Abstract
Undescribed Anatomical Predictors of Vascular Injury after Fully-Percutaneous Trans Femoral Trans Catheter Aortic Valve Implantation
Abstract
Background:
Vascular injury (VI) remains frequent after trans catheter aortic valve implantation (TAVI). We aimed to assess the incidence, predictive factors, and the impact of early VI after fully-percutaneous (FP) TAVI.
Method: We included a total of 139 consecutive patients who underwent FP transfemoral TAVI in our institution with 14 to 18Fr sheath systems, through right (119, 85.6%) or left (20, 14.4%) femoral arteries. VI was classified as mayor or minor according to VARC-2 definitions. In hospital data were prospectively collected. Follow-up was available for all patients. Reassessment of femoral artery anatomy as determined by computed tomography was performed including lumen diameters, calcification, tortuosity, height of femoral bifurcation and marked collateral circulation around common femoral artery.
Results: Mean age was 81 ± 6.5, 54% were men, logEuroSCORE were 13.9 ± 7.9 and STS-score was 6.3 ± 4.9. Balloon-expandable and self-expandable devices were used in 14 (10.1%) and 125 patients (89.9%), respectively. Mayor and minor VI were observed in 25 (18%) and in 20 patients (14.3%) respectively, 20 of them due to suboptimal femoral closure (80% of major VI occurring in the first half of the learning curve). Lower platelet count (p=0.043), higher calcification of aortic valve (p=0.049), presence of femoral collaterals (OR=4.5, [95% CI: 1.6-12.9], p=0.005), height of femoral bifurcation (OR=14.5, [95% CI: 5.0-42.1], p<0.001), and failed femoral closure (OR=21.3, [95% CI: 4.5-101.4], p<0.001) were associated to higher rate of VI. The median length of hospitalization was 11.6 days [IQR: 7-14], (15.7 days [IQR: 8-19] in the VI cohort, p<0.001). VI was associated to higher in hospital mortality (13.3 vs. 2.1%, p=0.014).
Conclusion: In patients who underwent FP TAVI, the rate of VI is still high and associated to worse outcomes. A high common femoral artery bifurcation and the presence of collaterals, especially if associated to other concomitant predisposing factors for VI, should be handled with special care and surgical access may be considered.
Author(s):
Javier Tobar, Ignacio J Amat-Santos*, Javier Castrodeza, Irene Martin-Morquecho, Carlos Cortes, Paol Rojas, Hipólito Gutiérrez, Itziar Gomez and Jose A San Román
Abstract | Full-Text | PDF
Share this

Google scholar citation report
Citations : 177
Journal of Vascular and Endovascular Therapy received 177 citations as per google scholar report
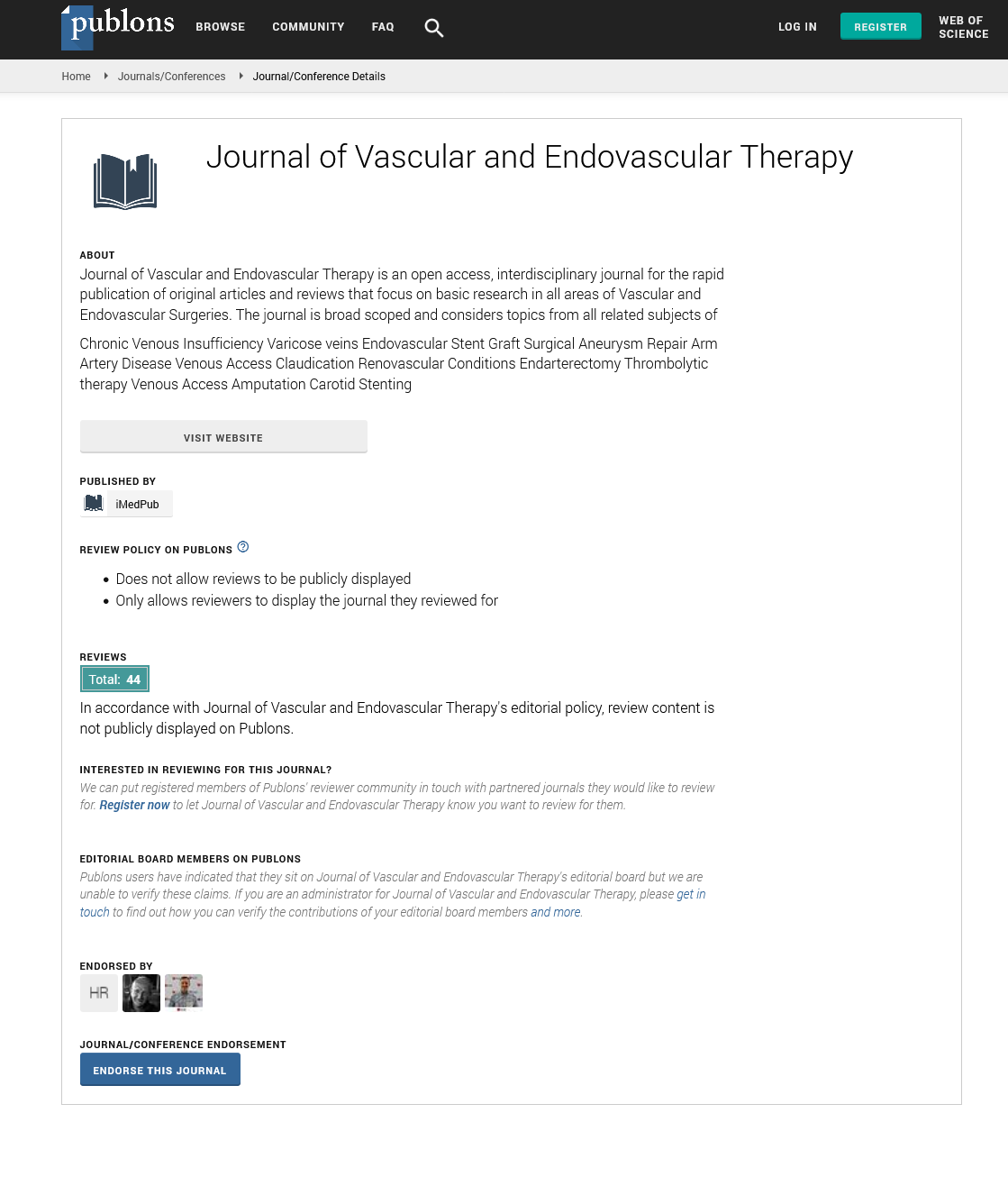
Journal of Vascular and Endovascular Therapy peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Open J Gate
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences