Endovascular Treatment of Type 1a Endoleak after Treatment of Suspending Rupture of Bilateral Internal Iliac Aneurysms for Preserving the Inferior Mesenteric Artery
Yoshiaki Yajima, Hiroto Kitahara, Satoshi Hoshino and Atsushi Bito
DOI10.21767/2573-4482.100057
Yoshiaki Yajima1*, Hiroto Kitahara1, Satoshi Hoshino1 and Atsushi Bito2
1Department of Cardiovascular Surgery, Matsumoto Kyoritsu Hospital, Nagano, Japan
2Department of Cardiovascular Surgery, Kikuna Memorial Hospital, Kanagawa, Japan
- *Corresponding Author:
- Yoshiaki Yajima
Department of Cardiovascular Surgery
Matsumoto Kyoritsu Hospital
9-26 Habaue Matsumoto
Nagano, 3908505, Japan
Tel: 81-263-35-5333
Fax: 81-263-36-0370
E-mail: YajimaY@chushin-miniren.gr.jp
Received Date: August 10, 2017; Accepted Date: August 22, 2017; Published Date: August 28, 2017
Citation: Yajima Y, Kitahara H, Hoshino S, Bito A (2017) Endovascular Treatment of Type 1a Endoleak after Treatment of Suspending Rupture of Bilateral Internal Iliac Aneurysms for Preserving the Inferior Mesenteric Artery. J Vasc Endovasc Surg. 2:24. doi: 10.21767/2573-4482.100057
Abstract
An 86-year-old man presented with lower abdominal pain. Enhanced CT revealed large bilateral internal iliac arterial aneurysms. After embolization of the bilateral internal iliac arteries, leg type stent grafts were implanted. 1 month later an enhanced CT showed a type 1a endoleak, so additional endovascular treatment was necessary. A bifurcated type stent graft was lowered into the terminal aorta to bail out the inferior mesenteric artery. The type 1a endoleak disappeared, nor were complications. The use of this simple and easy technique can prevent serious and fatal complications after bilateral internal iliac artery embolization.
Keywords
Endovascular arterial repair; Endoleak; Pelvic organ ischemia; Ischemic colitis
Introduction
The endovascular treatment of iliac aneurysms by Stent Graft (SG) is gaining popularity because of its low invasiveness and good results. In this case, a type 1a endoleak appeared after endovascular treatment with a leg type SG for the suspending rupture of both sides of the Internal Iliac Artery Aneurysms (IAAAs). The Inferior Mesenteric Artery (IMA) was preserved and a bifurcated type SG was implanted without complications such as intestinal tract ischemia.
Case Report
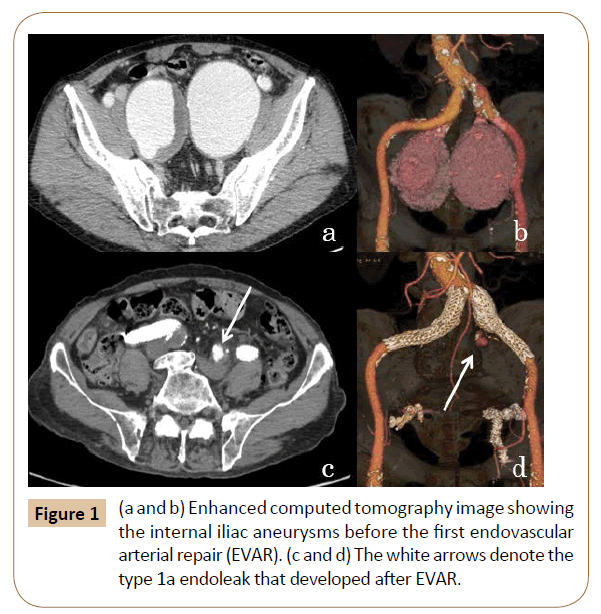
An 86-year-old man with a history of Ca blocker use for hypertension was referred to our institution for the treatment of bilateral IIAAs. He noticed hematuria and lower abdominal pain a few days prior for which he saw a nearby doctor. He visited our emergency room for the treatment of huge aneurysms detected by abdominal ultrasonography. On an enhanced CT view of both sides of the IAAAs and physical exam, suspending rupture was diagnosed and endovascular treatment was chosen. Enhanced CT showed that the right IAAA was 63 × 75 mm in diameter and the left IAAA was 71 × 85 mm in diameter. The first plain CT showed high density of the vascular wall of the right IAAA was almost identical to the suspending rupture. First, the peripheral arteries of the bilateral IIA were embolized by vascular plugs and coils (AMPLATZERTM Vascular Plug II (9- AVP2-010, St. Jude Medical, St Paul, MN, USA; AMPLATZERTM Vascular Plug4, 9-AVP038-008, St. Jude Medical, St Paul; TORNADO, COOK® Medical Incorporated, Bloomington, IN, USA ). A leg type SG (Excluder®, PLC201000J, W.L. Gore & Associates, Flagstaff, Az, USA) was implanted. The proximal end of the SG was positioned on the right CIA and the peripheral end was positioned on the right EIA, so blood was interrupted into the right IIAA. Similarly, the leg type SG (Excluder®, PLC231000J, Gore & Associates) was implanted, interrupting the blood flow into the left IIAA. A contrasting CT showed a type 1a endoleak to a left IAAA, so an aortic extender (Excluder® PLA230300J, W.L. Gore & Associates) was also implanted in the left CIA and the physical signs of the aneurysm disappeared. However, an additional treatment was necessary because a postoperative enhanced CT showed another type 1a endoleak on the proximal side of the left IAAA with a length of 51 mm from the IMA to the terminal aorta (TA) (Figure 1).
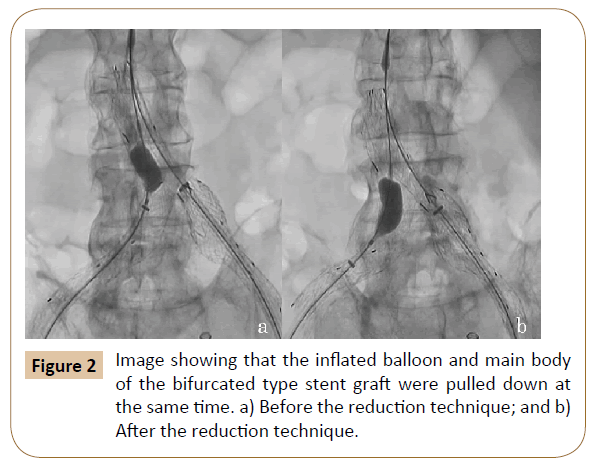
The operation was performed under general anesthesia. A 26 × 14 × 140 mm bifurcated type SG (Excluder®, RLT261414J, Gore WL & Associates) was chosen. The main trunk of the SG was 40 mm and the distance from the IMA to the TA was around 50 mm, meaning sufficient distance to implant the SG and preserve the IMA. From the left femoral artery through an 18Fr sheath (GORE® DrySeal sheath DSL1828J, W.L. Gore & Associates), the bifurcated type SG was inserted and the proximal side was deployed. From the right femoral artery through a 12Fr sheath (GORE® DrySeal sheath DSL1228J, W.L. Gore & Associates), a balloon (TMP SG balloon®, Tokai Medical Products Inc., Aichi, Japan) was inflated in the contralateral gate of the SG. The constraining dial was turned to close the proximal side of the main body. The inflated balloon and the main body of the SG were pulled down when the contralateral gate of the SG was pulled down into the right CIA, pulling the main trunk down to preserve the IMA (Figure 2). From the right femoral artery through a 12Fr sheath, a contralateral leg type SG (Excluder® PLC201000J, W.L. Gore & Associates) was implanted and ballooned. After confirmation of the preserved IMA blood flow and no endoleak, the operation was finished (Figure 2).
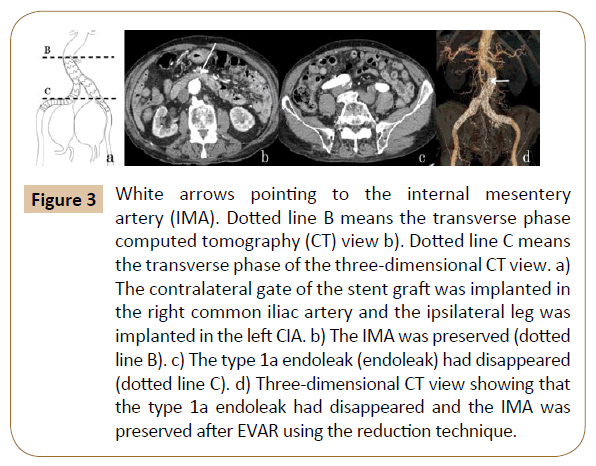
The postoperative enhanced CT also showed that the type 1a endoleak had disappeared and the IMA was preserved (Figure 3). The case made good progress without dilation of the aneurysm or complications such as claudication or intestinal tract ischemia.
Figure 3: White arrows pointing to the internal mesentery artery (IMA). Dotted line B means the transverse phase computed tomography (CT) view b). Dotted line C means the transverse phase of the three-dimensional CT view. a) The contralateral gate of the stent graft was implanted in the right common iliac artery and the ipsilateral leg was implanted in the left CIA. b) The IMA was preserved (dotted line B). c) The type 1a endoleak (endoleak) had disappeared (dotted line C). d) Three-dimensional CT view showing that the type 1a endoleak had disappeared and the IMA was preserved after EVAR using the reduction technique.
Discussion
In the surgical treatment for abdominal aortic aneurysm, including open surgery and endovascular arterial repair (EVAR), pelvic organ ischemia may occur and complications such as colon ischemia after EVAR occur at an approximate 6% frequency [1]. Certainly the precise etiology of ischemic colitis is still unclear during EVAR, but we cannot deny the idea that both sides of the IAA embolization would increase the possibility of pelvic organ ischemia [2,3]. It is especially necessary to prevent complications related to IIA embolization using EVAR because they can be serious or fatal [4]. Colonic ischemia is caused by intraoperative embolisms and reduced intestinal tract perfusion, the latter of which is mainly caused by interruption of the IMA and IIAs resulting in reduced circulation blood volume, vessel spasm, and reperfusion [1,5,6]. In open surgery, it is recommended that the IMA be rebuilt in cases after IAA embolization to prevent colic ischemia. In cases of a revascularized IMA, the risk of colon ischemia is decreased and the death rate significantly decreases [7].
In EVAR treatment, the IMA is usually embolized and the IIA often functions as a collateral circulation road for the left half of the colon. It is reported that in cases after interruption of the IMA and bilateral IIAs, the ipsilateral sides of the EIA and the deep femoral artery function as collateral vessels [8], but it is thought that when the bilateral IIAs must be interrupted, the IMA should be preserved whenever possible to prevent complications such as colon ischemia, since the development of collateral vessels would require significant time [7,9].
The “kissing stent graft technique” using the leg type SG is reportedly [9] a simple and easy technique for preserving the IMA in EVAR treatment, but it is possible that additional treatments would be limited if the endoleak occurred in the future. The “aortoiliac coverter” [10] and “snorkel” [11] techniques were also reported, but these are relatively complicated. Therefore, at first, the simpler and easier “upside down” technique to implant leg type SG reversely was used, but a type 1a endoleak occurred due to an insufficient landing zone. Therefore, the “reduction” technique was additionally used to insert the bifurcated type SG. The bifurcated type SG (Excluder) was chosen because the length of the main trunk of the SG was short and the proximal SG could be closed after deployment into the main trunk. Additionally, the position of the SG was changeable, allowing preservation of the IMA. This technique does not involve more complicated maneuvers, and additional treatments for endoleak are easily performed. This technique would be most suitable for additional treatment of type 1a endoleak as in this case. However, the use of this technique damages or embolizes shaggy aortas or arteriosclerotic vessels because the SG is moved downward. Therefore, we recommend the use of the reduction technique in cases in which vessels are in structurally good shape.
Conclusion
Use of the easy and simple reduction technique, which does not limit additional treatments for future endoleak, enabled the bifurcated type SG implantation to preserve the IMA. The case progressed well without serious or fatal complications such as ischemic colitis that are sometimes seen with EVAR.
References
- Dadian N, Ohki T, Veith FJ (2001) Overt colon ischemia after endovascular aneurysm repair: the importance of micro embolization as an etiology. J Vasc Surg 34: 986-996.
- Saengprakai W, van Herwaarden JA, Georgiadis GS (2017) Clinical outcomes of hypogastric artery occlusion for endovascular aortic aneurysm repair. Minim Invasive Ther Allied Technol 24: 1-10.
- Takei Y, Ogata K, Ogata K (2014) EVAR in which the bilateral limbs extended into the external iliac arteries. J Vasc Surg 23: 899-903.
- Lin PH, Chen AY, Vij A (2009) Hypogastric artery preservation during endovascular aortic aneurysm repair: is it important? Semin Vasc Surg 22: 193-200.
- Bjorck M, Wanhainen A (2010) Nonocclusive mesenteric hypoperfusion syndromes: recognition and treatment. Semin Vasc Surg 23: 54-64.
- Elder K, Lashner BA, Al Solaiman F (2009) Clinical approach to colonic ischemia. Cleve Clin J Med 76: 401-409.
- Seeger JM, Coe DA, Kaelin LD (1992) Routine re-implantation of patent inferior mesenteric arteries limits colon infarction after aortic reconstruction. J Vasc Surg 15: 635-641.
- Sugano N, Inoue Y, Iwai T (2003) Evaluation of buttock claudication with hypogastric artery stump pressure measurement and near infrared spectroscopy after abdominal aortic aneurysm repair. Eur J Vasc Endovasc Surg 26: 45-51.
- Ishizaka T, Watanabe M, Higashide T (2013) endovascular treatment of bilateral isolated iliac artery aneurysm with a kissing stent graft for preservation of the inferior mesenteric artery. Japanese Society for Vascular Surgery 22: 993-996.
- Katsikas VC, Dalainas I, Martinakis VG (2012) The role of aorto uniiliac devices in the treatment of aneurysmal disease. Eur Rev Med Pharmacol Sci 16: 1061-1071.
- Igari K, Kudo T, Mori K (2013) Two cases of successful inferior mesenteric artery preservation with bare metal stent in endovascular iliac artery aneurysm repair. Ann Vasc Dis 6: 674-677.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences