% in the ENDO group (P = 0.6, log-rank: 0.6, 95% CI: 0.2-0.3) (Figure 4). Four deaths were observed in the follow up: 2 cases, 2 cases (1 month and 72 months) for acute pulmonary edema, one case of myocardial infarction (1 month), and one case for reperfusion syndrome occurred in the surgical group. In the ENDO group, 4 deaths occurred. Two within the first month, overdue. The other two deaths occurred at 20 and 31 months after surgery, respectively due to a myocardial infarction and acute pulmonary edema.
Discussion
Although the surgical treatment of popliteal aneurysms is still considered the gold standard, with a primary patency and secondary patency reported in the literature respectively of 66% -76% and 84-87% [4,5], the endovascular approach is finding consensus in several studies [5,9-12]. Its advantages are clear: it is less invasive and potentially presents less risk.
The only medical treatment of poplitel aneurysm is related to a high risk of serious complications, for this reason asymptomatic patients with aneurysms greater than 2 cm may be subjected to surgical or endovascular treatment [13]. The symptomatic patient should be treated as early as possible in order to avoid the risk of amputation of the limb. In the literature, the benefits of endovascular treatment, particularly in the short term, are well described, with limited access related complications and shortened stay time [14-16]. While it has worse results in terms of primary patency than patients undergoing surgical treatment. The data is probably due to the presence of a higher percentage of short-term thrombosis, especially at the beginning of endovascular experience, where old-fashioned stent grafts were present. Antonello et al., n a study published in 2005 reported a 30- day thrombosis rate of 9.5% [17]. Currently, the most used stent for the treatment of the artery poplitea, the Viabahn, since 2007 is produced with some modifications such as the introduction of a heparin covered surface and a lower profile (further down from 2011). Additionally, the use of double anti-aggregation and careful selection of the patient to undergo endovascular treatment has improved results over time. These changes added to a better confidence of the operators with the methodology have allowed to treat longer and complex lesions that require coverage of a longer artery segment. A meta-analysis, recently published by Leake et al. [18], reports 76% of primary patency, 87% secondary patency in Open surgery and 68% of primary patency and 85% secondary patency in Endovascular treatment.
Tiellu et al. reported, in 57 cases, where only the Viabahn stent was used, a 77% primary patency and 87% secondary patency to 2 years of follow-up [19].
Another key point is the number of below the knee vessels In fact, a low runoff, is associated with a worsening of outcomes for both surgical treatment and endovascular treatment, also in our experience.
Among the technical details, it is worth noting the excessive discrepancy between the proximal and the distal landing zones, because the excessive oversizing required is an increased risk of stent infolding at the distal landing zone. In our experience the discrepancy was never greater than 2 mm and patients with greater discrepancy were treated with OPEN.
Curi et al. have retrospectively analyzed 15 endovascular treatments (all asymptomatic) and 41 OPEN, , which also had patients with acute ischemia. Respectively the primary and secondary patency reported are 83% and 100% at 24 months in the endovascular group [20].
Stone et al. reported 24 cases of endovascular treatment and 64 OPEN interventions and, at 3 years follow-up, the primary patency were respectively 63.7 % and 7.8% [21].
We are no able to report experience with the new nititinol sistem. In long and complex occlusive femoropopliteal disease, the Supera stent is an excellent alternative with clinical and patency results at 1 year. However, during the study period we prefer covered stent. Recent experience in this district did not suggest the use of this promising device [22].
Pulli et al., In 2012, reported their experience in this regard, comparing 43 cases of OPEN treatment with 21 endovascular cases. At 24 months, primary patency, secondary patency and freedom from amputation were respectively 78%, 81%, 93% in the surgical group and 61.5%, 78%, 95% in the Endovascular group [23]. Only two flow diverter stents were used in our study. The preliminary results of this graft do not seem to be encouraging [24]. Also Shahin Y reported in a Meta-Analysis the same conclusion. From the experience of this study and of the Literature the endo approach seems to be preferable in case of occlusion of the leg vessels, aneurysms <3 cm in dtm, in patients at high risk for comorbidity with inadequate venous assest for bypass, as long as it does not preclude any subsequent surgical approach [25,26].
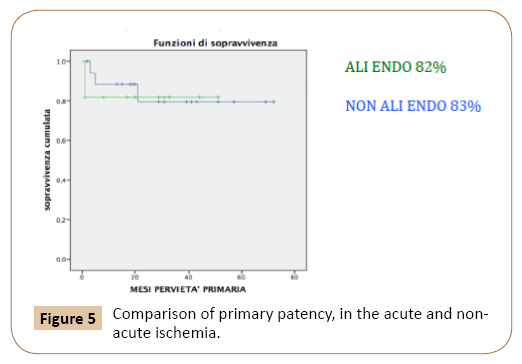
In this study there were no apparent diffrents between the two groups with the exception of clinical features, with a greater number of cases of acute ischemia within the endovascular group. Despite this, the endovascular group has shown good results in terms of primary patency, secondary patency, freedom from amputation, and overall survival when compared to the literature data’s. Indeed, our study reports a 82% primary patency, in the subgroup of patients with acute ischemia treated with endovascular technique (Figure 5).
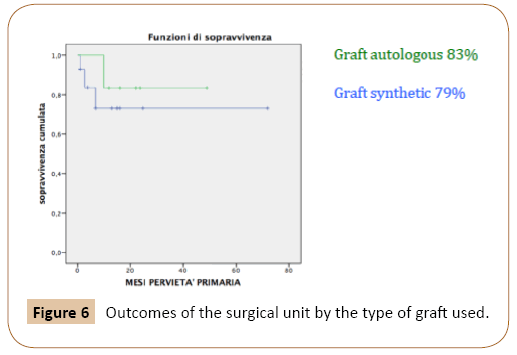
In addition, the outcomes of the surgical unit seem to be affected by the type of graft used. In fact, VSAI group has a better primary patency (83%) if compared to synthetic graft (79%) (Figure 6). This result is in line with the data in the literature, describing better outcomes for autologous grafts. The data may have a bias. In fact, the number of cases is limited and also all the surgical procedures where VSAI was used were performed by posterior access and consequently there were small aneurysms confined to the popliteal artery.
Limitations of the Study
In the present study there are more urgently treated patients in the ENDO group. However the aim of the work is to document the non-inferiority of the endovascular treatment compared to the open group.
Conclusions
Endovascular treatment represents a safe and lasting alternative to OPEN surgery, for treating the aneurysms of the popliteal artery. In addition to the advantages offered in terms of shortterm complications (access, hospital stay) already demonstrated in numerous studies in the literature, our study shows excellent results of endovascular treatment both on asymptomatic patients and patients with acute ischemia. In addition, the advancement of technology, that has improved the available stent characteristics, and the correct selection of patients have allowed to improve outcomes, making it comparable to OPEN surgery.
References
- Lawrence PF, Lorenzo-Rivero S, Lyon JL (1995) The incidence of iliac, femoral, and popliteal artery aneurysms in hospitalized patients. J Vasc Surg 22: 409-416.
- Ravn H, Wanhainen A, Bjorck M (2007) Surgical technique and long-term results after popliteal artery aneurysm repair: results from 717 legs. J Vasc Surg 46: 236-243.
- Perry MO (1993) John hunter-triumph and tragedy. J Vasc Surg 17: 7-14.
- Huang Y, Gloviczki P, Noel AA, Sullivan TM, Kalra M, et al. (2007) Early complications and long-term outcome after open surgical treatment of popliteal artery aneurysms: is exclusion with saphenous vein bypass still the gold standard? J Vasc Surg 45: 706-713.
- Pulli R, Dorigo W, Troisi N, Innocenti AA, Pratesi G, et al. (2006) Surgical management of popliteal artery aneurysms: which factors affect outcomes? J Vasc Surg 43: 481-487.
- Martelli E, Ippoliti A, Ventoruzzo G, De Vivo G, Ascoli Marchetti A, et al. (2004) Popliteal artery aneurysms. Factors associated with thromboembolism and graft failure. Int Angiol 23: 54-65.
- Marin ML, Veith FJ, Panetta TF, Cynamo J, Bakal CW, et al. (1994) Transfemoral endoluminal stented graft repair of a popliteal artery aneurysm. J Vasc Surg 19: 754-757.
- Gerasimidis T, Sfyroeras G, Papazoglou K, Trellopoulos G, Ntinas A, et al. (2003) Endovascular treatment of popliteal artery aneurysms. Eur J Vasc Endovasc Surg 26: 506-511.
- Varga ZA, Locke-Edmunds JC (1994) Baird RNA multicenter study of popliteal aneurysms. Joint Vascular Research Group. J Vasc Surg 20: 171-177.
- Taurino M, Calisti A, Grossi R, Maggiore C, Speziale F, et al. (1998) Outcome after early treatment of popliteal artery aneurysms. Int Angiol 17: 28-33.
- Mahmood A, Salaman R, Sintler M, Smith SR, Simms MH, et al. (2003) Surgery of popliteal artery aneurysms: A 12-year experience. J Vasc Surg 37: 586-593.
- Speziale F, Sirignano P, Menna D, Capoccia L, Mansour W, et al. (2015) Ten years' experience in endovascular repair of popliteal artery aneurysm using the Viabahn endoprosthesis: A report from two Italian vascular centers. Ann Vasc Surg 29: 941-949.
- Stiegler H, Mendler G, Baumann G (2002) Prospective study of 36 patients with 46 popliteal artery aneurysms with non-surgical treatment. Vasa 31: 43-46.
- Stone PA, Jagannath P, Thompson SN, Campbell JE, Mousa AY, et al. (2013) Evolving treatment of popliteal artery aneurysms. J Vasc Surg 57: 1306-1310.
- Serrano Hernando FJ, Martínez López I, Hernández Mateo MM, Hernando Rydings M, Sánchez Hervás L, et al. (2015) Comparison of popliteal artery aneurysm therapies. J Vasc Surg 61: 655-661.
- Huang Y, Gloviczki P, Oderich GS, Duncan AA, Kalra M, et al. (2014) Outcomes of endovascular and contemporary open surgical repairs of popliteal artery aneurysm. J Vasc Surg 60: 631-638.
- Antonello M, Frigatti P, Battocchio R, Lepidi S, Cognolato D, et al. (2005) Open repair versus endovascular treatment for asymptomatic popliteal artery aneurysm: Results of a prospective randomized study.J Vasc Surg 42: 185-193.
- Leake AE, Segal MA, Chaer RA, Eslami MH, Al-Khoury G, et al. (2017) Meta-analysis of open and endovascular repair of popliteal artery aneurysms. J Vasc Surg 65: 246-256.
- Tielliu IF, Verhoeven ELG, Zeebregts CJ, Prins TR, Span MM, et al. (2005) Endovascular treatment of popliteal artery an-eurysms: results of a prospective cohort study.J Vasc Surg 41: 561-567.
- Curi MA, Geraghty PJ, Merino OA, Veeraswamy RK, Rubin BG, et al. (2007) Mid-term outcomes of endovascular popliteal artery aneurysm repair. J Vasc Surg 45: 505-510.
- Stone PA, Jagannath P, Thompson SN, Campbell JE, Mousa AY, et al. (2013) Evolving treatment of popliteal artery aneurysms. J Vasc Surg 57: 1306-1310.
- Myint M, Schouten O, Bourke V, Thomas SD, Lennox AF, et al. (2016) A real-world experience with the supera interwoven nitinol stent in femoropopliteal arteries: midterm patency results and failure analysis. J Endovasc Ther 23: 433-441.
- Pulli R, Dorigo W, Fargion A, Pratesi G, Innocenti AA, et al. (2012) Comparison of early and midterm results of open and endovascular treatment of popliteal artery aneurysms. Ann Vasc Surg 26: 809-818.
- Tessarek J, Görtz H (2015) New aspects of endovascular treatment for popliteal aneurysms: first results of a pilot trial. Zentralbl Chir 140: 535-541.
- Shahin Y, Barakat H, Shrivastava V (2016) Endovascular versus open repair of asymptomatic popliteal artery aneurysms: a systematic review and meta-analysis. J Vasc Interv Radiol 27: 715-722.
- Tanner I Kim, Bauer E (2019) Sumpio management of asymptomatic popliteal artery aneurysms. Int J Angiol 28: 5-10.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences