Postraumatic Pseudoaneurysm of Common Carotid Artery After Penetrating Trauma : Diagnosis and Surgical Management
Encalada Palacios Juan, Ojeda Oscar , Barrera Arce David
DOI10.36648/2634-7156.21.6.45
Encalada Palacios Juan1, Ojeda Oscar 2*, Barrera Arce David3
1Cardiovascular Surgeon, Department of Vascular Surgery, Hospital Abel Gilbert Ponton, Guayaquil, Ecuador
2Vascular Surgeon, Department of Vascular Surgery, Hospital Abel Gilbert Ponton, Guayaquil, Ecuador
3Resident of Vascular Surgery, Hospital Teodoro Maldonado, Guayaquil, Ecuador
*Corresponding author: Ojeda Oscar , Vascular Surgeon, Department of Vascular Surgery, Hospital Abel Gilbert Ponton. Guayaquil-Ecuador; E-mail: oscarle1942@gmail.com
Received date: June 9, 2020; Accepted date: August 19, 2021; Published date: August 29, 2021
Citation:Ojeda O (2021) Postraumatic Pseudoaneurysm of Common Carotid Artery After Penetrating Trauma : Diagnosis and Surgical Management. J Vasc Endovasc Ther Vol.6 No.8.
Abstract
According to carotid pathology, we found carotid pseudoaneurysms, which occur in 13% of all carotid injuries. Carotid pseudoaneurysms are considered extremely rare when they are caused by blunt or penetrating trauma, being caused commonly after surgical interventions like carotid endarterectomy. Extensive cervical exposure and the risk of near structure lesions makes the surgical treatment of carotid pseudoaneurysms complex, indeed, cranial nerves lesions are the principal concern as surgical failure.
Methods
We present the case of a 20-year-old man who, after being treated for damage control due to a gunshot penetrating trauma at cervical level, it presents a pulsating mass that increases in the cervical region accompanied by a progressive dysphonia. The diagnosis was made initially with Doppler ultrasonography and confirmed with selective angiography of carotid artery.
Results
We proceeded to control of carotid vessels and resection of pseudoaneurysm and reconstruction with autologous vein patch. We did not use shunt. There were no complications and the patients discharge was in 2 days.
Conclusion
Although open surgery includes a high complexity procedure, it is the treatment of choice in these cases of posttraumatic pseudoaneurysms, endovascular treatment could be an alternative in the therapeutic arsenal, but at the moment, its role in this type of etiologies is not clarified.
Keywords: vascular, trauma, pseudoaneurysm, carotid
Introduction
The Society of Vascular Surgery defines aneurysm as the dilation of the three vascular layers. It could be said that the wall is "bulging" completely. While a pseudoaneurysm occurs mainly by a break in the inner wall (tunica intima) as a result of external influences. This disruption is usually secondary to a traumatic, inflammatory, infectious or iatrogenic cause. (2. 3. 4) Carotid pseudoaneurysms are rare entities, which are described in the series with 13-14% of all carotid artery injury (5), (6). The majority is due to late complications after a carotid endarterectomy, in the US this procedure occupies the third most common cardiovascular interventions of the common carotid arteries (7), the proposed mechanisms have been: rupture and dilatation of the prosthetic patch, partial disruption of the suture line due to infection and mechanical stress (8). Pseudoaneurysms due to trauma are extremely rare and most of them are the result of blunt trauma, while those resulting from penetrating trauma have been less described, although with a growing frequency due to iatrogenic causes after jugular puncture for catheterization (9). The most common localization of aneurysms and pseudoaneurysms is near the bifurcation of the common carotid artery (10). Patients with carotid pseudoaneurysm have a high risk of: neurological complications due to thromboembolism, small risk of rupture with massive hemorrhage as well as neurological or surrounding structures compression (5), (11).
Materials and Methods
The presentation derived from embolic episodes can be: arousal impaired, transient ischemic attack and episodes of retinal ischemia. (11). The treatment most frequently used in the different series has been the reconstruction with autologous vein, the difficulty of the reconstruction is conditioned by the size of the lesion, but also and especially by the location, some cases of endoluminal treatment have been reported, but the scarce literature regarding the subject treated and the lack of long-term results do not allow an objective evaluation of this technique in this specific type of patients, as well as the impossibility of conversion in case of complication during or after the procedure is a great argument against this procedure (5) (12).
We present the case of a 21-year-old man who suffered several gunshot wounds, (Figure 1), on the extremities and one in the mandibular region with a caudal trajectory with involvement of the neck vessels, evidenced by a progressive increase in the cervical perimeter, respiratory distress which requires emergency orotracheal intubation, as well as progressive blood loss with the need for politransfusion.
The patient is taken to emergency surgery where a great blood infiltration of all the tissues is observed, which difficult the differentiation of the structures, abundant bleeding from the jugular vein, and proximal carotid artery and distal veins at the level of the mandibular angle. It is possible to control proximally the carotid but not distally due to the location of the bleeding, which forces damage control with several 5/0 prolene sutures to stop heavy bleeding.
The patient is transferred to the intensive care unit where he satisfactorily recovers from his injuries and then transferred to the conventional room and finally discharged in good condition.
After approximately 3 months, the patient consulted for a left cervical pulsatile mass that has been increasing in size, as well as progressive dysphonia (Figure 2). Doppler ultrasonography was performed, which showed a pulsatile mass with turbulent flow inside it, compatible with pseudoaneurysm. The patient was hospitalized, and a selective left common carotid arteriography was practiced on him which confirm the presence of a pseudoaneurysm at the level of the carotid bifurcation (Figure 3), as well as the presence of the projectile in the posterior cervical part (Figures 4 and 5).
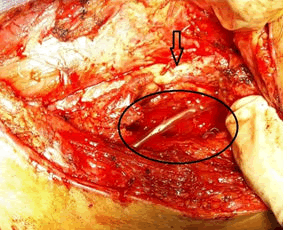
We proceed to surgically intervention with a systemic heparinization. The common carotid is controlled, being difficult the control of internal and external carotid artery because of the size of the pseudoaneurysm and the displacement that this causes, as well as the location near the angle of the mandible (Figure 6).
Therefore, it is decided to dissect the pseudoaneurysm and to digitally control the bleeding through it, after which the control of both internal and external carotid is more easily achieved, and the vascular lesion is demonstrated at the level of the bifurcation, which is repaired with an autologous vein patch. The intervention is performed without arterial shunt (13), approximate clamping time of 40 minutes, drainage is left and then we proceed to closure by planes (8), (14), (15).
The patient was extubated in the operating room without neurological damage, he was discharged on the second day in good conditions. IN the subsequent controls with follow-up at 6 months there is no evidence of nerve structure damage or other type of symptomatology.
Discussion
In the literature, Pseudoaneurysms represent only 14% of the carotid pathology, most of them are the carotid postendarterectomy and secondly the post-traumatic (car accident, penetrating or iatrogenic injuries) (17), (18) with an incidence between 0.02 a 0.4% among all traumatic pseudoaneurysms. The most extensive series are that of the Texas Heart Institute between 1960 and 1995 with 65 cases, however it includes aneurysms and pseudoaneurysms of different etiologies, the different causes, especially traumatic injuries explain the age of this population (19). Alimi et al. identified 155 cases of traumatic injuries of the carotid in a period of 15 years (17), (20). The development of pseudoaneurysms can take from a few hours to several years after the original event. In the United States, approximately 100,000 cases of carotid endarterectomy are reported, of which 0.37% develop post-endarterectomy pseudoaneurysm (1) The pseudoaneurysms show a high incidence of thromboembolic events, and a lower number for rupture with massive hemorrhage or compression of nerve structures (11) (12).
Historically the first successful operation was performed by Sir Astley Cooper in London in 1808 where carotid ligature was performed, in 1970 the reconstruction of the carotid axis replaced the ligature (11,5).
The complication rate compared with the expectant treatment is between 20 to 71%, however, it should be noted that an open surgery is invasive, disabling and extremely difficult when the lesion is near the base of the cranium with high risk of cranial nerve injury (12). This could be the reason why endovascular treatment has recently been used in certain circumstances. (12) Beall et al were the first to report the use of prosthetic graft to replace the carotid artery by aneurysm in 1959. (10) The use of autologous venous spiral grafts is another alternative in vascular reconstruction, especially in those where there is a high risk of contamination. (21) The spiral vein graft technique is as follows. The greater saphenous vein is exposed from the saphenofemoral junction. The vein is handled with care, and its branches are linked. The length of the saphenous vein to be harvested is calculated according to the following formula: The length of the saphenous vein is equal to the diameter of the duct created divided by the average diameter of the saphenous vein multiplied by the length of the space of the carotid artery.
The saphenous vein is removed, irrigated and gently distended with a heparinized saline solution. The vein is divided longitudinally and wrapped around a tube, it can be an endotracheal tube, a 28 French tube will create a 9 mm conduit; A 32 French tube will create a 101/2 mm conduit. Then it is sutured continuously using 7-0 polypropylene until an adequate length of conduit has been built (22).
Doppler ultrasound is the simplest method of investigation but it may fail if the lesion is located high or due to the anatomy of the patient (17) (12). Arteriography provides in most of the cases the diagnosis of the lesion, it specifies the location and detects associated lesions (17). Computed tomography with 3D reconstruction also allows a clear determination of the lesion, its shape and relationship with surrounding structures. Finally magnetic resonance is another option, however this technique requires a long exposure time and it cannot be seen clearly because of the respiratory movements (8), (10), (12). The surgical treatment of pseudoaneurysms requires an approach determined by etiology, size and location as well as comorbidities (6).
Young patients with trauma usually tolerate the clamping while the contralateral carotid is preserved. There is a high incidence of cranial nerve injury, especially in re-intervention, the rates of permanent and transient cranial nerve injuries range between 11-22% and 3-13%, respectively. These complications are especially associated with distal aneurysms of the internal carotid. (12).
The reconstruction is done by the use of autologous vein graft or PTFE patch, always trying to preserve the posterior wall of the artery without injury the nearby nerve structures. (12)
Some cases of endoluminal treatment have been reported but the scarce evidence and the lack of long-term results do not allow an objective evaluation of this technique. (23) According to a study conducted in 2014, 3 cases were performed using the endoluminal technique under local and femoral anesthesia, using a covered stent (24), the first patient underwent previous cervical surgery, while the other two were caused by takayasu syndrome, all of them with comorbidities (5) (12).
The surgical repair of pseudoaneurysms can be achieved with a relatively low mortality rate of 1.2%, a stroke rate of around 10%, and a peripheral neurological damage of about 6%. Long-term follow-up has been reported in very few studies, describing different pathologies after surgical treatment, N Attigah and col, describe a 30-day mortality of 0%. Among the lesions mostly described it involves neurological alterations consistent with temporary hemiplegia, lesions of cranial nerves permanently and temporally. (16)
The long-term follow-up data showed a 7.6% rate of ipsilateral cerebral ischemia, compared to free stroke rates of 96%, 92% and 92% after 5, 10 and 18 years, respectively (12). (25) The satisfactory results of reconstructive surgery justify the aggressive attitude regarding diagnosis and surgical treatment.
Conclusion
Penetrating injuries of the carotid artery have a high morbidity and mortality rate, especially if the "golden hour" is exceeded for trauma care. Carotid pseudoaneurysms are rare and complex entities to treat.
Conventional surgery with repair of the injured vessel, angioplasty with autologous vein patch or prosthesis, bypass and primary repair are valid options to treat this type of trauma. Endovascular treatment, especially the angioplasty with a covered stent is an option that has been used in many hospital, however it has several limitations such as lesions near the bifurcation or in the distal internal carotid, in addition, the damage in adjacent tissues caused for traumas by firearm or stab wounds make the surgery the best option for both vascular and soft tissue repair, bleeding control, etc.
References
- Pourier VEC, Van Laarhoven CJHCM, Vergouwen MDI (2017) Prevalence of extracranial carotid artery. PLoS One 12: 1-8.
- Molina JA, Benito SantamarÃÂa V, Guerrero R, Babun Y (2013) Spectrum of CT Angiography Findings of Pseudoaneurysm. Eur Radiol 1: 1-27.
- Kim HO, Yong BJ, Seung HL, Cheolkyu J, Kyung T, et al. (2012) Cases of Common Carotid Artery Pseudoaneurysm Treated by Stent Graft. Case Reports in Otolaryngology 1-5.
- Peter B, Martin B (2015) True aneurysm in autologous hemodialysis fistulae:definitions, classification and indications for treatment. J Vasc Access 16: 446-453.
- Richard J, Powell, Eva M, Rzucidlo (2003) Stent-graft treatment of a large internal carotid artery vein graft aneurysm. J Vasc Surg 37: 1310-1313.
- Lukla B, Matteo A, Alessandro D T, Pierfranco S, Tiziano T, et al. (2008) Extracranial Internal Carotid Artery Aneurysms: case. Biomed Acta 79: 217-222.
- Christoph K, Andreas K (2018) Patient characteristics and in-hospital outcomes of emergency carotid endarterectomy and carotid stenting after stroke in evolution. J Vasc Surg 1: 1-9.
- Konstantinos P. Donas, Stefan S, Georgios A. Pitoulias, et al. (2009) Surgical outcome of degenerative versus. J Vasc Surg. 49: 93-98.
- Edson Pedroza dos Santos Junior, Rodolfo Rogers Américo Machado Batista et al (2011) Pseudoaneurysm of common carotid due to trauma. J Vasc Bras; 10: 261-265.
- Grant T, Fankhauser, William M (2015) Stone Surgical and medical management of extracranial. J Vasc Bras 61: 389-392.
- Karan G, Caron B, Rockman, Victoria L (2012) Presentation and management of carotid artery. J Vasc Bras 55: 1619-1622.
- Domenico A, Raffaele P, Davide M, Pietro F (2014) Surgical and Endovascular Treatment of Extracranial Carotid Artery Aneurysms. Ann Vasc Surg 28: 659-664.
- Emrah U, Muhammet F S, Emre B, Ã?nsal E (2018) Surgical repair of carotid artery pseudoaneurysm and stenosis in Behçetâ??s disease. Damar Cerrahi Dergisi 27: 51-54.
- .Manuela A, Klaus L, Wolfgang H, Florian E, Julio E A, et al. (2018) Ugurluoglu a. Autologous Bifurcated Carotid Artery Reconstruction: Technique and 2 Year. European Journal of Vascular and Endovascular Surgery : 1-8.
- Norman R, Hertzer (2000) Extracranial carotid aneurysms. J Vasc Bras 31: 823-825.
- Attigah N, Kuèlkens S, Zausig N, Hansmann J, Ringleb P, et al. (2009) Surgical Therapy of Extracranial Carotid Artery Aneurysms: Long-Term Results over a 24-Year Period. Eur J Vasc Surg 37: 127-133.
- Eugenio Rosset, Jean-Noel Albertini, Pierre Edouard Magnan (2000 Surgical treatment of extracranial internal. J Vasc Surg 31: 713-723.
- Gabriel PB, César D, Estela R (2012) Pseudoaneurysm of the Carotid Artery: Severe Complication after Carotid Endarterectomy. Rev Argent Cardiol 80: 471-473.
- Rehana S, Saba S, Parvez A S, Qamar N (2017) Pseudoaneurysm of Left proximal Common Carotid Artery following penetrating trauma. Pak J Med Sci 33: 1291-1293.
- Rafik E S, FRCS (G), Denton A, Cooley (2000) Extracranial carotid artery aneurysms. J Vasc Surg 31: 702-7012.
- Richard J. Fowl, Kevin D. Martin (1988) Use of autologous spiral vein graftsfor vascular reconstructions in contamined fields. J Vasc Surg 8: 442-446.
- Stuart W. Leafstedt, Richard B, Rubenstein (1985) Spiral Saphenous Vein Graft for Replacement of Internal Jugular Vein: A Series of Case Reports. Vasc Dis Manag 828-831.
- Welleweerd JC, den Ruijter HM, Nelissen BGL (2015) Management of Extracranial Carotid Artery Aneurysm. Eur J Vasc Endovasc Surg Surgery 1-7.
- Donald T, Baril, Sharif H, Ellozy, (2004) Endovascular repair of an infected carotid artery pseudoaneurysm. J Vasc Surg 40: 1024-1027.
- Hocine D, Benoît G, Laurent B, Claude L,Valérie B,Valérie B, Lionel A, et al. (2000) Jean Michel Tubiana. MR Angiography for the Long-Term Follow-Up of Dissecting Aneurysms of the Extracranial Internal Carotid Artery. American Roentgen Ray Society 174.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences