Delayed Critical Stenosis in a Zenith Alpha Stent-Graft Used for the Treatment of Blunt Thoracic Aortic Injury
Rohan Arasu*, Ian Campbell, and Juanita Muller
Department of Vascular Surgery, Princess Alexandra Hospital, Woolloongabba, Australia
- *Corresponding Author:
- Rohan Arasu
Department of Vascular Surgery,
Princess Alexandra Hospital, Woolloongabba,
Australia,
E-mail: rohan_arasu@outlook.com
Received date: September 01, 2022, Manuscript No. IPJVES-22-15760; Editor assigned date: September 03, 2022, PreQC No. IPJVES-22-15760 ( PQ); Reviewed date: September 14, 2022, QC No. IPJVES-22-15760; Revised date: September 23, 2022, Manuscript No. IPJVES-22-15760 (R); Published date: September 30, 2022, DOI: 10.36648/2471-9943.7.9.002.
Citation: Arasu R, Camobell I, Muller J (2022) Delayed Critical Stenosis in a Zenith Alpha Stent-Graft Used for the Treatment of Blunt Thoracic Aortic Injury. J Vasc Endovasc Therapy Vol.7 No.9: 002.
Abstract
Introduction: Thoracic Aortic Endovascular Repair (TEVAR) is the preferred method for managing Blunt Thoracic Aortic Injuries (BTAI) but lacks robust long-term data reporting on potential delayed complications.
Case report: We present a case of a seventeen-year-old male who developed delayed critical stenosis of a Zenith Alpha stent-graft by Cook Medical which was used for treatment of a grade-2 BTAI. This was successfully managed with endovascular relining using a Zenith TX2 stent-graft.
Discussion: The complication is rare in the literature with the proposed mechanism being thrombosis secondary to infolding of the graft material as investigated by the TRANSFIX study. Endovascular re-lining of the TEVAR was successful in this patient, however, the long-term durability of the repair remains uncertain.
Conclusion: Thrombosis of TEVAR stent-grafts used for BTAI is probably a more common complication than is appreciated; especially with the Zenith Alpha device and ongoing surveillance of such patients is therefore recommended.
Keywords
Thoracic Endovascular Aortic Repair (TEVAR); Blunt Thoracic Aortic Injury (BTAI); Thoracic Aorta; endovascular surgery; Cardiothoracic Surgery; Vascular Surgery
Statements and Declarations
Informed Consent: The patient who is the subject of the case report has provided written consent for publication of this article.
Presentation: This article was presented as an oral presentation at the Vascular Society of New Zealand (VSNZ) 2021 annual scientific conference.
Introduction
Thoracic Endovascular Aortic Repair (TEVAR) has become the preferred treatment modality for blunt thoracic aortic injuries (BTAI) due to the reduced early surgical mortality and a reduced incidence of spinal cord ischemia compared to open repair. 1 This is especially relevant as these aortic injuries are associated with other concomitant poly-traumatic injuries in an often critically unstable patient. Short- to mid-term results in terms of durability of repair have generally been satisfactory 1 with the common complications being proximal seal inadequacies, spinal cord ischemia and groin complications. We report on a rarer complication where an implanted TEVAR stent-graft developed thrombotic critical distal stenosis, resulting in symptomatic distal malperfusion. This complication was successfully managed with the relatively novel technique of endovascular relining. This case directs attention to the concerns around the long-term durability of these repairs and their associated devices, which is particularly relevant as the demographic of BTAI patients is generally of a young age
Case Presentation
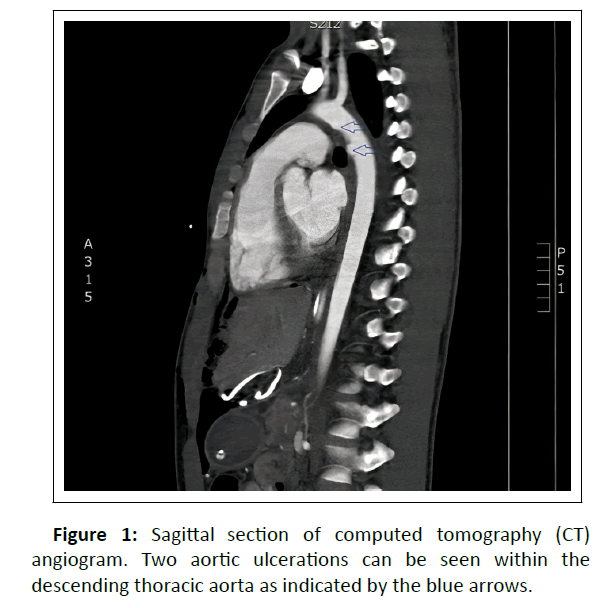
A seventeen-year-old male was admitted with a BTAI following a high-speed motor-vehicle accident. His other polytraumatic injuries included bilateral lower limb compound fractures requiring operative fixation, multiple intra-abdominal injuries requiring laparotomy, bilateral lung contusion and multifocal cerebral contusion. Emergency Computed Tomographic Angiogram (CTA) showed two individual aortic ulcerations distal to the left subclavian artery over a 2cm segment as demonstrated in Figure 1. This was followed by a Transoesphageal Echocardiogram (TOE) which suggested the presence of aortic Intramural Haematoma (IMH) associated with the intimal defects. The patient underwent TEVAR given the grade-2 classification based on the presence of IMH on TOE and the high force associated with the initial trauma. A 22mm x 105mm Zenith Alpha device by Cook Medical was deployed with near-complete covering of the left subclavian artery due to its proximity to the injury at the aortic isthmus. The stent-graft used was the smallest diameter device that was available to us which resulted in oversizing by 18%. This was based on a measured aortic calibre of 18 mm on the initial CTA prior to extensive resuscitation. This degree of oversizing remained within the recommended range in the Instructions For Use (IFU) set by the manufacturer. Post-completion angiogram showed successful exclusion of the injury without evidence of an endoleak. The patient had serial CTA imaging during his threemonth admission which showed no evidence of complications, however, the patient was lost to follow-up after being discharged.
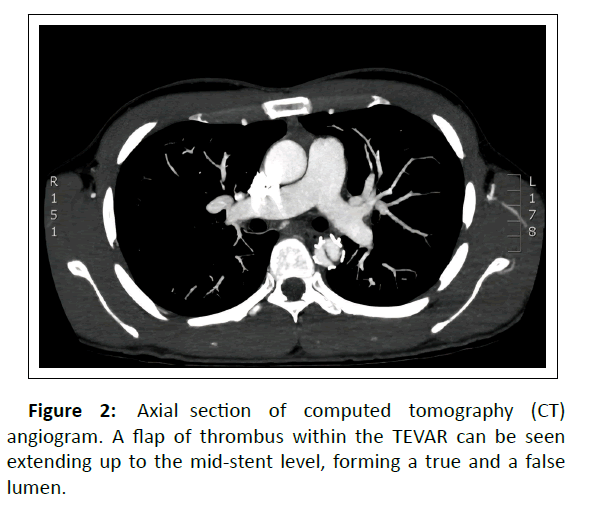
Two and a half years later, the patient represented with recurrent headaches and hypertension diagnosed by his general practitioner. The patient unusually reported no symptoms of distal malperfusion which was contrary to his clinical examination which revealed no palpable femoral pulses, a radial-femoral pulse delay and a blood pressure of 191/104 mmHg though to be caused by renal malperfusion. CTA showed a flap of thrombus extending superiorly from the distal edge of the stent up to the mid-stent level, forming a true and false lumen as seen in Figure 2. This was further evaluated with TOE which showed significantly elevated velocities through the true lumen consistent with critical stenosis.
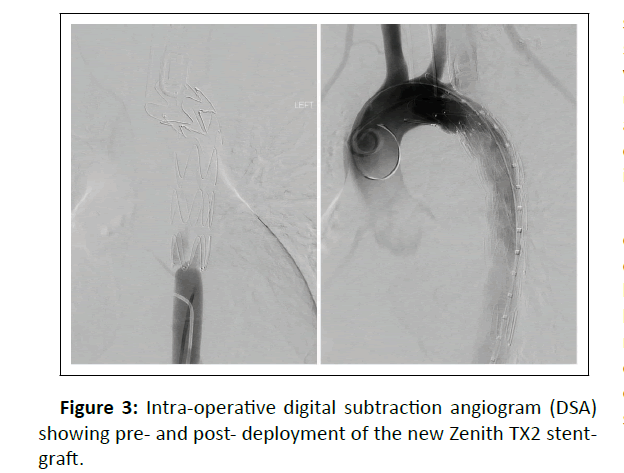
There was concern that the patient would develop acute thrombotic occlusion of the stent-graft and therefore was commenced on therapeutic anticoagulation with enoxaparin. His hypertension was significantly resistant to medical management, requiring four agents. After careful consideration, the decision was made to attempt endovascular re-lining of the stent-graft. The true lumen was cannulated with a guidewire using intraoperative TOE for confirmation of entry into the correct lumen. The severity of the stenosis was more appreciable on fluoroscopic imaging as can be seen in , which shows virtually no entry of contrast through the stent-graft with the catheter positioned inferiorly. A 22mm x 115mm Zenith TX2 device by Cook Medical was deployed with both proximal and distal landing beyond the edges of the pre-existing stent-graft. The proximal landing partially covered the left common carotid artery origin, while the distal landing was in the descending aorta at approximately T8 vertebral level. The new stent-graft was expanded using balloon angioplasty which initially showed wasting against the previous stent-graft. Following several attempts to expand the stent-graft, the post-completion angiogram showed a widely patent aortic lumen as demonstrated in Figure 3. All lower limb pulses were immediately palpable post-operatively. The patient was discharged on aspirin monotherapy with a plan for ongoing follow-up with CTA surveillance to ensure the durability of the repair.
The patient’s hypertension unusually remained refractory requiring four agents for control, despite a widely patent graft on follow up imaging. A full secondary hypertension screen was performed looking for renal, endocrine, and metabolic causes which was negative. Specialised imaging in the form of radioisotope renography and renal artery duplex ultrasonography also showed no abnormalities. The reason for ongoing hypertension remains somewhat of a mystery, however, may be related to haemodynamic changes from the implanted aortic stent-graft.
Discussion
The initial stent-graft used in our patient was the Zenith Alpha stent-graft by Cook Medical. This device has had recurrent reports of delayed thrombus formation, which eventually led to the manufacturer removing BTAI as a suggested indication from the IFU on the 22nd of June 2017 (which was after the date of deployment in our patient). Additionally, there was a recall of the stent-graft sizes between 18 mm and 22 mm. The likely cause for this complication has only recently been described in the TRANSFIX study. 2 The study was designed to investigate the safety of the Zenith Alpha device prospectively over five years in a cohort of 50 patients. The study found that 15 of its 50 patients (30%) developed delayed thrombosis of the distal aspect of the stent-graft, particularly in younger patients. None of the patients in the study were reported to be symptomatic from this, with a single patient undergoing re-intervention prophylactically in a similar fashion to our patient with relining using a Zenith TX2 stent-graft. The proposed mechanism for the complication was a design flaw where the distal aspect of the stent-graft developed infolding of the graft material under the stent edge. This infolding was particularly exacerbated in younger patients for two reasons; firstly, the stent-grafts were usually more oversized due to the patients’ small calibre aortas and secondly, younger patients have more tapering of the descending aorta distally. Both these factors were of relevance in our patient.
Contrary to the patients in the TRANSFIX study, our patient developed a high-grade lesion with significant clinical complications. There are a few other reported cases in the literature of TEVAR use for BTAI, which were later complicated by thrombosis of the stent-graft and leading to severe distal malperfusion. 3-8 It is important to note that only one these other cases had a Zenith Alpha stent-graft in-situ, 6 with the other cases reporting use of a variety of different thoracic aortic stent-grafts.
Open surgical repair is the most reported technique for the management of distal TEVAR stenotic or occlusive lesions. This involves either in-situ reconstruction of the thoracic aorta or with extra-anatomical bypass using an axillobifemoral bypass. 3-5, 8 In addition to the patient described in the TRANSFIX study, there are two other reports of endovascular management with a re-lining TEVAR; Hostalrich et al 6 described use of an Optimed bare-nitinol-stent and Marino et al 7 described use of Medtronic Valiant Captiva stent-graft. Both had successful outcomes, however, Marino et al described distal lower extremity thromboembolism in their patient post-operatively. We elected for an endovascular first approach as well due to the obvious reduced morbidity and mortality. The stent-graft we used was the Zenith TX2 by Cook Medical which is a stainless-steel stentgraft that has superior radial strength. It has been reported to have lower rates of device collapse and thought to be better suited for healthy aortas in young patients. 9 Intravascular ultrasound would have been a useful ancillary tool both in terms of assessment of the initial injury and in assisting with deployment of the stent-graft in the initial and follow-up procedures; however, was unavailable to our unit at the time. Instead, intra-operative TOE was used in the follow-up procedure to confirm cannulation of the true lumen which may not have been possible with fluoroscopy alone.
In the short term, the outcome of endovascular repair for the complication was successful, however given our limited exposure to this problem in addition to the lack of literature reporting on use of this technique makes us wary about the long-term durability of endovascular relining. We will continue to closely follow up the patient with ongoing CTA, potentially transitioning to a different modality such as magnetic resonance imaging or echocardiography down the track.
Conclusion
Based on the literature, thrombosis of TEVAR stent-grafts is probably more common than is currently appreciated. It is important that there is awareness regarding this complication with its propensity to cause critical stenosis or occlusion of these stent-grafts. This is particularly relevant in patients who have had previous Zenith Alpha devices for BTAI and we would suggest if other departments have such patients, to closely follow them up with serial imaging.
Declarations
All authors were involved in the conception, literature review and writing of the article.
The authors declare that there are no conflicts of interests and there was no external funding or grants used for the writing of this manuscript.
There are no acknowledgements. The patient who is the subject of the manuscript has provided informed, written consent for publication of the manuscript and the associated images.
References
- Khoynezhad A, Azizzadeh A, Donayre C, Matsumoto A, Velazquez O, White R (2013). Results of a multicenter, prospective trial of thoracic endovascular aortic repair for blunt thoracic aortic injury (RESCUE trial). J Vasc Surg. 57: 899-905.
[Crossref], [Google Scholar]
- Starnes B, Dwivedi A, Giglia J, Woo K, Yeh C (2020). Updated outcomes from the TRANSFIX study to evaluate endovascular repair of blunt thoracic aortic injuries with the Zenith Alpha thoracic device. J Vasc Surg. 71: 1851-1857.
[Crossref], [Google Scholar]
- Abdoli S, Ham S, Wilcox A, Fleischman F, Lam L (2017). Symptomatic intragraft thrombus following endovascular repair of blunt thoracic aortic injury. Ann Vasc Surg. 42: 305.e307-305.e312.
[Crossref], [Google Scholar]
- Alvarez B, Constenla I, Maeso J, Matas M (2009). Late thrombosis of a thoracic aorta stent graft. J Vasc Surg. 49: 119-129.
[Crossref], [Google Scholar]
- Fernadez V, Metres G, Maeso J, Dominguez J, Aloy M, Matas M (2010). Endovascular treatment of traumatic thoracic aortic injuries: short- and medium-term follow up. Ann Vasc Surg. 24: 160-166.
[Crossref], [Google Scholar]
- Hostalrich A, Canaud L, Ozdemir B, Chaufour X (2019). Severe thoracic aorta stenosis after endovascular treatment of blunt thoracic aortic injury. Semin Thorac Cardiovasc Surg. 31: 227-229.
[Crossref], [Google Scholar]
- Marino M, Kasemi H, Martinelli O, Bresadola L, Salvatori F, Irace L (2013). Re-TEVAR for complications after blunt aortic traumatic injury stenting. Cardiovasc Intervent Radiol. 37: 519-522.
[Crossref], [Google Scholar]
- Reich H, Margulies D, Khoynezhad A (2014). Catastrohic outcome of de novo aortic thrombus after stent grafting for blunt thoracic aortic injury. Ann Thor Surg. 98: 139-141.
[Crossref], [Google Scholar]
- Jonker F, Schlosser F, Geirsson A, Sumpio B, Moll F, Muhs B (2010). Endograft collapse after thoracic endovascular aortic repair. J Endovasc Ther 17: 738-743.
[Crossref], [Google Scholar]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences