Intravascular Lithotripsy Assisted Carotid Stent Expansion
Veena Mehta1* and Mathew Wooster2
1Department of Vascular Surgery, Medical University of South Carolina College of Medicine, Charleston, SC, USA
2Department of Vascular Surgery, Medical University of South Carolina Division of Vascular Surgery, Charleston, SC, USA
- *Corresponding Author:
- Veena Mehta
Department of Vascular Surgery, Medical University of South Carolina College of Medicine, Charleston, SC, USA
E-mail:mehtav@musc.edu
Received date: 03 January, 2022, Manuscript No. IPJVES-22-12511; Editor assigned date: 05 January, 2022, PreQC No. IPJVES-22-12511(PQ);
Reviewed date: 17 January, 2022, QC No IPJVES-22-12511; Revised date: 24 January, 2022, Manuscript No. IPJVES-22-12511(R);
Published date: 31 January, 2022, DOI: 10.36648/2634-7156.7.1.4602
Citation: Mehta V, Wooster M (2022). Intravascular Lithotripsy Assisted Carotid Stent Expansion. Int J Vasc Endovasc Therapy Vol.7 No.1:4602
Abstract
Carotid stenting has been demonstrated to effectively reduce the risk of stroke in appropriately selected patients. However, application of carotid artery stenting remains limited in the setting of heavily calcified disease. We present here three patients, who were treated with intravascular lithotripsy of the internal and common carotid arteries. All three patients recovered uneventfully and have demonstrated excellent stent expansion on surveillance imaging. Intravascular lithotripsy is an effective adjunct for enabling stent expansion in heavily calcified lesions and can be employed for treatment of high risk carotid lesions that would otherwise be poor endovascular candidates.
Keywords
Carotid stenosis; Intravascular lithotripsy; Transcarotid artery revascularization; Transfemoral carotid stenting; Cerebrovascular disease; Arterial calcification
Introduction
Endovascular management of carotid artery stenosis with carotid stenting is particularly useful in patients with higher lesions that are surgically inaccessible via an open approach, patients with prior neck radiation or surgery, and elderly patients with multiple medical comorbidities [1,2]. However, one significant limitation of carotid artery stenting remains patients with heavily calcified atherosclerosis, as this may prevent adequate expansion of the stent. In coronary and infrainguinal disease, atherectomy has been utilized extensively for overcoming the challenges calcium poses [3-6], but this comes with a risk of embolization that is not acceptable in cerebrovascular intervention [7,8]. More recently, intravascular lithotripsy was first successfully described for use in heavily calcified femoropopliteal arteries [9]. These percutaneous devices are derived from established therapy for renal and ureteral calculi and adapted to produce ultrasonic pressure waves to induce microfractures in the calcium, improving the ability to expand the lesion with angioplasty. This diminishes the risks of embolization relative to atherectomy, leading to interest in its use for calcified carotid lesions [10-12].
Methods
We present three cases in which intravascular lithotripsy was used to successfully treat carotid artery lesions: Prior to transfemoral stenting, prior to Transcarotid Artery Revascularization (TCAR), and post stenting with an under-expanded stent. Patients were deemed high risk endarterectomy candidates by a multidisciplinary team and offered endovascular intervention via transfemoral or transcarotid approach at the surgeon's discretion. All patients were informed of the intended off-label use of the intravascular lithotripsy for their procedures and consented accordingly.
Results
Patient 1
An 82 year old woman with history of symptomatic left carotid artery stenosis treated with left carotid TCAR presented for a follow up appointment 8 months later. Despite compliance with her daily aspirin, clopidogrel and atorvastatin, her carotid artery duplex at this time showed elevated velocities with Peak Systolic Velocity (PSV) of 332 cm/s, consistent with 70%-79% stenosis. She remained asymptomatic. Further evaluation using CT angiogram of head and neck also showed >70% stenosis by NASCET criteria and suggested under expansion of the stent rather than in-stent restenosis. Given that her primary repair was a TCAR and this would have been a redo exposure, we felt that transfemoral approach would be the safer option.
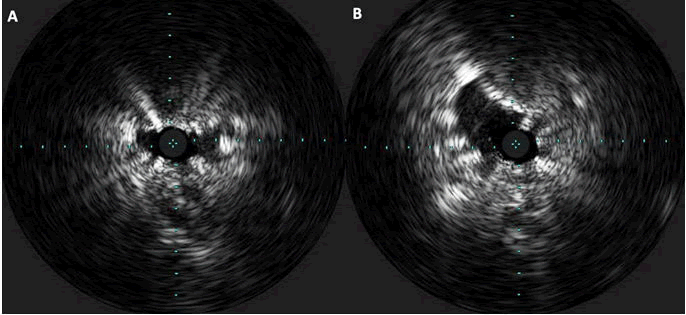
Under local anesthesia, a transfemoral approach was used to advance a 6 French sheath into the distal left common carotid artery. The lesion was crossed with an embolic protection device (Abbott Medical Nav6 Emboshield filter), which was deployed distal to the stent into a straight segment of the left internal carotid artery. Intravascular Ultrasound (IVUS) confirmed near occlusion of the stent secondary to under-expansion with mild in stent restenosis (Figure 1). We treated this segment with 5 × 60 intravascular lithotripsy balloon for 3 rounds of lithotripsy at 6, 8 and 10 atmospheres. IVUS still demonstrated significant stenosis, so we performed higher pressure angioplasty with high pressure balloon (Mustang) with angiographic resolution of the waist at 18 atmospheres. Following this treatment, IVUS showed approximately 30% residual stenosis. However, given the prolonged time intervening within the carotid segment, we decided against further angioplasty. Minimal emboli were seen in the filter upon removal.
In follow-up at 15 months postoperatively, she remains asymptomatic and endorses compliance with daily aspirin, statin and clopidogrel. Carotid artery duplex has continued to demonstrate improved stent expansion, with approximately 16%-49% stenosis of the stent (PSV 204 cm/s, EDV 39 cm/s), consistent with intraoperative findings.
Patient 2
A 60 year old woman admitted for decompensated heart failure secondary to cardiomyopathy (left ventricular ejection fraction of 25%) underwent Cardiac catheterization showing multi-vessel disease in left anterior descending artery, left circumflex artery, and right coronary artery. Based on these findings, she underwent workup for coronary bypass, during which she was found to have right Internal Carotid Artery (ICA) occlusion and left ICA stenosis of >70%. Medical history was significant for hypertension, hyperlipidemia, chronic obstructive pulmonary disease, and type 2 diabetes and prior neck surgery. Given her significant cardiac disease, prior low neck dissection, and a type 1 arch, we felt she would be best served with transfemoral carotid stenting. However, due to heavy calcific burden at both the ICA and a focal Common Carotid Artery (CCA) origin lesion, we planned to perform adjunctive intravascular lithotripsy prior to her stent placement. Given her severe congestive heart failure and body habitus, she was unable to lay flat enough with her head turned sufficiently to perform TCAR safely. Therefore, we opted to proceed with transfemoral carotid stenting for shorter operative duration and improved ergonomics for the patient.
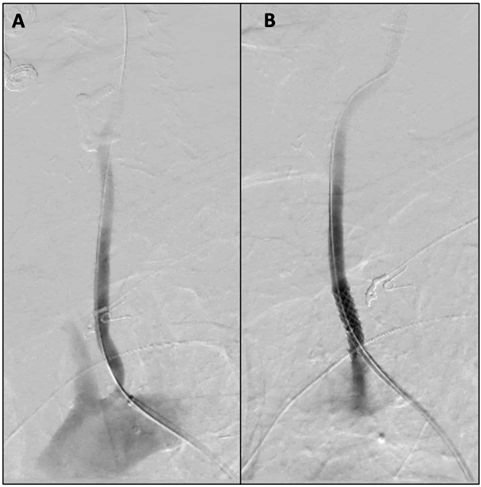
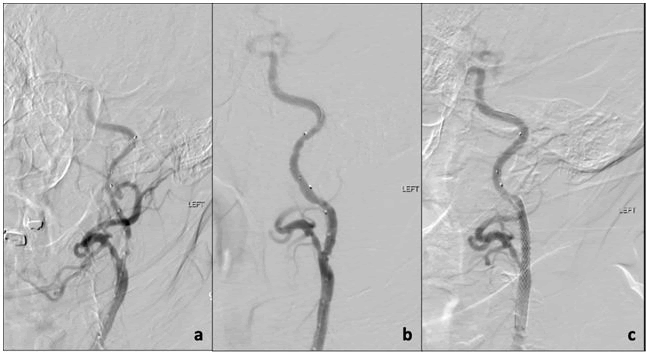
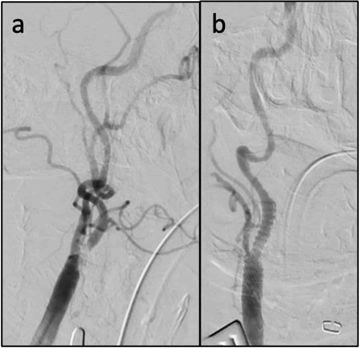
Under local anesthesia, a transfemoral approach was used to advance a 7 French sheath into the common carotid artery. A 7 × 29 balloon expandable stent (Gore VBX) was placed at the common carotid lesion, and we then advanced the sheath to the mid common carotid artery (Figure 2). The lesion was crossed, and a spider filter (medtronic medical) was deployed into the straight segment of the internal carotid artery. After two rounds of lithotripsy at 4 and 6 atmospheres with 5 × 60 balloon the angiographic waist was resolved. We then deployed a 10 × 31 self-expanding metal stent (wallstent), and the filter was retrieved with minimal emboli present. Completion angiography was performed showing patent stent in the internal carotid artery with measured residual stenosis <30% (Figure 3).
She successfully underwent coronary artery bypass grafting two days after carotid stenting without any major complications. At two-month follow-up, she remains asymptomatic and endorses compliance with daily aspirin, statin, and clopidogrel. Surveillance carotid duplex continues to demonstrate wide patency of the internal carotid artery stent without evidence of significant stenosis (PSV 109 cm/s, EDV 39.5 cm/s).
Patient 3
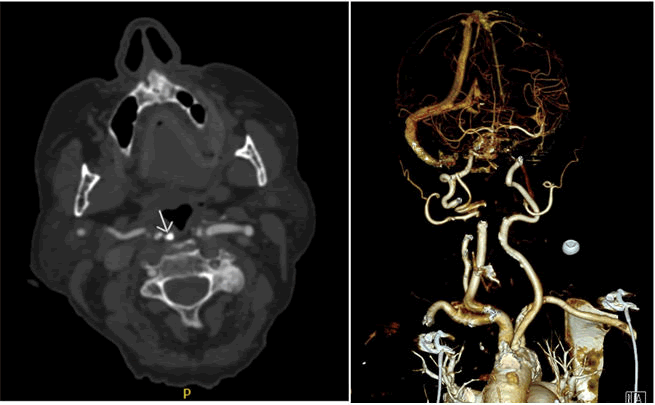
An 86 year old woman with a known history of 70% right sided carotid artery stenosis presented with six weeks of intermittent left sided facial droop and blurry vision, slurred speech, and difficulty swallowing. Imaging at an outside hospital showed progression to 95% stenosis of her right carotid artery (Figure 4). Past medical history included atrial fibrillation (on rivaroxaban), coronary artery disease, peripheral artery disease and hypothyroidism. Surgical history was significant for multiple vascular interventions including aorta bifemoral bypass, left femoral-popliteal bypass requiring re-intervention, and left groin pseudoaneurysm repair, making her groins inhospitable. We found that her lesion was retropharyngeal and high, at the level of C2, making it difficult to exposure surgically. Due to her multiple comorbidities and heavy calcification, we felt that her stenosis would be best treated with TCAR with pre-emptive intravascular lithotripsy.
Under general anesthesia with cerebral oximetry for neurologic monitoring, the common carotid artery was exposed and standard TCAR procedure ensued. Under flow reversal, two rounds of lithotripsy were performed at 4 and 6 atmospheres using 4 mm × 40 mm balloon. While cerebral oximetry remained appropriate, there was significant bradycardia despite administration of atropine. Of note, she had not been pre-treated with atropine or glycopyrrolate. At this point, angiogram demonstrated significant improvement in the lesions (Figure 5) so a third round was not performed. A 7 × 30 nitinol carotid stent (Precise) was deployed and the remainder of the TCAR procedure completed according to the standard protocol. Final measured stenosis after stenting was <30%. Postoperatively, she did not experience any further episodes of bradycardia requiring treatment. Her preoperative symptoms of facial droop and blurry vision completely resolved after stenting.
She continued to do well at two-month follow-up visit without any neurologic sequelae. She continues to be compliant with daily rivaroxaban and ticagrelor. Carotid artery duplex at this time demonstrated end stent peak systolic velocities of 645 cm/s, consistent with 80%-99% stenosis, although the study was noted to be technically difficult due to labored breathing and tortuous arteries. Unfortunately, she was lost to further follow-up, and we were unable to obtain other imaging for further evaluation.
Discussion
Despite the embolic risks associate with peripheral atherectomy [7,13], intravascular lithotripsy has gained interest for treating patients with heavily calcified carotid arteries who are poor surgical candidates for endarterectomy as well as poor stenting candidates. However, there are some limitations to the use of this device. As demonstrated in Patient 3, carotid baro-receptor stretch during angioplasty can be associated with significant bradycardia or asystole. Traditionally, carotid stenting balloon inflations are rapid, and a single inflation is used due to embolic risk [14]. However, lithotripsy requires 30-second-long inflations per round and may require multiple rounds to achieve low pressure expansion of the calcium. An additional challenge as seen in patient 1 comes in the pressure requirements, as some lesions will not give at the 10 atmosphere rated burst pressure. This requires an additional catheter exchange and inflation with a higher-pressure balloon.
Finally, the current balloon lengths and delivery system complicate the procedure. The standard TCAR procedure is performed with a 95 cm guidewire while most transfemoral stenting is performed with 190 cm filter wires (though 300 cm length are routinely used by some practitioners). The peripheral S4/M5 balloons are on 135 cm/110 cm over the wire delivery shafts, forcing practitioners to intentionally cross with a different wire than their usual practice-this does not truly change the procedure but must be born in mind when using this technology. The S2 coronary balloon is rapid exchange, but it is only offered in a maximum diameter of 4 mm with a length of 12 mm, too short for most carotid lesions. The M5 balloons range up to 7 mm diameter but are all 60 mm in length. For most TCAR procedures the sheath tip is less than 4 cm from the carotid bifurcation forcing the balloon to extend higher into the internal carotid artery than most practitioners would typically prefer. The S4 is 40 mm length but only comes in up to 4 mm diameter. For transfemoral stenting the length is less of an issue as the sheath can be left further away from the carotid bulb, but this does increase the risk of sheath kicking back into the aorta. Finally, for the 6.5 mm -7 mm balloon diameter, a 7 Fr sheath is required while most transfemoral stenting is performed through a 6 Fr requirement. It is uncommon to use such a large balloon for the internal carotid artery, but should it be required it is important to identify this pre-procedurally to ensure an adequately size sheath is advanced. It is important to note that this remains an off-label use of technology.
Conclusion
Carotid endarterectomy and TCAR continue to remain the treatment of choice for carotid disease. For otherwise no-option patients, there is potential for intravascular lithotripsy to expand the use of carotid stenting. However, caution must be taken in patient selection and careful review of required modification to the standard transfemoral or transcarotid approaches must be made in advance.
References
- Lamanna A, Maingard J, Barras CD, Kok HK, Handelman G, et al. (2019) Carotid artery stenting: Current state of evidence and future directions. Acta Neurologica Scandinavica 139: 318-333. [Crossref], [Google Scholar], [Indexed]
- Dakour-Aridi H, Kashyap VS, Wang GJ, Eldrup-Jorgensen J, Schermerhorn ML, et al. (2020) The impact of age on in-hospital outcomes after transcarotid artery revascularization, transfemoral carotid artery stenting, and carotid endarterectomy. J Vasc Surg 72: 931-942e2. [Crossref], [Google Scholar], [Indexed]
- Chambers JW, Behrens AN, Martinsen BJ (2016) Atherectomy devices for the treatment of calcified coronary lesions. Interv Cardiol Clin 5: 143-151. [Crossref], [Google Scholar], [Indexed]
- Kübler P, Zimoch W, Kosowski M, Tomasiewicz B, Rakotoarison O, et al. (2018) The use of rotational atherectomy in high-risk patients: Results from a high-volume centre. Kardiol Pol 76: 1360-1368. [Crossref], [Google Scholar], [Indexed]
- Beohar N, Kaltenbach LA, Wojdyla D, Pineda AM, Rao SV, et al. (2020) Trends in usage and clinical outcomes of coronary atherectomy. Circ Cardiovasc Interv 13: e008239. [Crossref], [Google Scholar], [Indexed]
- Minko P, Katoh M, Jaeger S, Buecker A (2011) Atherectomy of heavily calcified femoropopliteal stenotic lesions. J Vasc Interv Radiol 22: 995-1000. [Crossref], [Google Scholar], [Indexed]
- Azar Y, DeRubertis B, Baril D, Woo K (2018) Atherectomy-Associated complications in the southern california vascular outcomes improvement collaborative. Ann Vasc Surg 49: 241-246. [Crossref], [Google Scholar], [Indexed]
- Harrington RA, Lincoff AM, Califf RM, Holmes DR, Berdan LG, et al. (1995) Characteristics and consequences of myocardial infarction after percutaneous coronary intervention: Insights from the coronary angioplasty versus excisional atherectomy trial (CAVEAT). J Am Coll Cardiol 25: 1693-1699. [Crossref], [Google Scholar], [Indexed]
- Brodmann M, Werner M, Brinton TJ, Illindala U, Lansky A, et al. (2017) Safety and performance of lithoplasty for treatment of calcified peripheral artery lesions. J Am Coll Cardiol 70: 908-910. [Crossref], [Google Scholar], [Indexed]
- Brodmann M, Werner M, Holden A, Tepe G, Scheinert D, et al. (2019) Primary outcomes and mechanism of action of intravascular lithotripsy in calcified, femoropopliteal lesions: Results of Disrupt PAD II. Catheter Cardiovasc Interv 93: 335-342. [Crossref], [Google Scholar], [Indexed]
- Giannopoulos S, Speziale F, Vadalà G, Soukas P, Kuhn B, et al. (2021) Intravascular lithotripsy for treatment of calcified lesions during carotid artery stenting. J Endovasc Ther 28: 93-99. [Crossref], [Google Scholar], [Indexed]
- Henry CL, Hansen SK, Gable CE, Grimsley BR, Gable DR (2021) Intravascular lithotripsy during transcarotid arterial revascularization for highly calcified lesions in high-risk patients. J Vasc Surg Cases Innov Tech 7: 68-73. [Crossref], [Google Scholar], [Indexed]
- Ochoa Chaar CI, Shebl F, Sumpio B, Dardik A, Indes J, et al. (2017) Distal embolization during lower extremity endovascular interventions. J Vasc Surg 66: 143-150. [Crossref], [Google Scholar], [Indexed]
- Jordan WD, Voellinger DC, Doblar DD, Plyushcheva NP, Fisher WS, et al. (1997) Microemboli detected by transcranial Doppler monitoring in patients during carotid angioplasty versus carotid endarterectomy. Cardiovasc Surg 7: 33-38. [Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences