Transaxillary First Rib Resection and Partial Scalenectomy for Neurogenic Thoracic Outlet Syndrome
Zachary A German, Adam G Strickland and Julie A Freischlag
DOI10.36648/2634-7156.21.6.13
Zachary A German1*, Adam G Strickland2 and Julie A Freischlag2
1Wake Forest School of Medicine, Winston-Salem, USA
2Department of Vascular Surgery, Wake Forest Baptist Medical Center, Winston- Salem, USA
- *Corresponding Author:
- Zachary A German
Wake Forest School of Medicine, Winston- Salem, USA
Tel: +8566492630
E-mail: zgerman@wakehealth.edu
Received Date: February 19, 2021; Accepted Date: March 23, 2021; Published Date: March 30, 2021
Citation: Zachary AG, Adam GS, Julie AF (2021) Transaxillary First Rib Resection and Partial Scalenectomy for Neurogenic Thoracic Outlet Syndrome. J Vasc Endovasc Ther. 6 No. 3: 13.
Abstract
Neurogenic thoracic outlet syndrome typically presents with paresthesia, pain, and impaired strength in the neck, shoulder, and arm, and is typically a diagnosis of exclusion. This condition is caused by compression of the brachial plexus, typically by a bony or soft tissue anomaly present congenitally and influenced by repetitive motion or significant trauma. Treatment typically involves removal of the first rib and anterior scalene to decompress the thoracic outlet and relieve stress to the brachial plexus if the patient has failed conservative treatment with physical therapy and lifestyle modifications. We present a case of neurogenic thoracic outlet syndrome treated surgically via a transaxillary first rib resection.
Introduction
Thoracic outlet syndrome (TOS) is a condition involving the compression of the brachial plexus, subclavian vein, or subclavian artery by bone, muscle, or other soft tissue at the thoracic outlet due to chronic repetitive injury. The estimated incidence of TOS is 8% of the population [1], with over 95% of these cases considered neurogenic [1,2]. This condition is more common in women than men at a rate of 4:11, [3-5], and most commonly affects younger women [6].
Bone and soft tissue abnormalities causing TOS are often congenital or can be caused by chronic repetitive motion and/ or trauma. Congenital abnormalities that can contribute to TOS include anomalies of the transverse process of the seventh cervical vertebra, cervical rib, first rib, enlarged scalene tubercle, scalene muscles, costoclavicular ligaments, subclaviusmuscle, or the pectoralis minor [7-12]. Traumatic bony lesions contributing to TOS include bone remodeling after fractures of the clavicle or first rib and posterior subluxation of the acromioclavicular joint. Soft tissue pathology contributing to TOS include anterior scalene muscle hypertrophy, muscle fiber type adaptive transformation, spasm, and excessive contraction after cervical trauma [1,13-18]. The typical presentation of neurogenic thoracic outlet syndrome includes paresthesia (ulnar nerve distribution), pain, and impaired strength in the neck, shoulder, and arm due to compression of the brachial plexus, with a tender, enlarged scalene on the side of the complaint. Other, less common, signs include occipital headaches, neck discomfort, and tenderness on palpation of the shoulder, mastoid region, or supraclavicular fossa [19].
Diagnosis is made clinically via history and physical exam, and it is often a diagnosis of exclusion [20]. There are three physical exam maneuvers that support the diagnosis of neurogenic TOS: rotation of the neck and tilting of the head to the opposite side eliciting pain in the affected arm, the upper limb tension test (abduction of both arms to 90 degrees with the elbows in a locked position with dorsiflexion of the wrists and head tilted to the side eliciting pain on the contralateral side to the head tilt), and the elevated arm stress test (both arms are raised direction above the head and fists are repeatedly opened and closed) [19]. Frequently, there is a large anterior scalene muscle palpable on the side with symptoms which is tender and much different than the asymptomatic side.
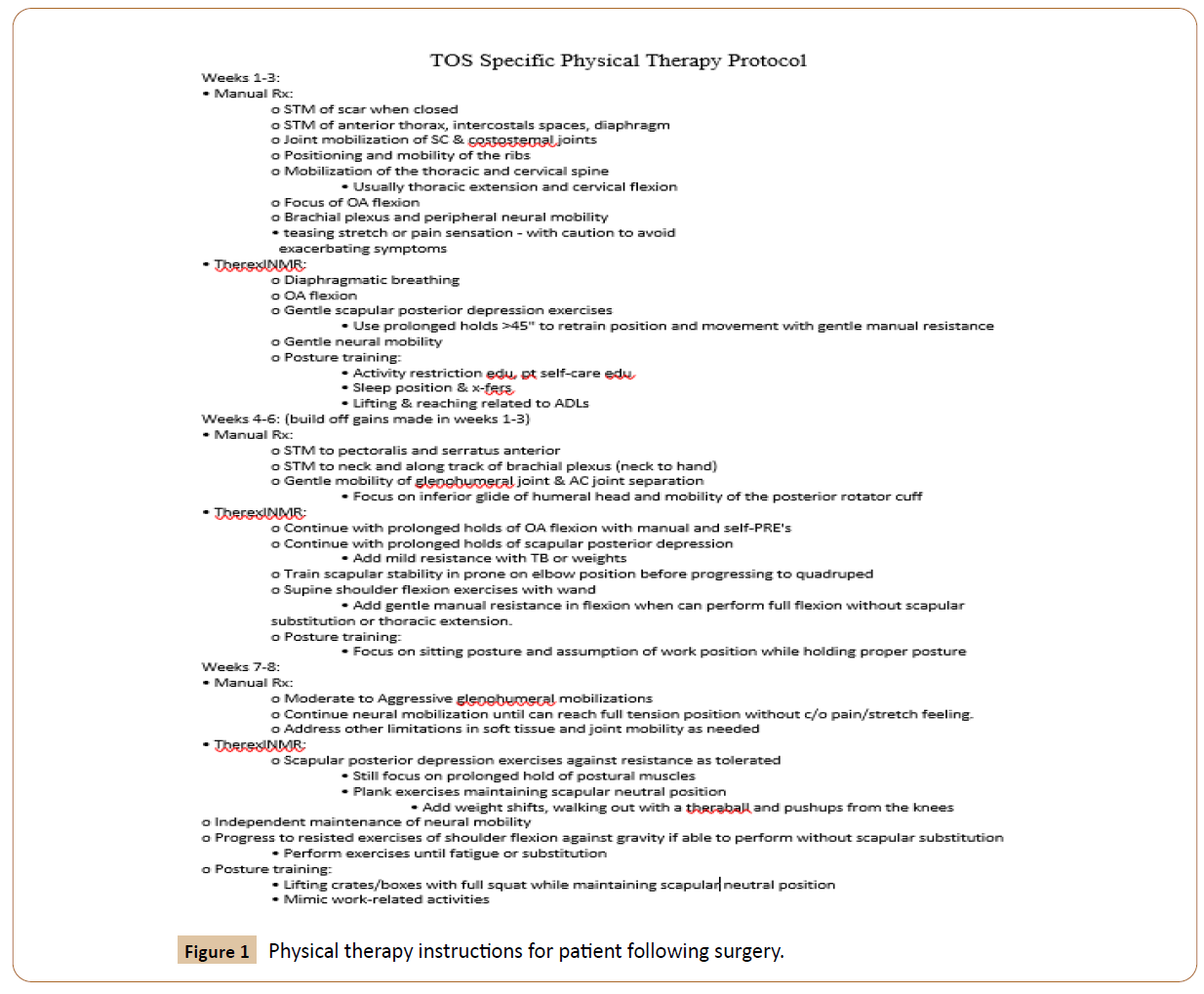
After evaluation, patients should be sent for eight weeks of physical therapy in order to improve range of motion and posture (Figure 1). If symptoms continue after physical therapy, surgical intervention is indicated. Prior to surgery, many patients undergo an anterior scalene block to confirm the diagnosis of neurogenic TOS and to help understand the extent of symptomatic improvement that will be experienced postoperatively. Surgical options include transaxillary approach, supraclavicular scalenectomy with or without first rib resection, combined supraclavicular and infraclavicular approach, and thoracoscopic rib resection. Choice of surgical technique is based on surgeon preference and whether vessel reconstruction is anticipated [19]. All of these surgical techniques are successful at alleviating symptoms.
Case Description
Patient is an 18-year-old female with a one year history of right shoulder injury that occurred during a softball game who presents with pain, numbness, and tingling that has persisted despite eight weeks of physical therapy, as described in Figure 1. Her pain keeps her up at night and has caused her to stop playing softball. On physical exam, she has normal range of motion, large tender right anterior scalene muscle, and normal sized slightly tender left anterior scalene muscle. She has 4/5 strength in the right ulnar distribution, 5/5 strength in the right median and radial nerve distributions, and 5/5 strength in the left ulnar, median, and radial nerve distributions. Elevated arm stress test is positive, with pain on the right side after 15 seconds. Right first rib resection and anterior scalenectomy was indicated, and the patient was consented.
After the induction of general anesthesia, the patient was turned on her left side and her right arm was prepped and draped and then wrapped and padded onto the Machleder retractor. An incision was made just below the axillary hair line between the latissimusdorsi muscle and the pectoralis major muscle and carried down to the chest wall. After dissection through adipose tissue, the first rib, subclavius tendon, subclavian artery and vein, C7 nerve root, and enlarged anterior scalene muscle were identified. A periosteal elevator was used to clean off the right first rib on the inferior border, allowing isolation of the anterior scalene muscle and the subclavius tendon. The patient’s arm was rested and re-elevated to prevent traction of the brachial plexus. The subclavius tendon was cut sharply, then the anterior scalene was cut over a right angle to free up the rib. The rib was cut anteriorly and then posteriorly with the large rib cutter, then the rib was cut several times more medially with rongeurs to clear the vein. The posterior part of the rib was deemed adequate because it was behind the nerve root. Saline was then added to the wound to assess for evidence of pneumothorax, and no bubbles were observed. The saline was suctioned out, the wound was packed to ensure hemostasis, and the wound was closed with 3-0 and 4-0 Vicryl.
While in the operating room, the patient received a pectoralis major block by the anesthesia team for post-op pain control, and was taken to the recovery room in good condition. There were no intra-operative complications, and the patient was taken back to the floor for recovery. Pain was evaluated as 3/10 on the floor with hydromorphone PCA, oxycodone 5 mg q4h PRN, and Tylenol 1000 mg q6h scheduled. On the morning of post-op day one, patient was transitioned to PO pain medications with adequate pain control. She was tolerating diet and ambulating on her own. She was discharged and planned for follow up in one month. Patient was instructed to complete eight weeks of physical therapy. At her scheduled six month post-operation visit, she has had no complaints and has mobility and strength restored.
Discussion
While thoracic outlet syndrome may be relatively common in the general population, the number of people requiring surgical correction for the condition is relatively low. Physical therapy is an excellent preliminary therapy that significantly reduces the amount of patients requiring surgery by as much as 60% [19]. Other reasons for the relatively low number of annual surgeries for thoracic outlet syndrome include difficulty in diagnosing the condition and the low number of surgeons with significant experience in treating the condition. TOS is diagnosed clinically and is often a diagnosis of exclusion [20], requiring many months of testing to rule out other etiologies. Once diagnosed, management can also be very difficult due to the relatively low number of experienced providers as well as the lack of evidence supporting either surgical or conservative management [5].
If surgical treatment of neurogenic thoracic outlet syndrome is chosen, it is predominantly achieved via a transaxillary or supraclavicular approach with removal of the first rib. Both approaches have reported few complications [21-30], and choice of approach is mainly based on the experience of the surgeon. In specialized surgical centers, both approaches achieve excellent outcomes. However, when performed outside specialized centers, surgeons have more sporadic operative experience with these techniques, and complication rates, specifically brachial plexus injuries, are reported to be higher. Patients treated in specialized centers also tended to have lower rates of vascular injuries, shorter hospital lengths of stay, and lower hospital charges [31].
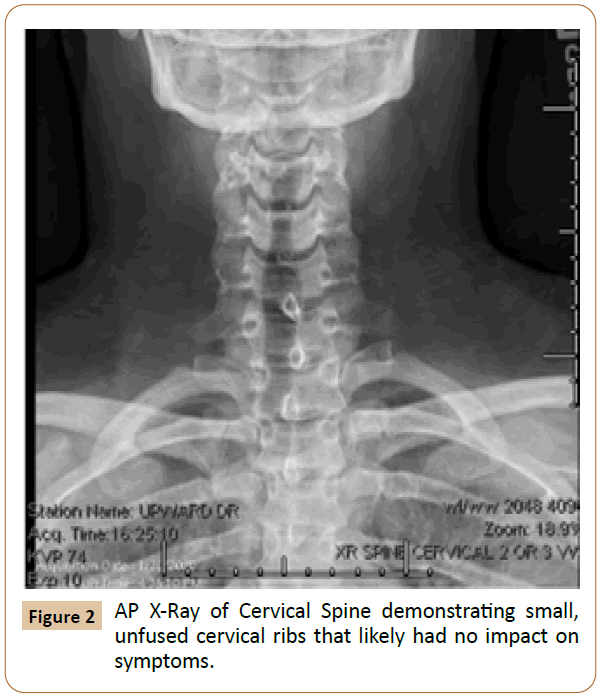
Previous literature has suggested the need to resect both the cervical rib and first rib in patients with clinically significant Gruber class 2, 3, and 4 cervical ribs to prevent the need for a second operation. These classes of cervical ribs are large in size and are frequently fused to the first rib, which can cause arterial compression, aneurysm formation, thrombosis, or embolization [32]. Cervical ribs have an incidence in the general population of 0·2% to 1·0% [33,34], but are generally asymptomatic and do not require resection unless very large and/or fused to the first or second rib [35]. In this patient’s case, the cervical ribs were small and not fused with the first ribs, so were therefore unlikely to impact symptoms. Additionally, plain radiograph of the neck (Figure 2) and MRI of the shoulder before surgery showed no abnormalities.
Surgical intervention for neurogenic thoracic outlet syndrome does not always prove successful. About 10% of patients experience residual, recurrent, or contralateral neurogenic symptoms. Patients who had residual or unresolved symptoms were more likely to be older, active smokers, present with chronic pain syndromes or neck and/or shoulder comorbidities, and have a longer duration of symptoms [36,37]. Patients under 40 years of age with neurogenic thoracic outlet syndrome who underwent transaxillary first rib resection had much better outcomes than those who were older [37,38]. Pre-operatively, these patients had greater narcotic use and had CT-guided Botox injections with less relief of symptoms [36].
Recurrent symptoms usually are due to scar tissue which forms at about a year after surgery. Postoperative physical therapy helps to prevent that recurrence and some patients require three to six months of postoperative physical therapy depending on their preoperative length of symptoms. The recurrent symptoms due to scar tissue can be treated with physical therapy and sometimes botox injections [36,37]. Some patients have recurrent symptoms early after rib resection, which usually is related to a re-injury due to chronic repetitive motion or trauma. Physical therapy usually improves those symptoms [36].
Finally, patients who developed contralateral symptoms were more likely to have originally presented due to repetitive injury rather than trauma. These patients are effectively treated with first rib resection and scalenectomy on the contralateral side. Routinely, one should wait a year between rib resections in order for the patient to completely recover from the first rib resection [36].
In summary, with appropriate patient selection, performance of an excellent surgical intervention, and attention to post-operative physical therapy, patients with neurogenic thoracic outlet can have excellent long term results with excellent quality of life.
References
- Davidovic LB, Kostic DM, Jakovljevic NS, Kuzmanovic IL, Simic TM (2003) Vascular thoracic outlet syndrome. World J Surg 27:545-550.
- Sanders RJ, Hammond SL, Rao NM (2007) Diagnosis of thoracic outlet syndrome. J VascSurg 46: 601-604.
- Gockel M, Vastamäki M, Alaranta H (1994) Long-term results of primary scalenotomy in the treatment of thoracic outlet syndrome. J Hand Surg Br 19:229-233.
- Demondion X, Bacqueville E, Paul C, Duquesnoy B, Hachulla E, et al. (2003) Thoracic outlet: assessment with MR imaging in asymptomatic and symptomatic populations. Radiol 227:461-468.
- Degeorges R, Reynaud C, Becquemin JP (2004) Thoracic outlet syndrome surgery: long-term functional results. Ann VascSurg18:558-565.
- Van HW (2001) MRI of the brachial plexus. EurRadiol 11: 325-336.
- Gruber E (1952)Cervical rib; report of a case. S Afr Med J26:551-552.
- Makhoul RG, Machleder HI (1992) Developmental anomalies at the thoracic outlet: an analysis of 200 consecutive cases. J VascSurg16:534-542.
- Rockwood CA, Groh GI, Wirth MA, Grassi FA (1997) Resection arthroplasty of the sternoclavicular joint. J Bone Joint Surg Am 79:387-393.
- Athanassiadi K, Kalavrouziotis G, Karydakis K, Bellenis I (2001) Treatment of thoracic outlet syndrome: long-term results. World J Surg 25:553-557.
- Jain S, Monbaliu D, Thompson JF (2002) Thoracic outlet syndrome caused by chronic retrosternal dislocation of the clavicle. Successful treatment by transaxillary resection of the first rib. J Bone Joint Surg Br 84:116-118.
- Barkhordarian S (2007) First rib resection in thoracic outlet syndrome. J Hand Surg Am 32:565-570.
- Roos DB (1982)The place for scalenectomy and first-rib resection in thoracic outlet syndrome. Surg 92:1077-1085.
- Machleder HI, Moll F, Verity MA (1986)The anterior scalene muscle in thoracic outlet compression syndrome. Histochemical and morphometric studies. Arch Surg 121:1141-1144.
- Mackinnon SE (1994) Thoracic outlet syndrome. Ann Thorac Surg 58:287-289.
- Schwartzman RJ, Maleki J (1999) Postinjury neuropathic pain syndromes. Med Clin North Am 83:597-626.
- Kai Y, Oyama M, Kurose S, Inadome T, Oketani Y, et al. (2001) Neurogenic thoracic outlet syndrome in whiplash injury. J Spinal Disord 14:487-493.
- Pascarelli EF, Hsu YP (2001) Understanding work-related upper extremity disorders: clinical findings in 485 computer users, musicians, and others. J Occup Rehabil 11:1-21.
- Arnaoutakis GJ, Freischlag JA, Reifsnyder T (2014) Transaxillary Rib Resection for Thoracic Outlet Syndrome. Atlas Vasc Surg Endovasc Ther 14: 193-203.
- Watson LA, Pizzari T, Balster S (2009) Thoracic outlet syndrome part 1: clinical manifestations, differentiation and treatment pathways. Man Ther 14:586-595.
- Green RM, McNamara J, Ouriel K (1991) Long-term follow-up after thoracic outlet decompression: an analysis of factors determining outcome. J Vasc Surg 14:739-745.
- Jamieson WG, Chinnick B (1996) Thoracic outlet syndrome: fact or fancy? A review of 409 consecutive patients who underwent operation. Can J Surg 39:321-326.
- Leffert RD, Perlmutter GS (1999) Thoracic outlet syndrome. Results of 282 transaxillary first rib resections. Clin Orthop Relat Res 368:66-79.
- Axelrod DA, Proctor MC, Geisser ME, Roth RS, Greenfield LJ (2001) Outcomes after surgery for thoracic outlet syndrome. J Vasc Surg 33:1220-1225.
- Hempel GK, Shutze WP, Anderson JF, Bukhari HI (1996) 770 consecutive supraclavicular first rib resections for thoracic outlet syndrome. Ann Vasc Surg 10:456-463.
- Urschel HC, Razzuk MA (1998) Neurovascular compression in the thoracic outlet: changing management over 50 years. Ann Surg 228:609-617.
- Sanders RJ, Haug CE, Pearce WH (1990) Recurrent thoracic outlet syndrome. J Vasc Surg 12:390-398.
- Sanders RJ, Pearce WH (1989)The treatment of thoracic outlet syndrome: a comparison of different operations. J Vasc Surg 10:626-634.
- Altobelli GG, Kudo T, Haas BT, Chandra FA, Moy JL, et al. (2005) Thoracic outlet syndrome: pattern of clinical success after operative decompression. J Vasc Surg 42:122-128.
- Samarasam I, Sadhu D, Agarwal S, Nayak S (2004)Surgical management of thoracic outlet syndrome: a 10-year experience. ANZ J Surg 74:450-454.
- Chang DC, Lidor AO, Matsen SL, Freischlag JA (2007) Reported in-hospital complications following rib resections for neurogenic thoracic outlet syndrome. Ann Vasc Surg 21:564-570.
- Chang KZ, Likes K, Davis K, Demos J, Freischlag JA (2013) The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg 57:771-775.
- Guttentag AR, Salwen JK (1999) Keep your eyes on the ribs: the spectrum of normal variants and diseases that involve the ribs. Radiograph 19:1125-1142.
- Adson AW, Coffey JR (1927)Cervical rib: a method of anterior approach for relief of symptoms by division of the scalenusanticus. Ann Surg 85:839-857.
- Davies AH, Walton J, Stuart E, Morris PJ (1991)Surgical management of the thoracic outlet compression syndrome. Br J Surg 78:1193-1195.
- Rochlin DH, Likes KC, Gilson MM, Christo PJ, Freischlag JA (2012) Management of unresolved, recurrent, and/or contralateral neurogenic symptoms in patients following first rib resection and scalenectomy. J Vasc Surg 56:1061-1067.
- Rochlin DH, Gilson MM, Likes KC, Graf E, Ford N, et al. (2013) Quality of life scores in neurogenic thoracic outlet patients undergoing first rib resection. J Vasc Surg 57:436-443.
- Lum YW, Brooke BS, Likes KC, Modi M, Grunebach H, et al. (2012) Impact of anterior scalene lidocaine blocks on predicting surgical success in older patients with neurogenic thoracic outlet syndrome. J Vasc Surg 55:1370-1375.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences