The Pathology of Chronic Post-Thrombotic Venous Obstruction is not Chronic Thrombus
Paulo Eduardo Eduardo Ocke Reis and Anthony James Comerota
DOI10.21767/2573-4482.100030
Paulo Eduardo Ocke Reis1* and Anthony James Comerota2
1Department of Specialized and General Surgery, Fluminense Federal University, Rio de Janeiro, Brazil
2Executive Director of Research Jobst Vascular Institute and ProMedica Health System, Toledo, Ohio, USA
- *Corresponding Author:
- Paulo Eduardo Ocke Reis
Department of Specialized and General Surgery
Fluminense Federal University, Rio de Janeiro, Brazil
Tel: +55 21 2629-5000
E-mail: vascular@pauloocke.com.br
Received Date: November 15, 2016; Accepted Date: November 21, 2016; Published Date: November 25, 2016
Citation: Ocke Reis PE, Comerota AJ. The Pathology of Chronic Post-Thrombotic Venous Obstruction is not Chronic Thrombus. J Vasc Endovasc Surg. 2016, 1:4. doi: 10.21767/2573-4482.100030
Editorial
Post-thrombotic venous obstruction is an important contributor to Post-Thrombotic Syndrome (PTS), especially when it involves the common femoral and iliac vein. The term “chronic thrombus” is used commonly to describe the chronic ultrasound findings or even the luminal changes demonstrated by contrast phlebograms. The recent report by Comerota et al. [1] clearly describes the histology of the tissue causing post-thrombotic venous obstruction 7 months to 25 years after the episode of acute thrombosis.
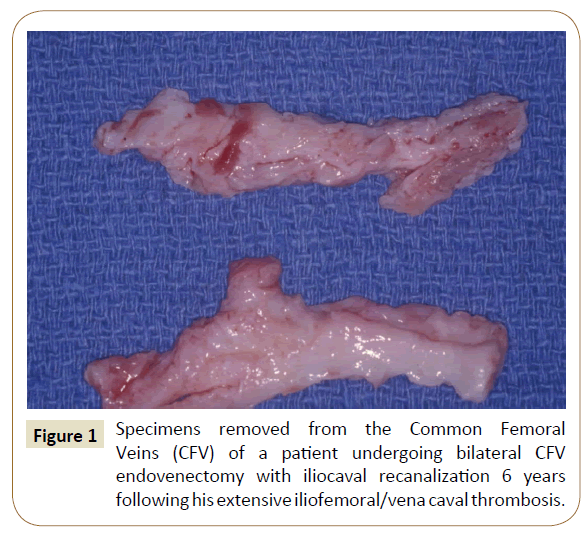
Endophlebecomy of the common femoral vein was performed in 16 patients with post-thrombotic iliofemoral venous obstruction causing incapacitating PTS. Following the endophlebectomy the obstructed iliac veins (and vena cava if necessary) were recanalized with balloon venoplasty and stenting to provide unobstructed venous drainage from the profunda femorous vein to the vena cava [2,3] The tissue excised from the vein was a white fibrous-like tissue with no evidence of thrombus (Figure 1).
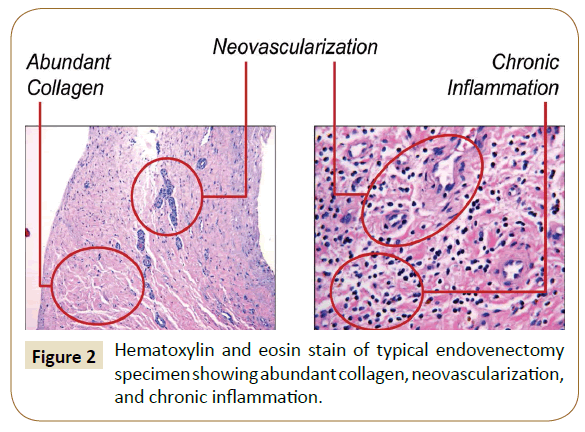
The histologic examination and tissue typing of the specimens excised from the common femoral veins demonstrated that this tissue was collagen, predominately type 1 collagen. On H and E stains, there was seen abundant collagen, neovascularization and chronic inflammation (Figure 2). Observations notably failed to show any thrombus. Biomarker studies showed a high concentration of VEGF-R, especially in younger specimens, less than 1 year since the acute DVT. There was increased vWF in older specimens, greater than 10 years since the acute DVT, consistent with the stability of the older specimens.
The terminology used by physicians to describe tissue is important, as it may have implications for patient care. The term “chronic thrombus” suggests that this tissue might respond to thrombolysis which, of course it will not, since there is no thrombus. This histologic analysis indicates that the term “chronic thrombus” is inaccurate, misleading, and should be abandoned. When intraluminal venous obstruction is described on imaging studies, the term “findings consistent with chronic post-thrombotic venous obstruction” appears appropriate.
References
- Comerota AJ, Oostra C, Fayad Z (2015) A histological and functional description of the tissue causing chronic postthrombotic venous obstruction. Thromb Res 135:882-887.
- Comerota AJ, Grewal NK, Thakur S, Assi Z (2010) Endovenectomy of the common femoral vein and intraoperative iliac vein recanalization for chronic iliofemoral venous occlusion. J Vasc Surg 52:243-247
- Vogel D, Comerota AJ, Al-Jabouri M, Assi ZI (2012) Common femoral endovenectomy with iliocaval endoluminal recanalization improves symptoms and quality of life in patients with postthrombotic iliofemoral obstruction. J Vasc Surg 55:129-135.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences