5-Year Outcome for Endoleak Type 2 after Endovascular Treatment in Abdominal Aortic Aneurysm in Songklanagarind Hospital
Chonpisith Chodchoy, Wittawat Tantarattanapong and Dhanakom Premprabha
DOI10.21767/2573-4482.20.05.27
1Department of General Surgery, Songklanagarind hospital, Thailand
2Vascular surgery service, Department of General Surgery, Songklanagarind hospital, Thailand
- *Corresponding Author:
- Chonpisith Chodchoy
Department of general surgery,
Songklanagarind hospital, Thailand
E-mail:chonpisith.c@psu.ac.th
Received Date: November 02, 2020; Accepted Date: November 11, 2020; Published Date: November 18, 2020
Citation: Chonpisith C, Wittawat T, Dhanakom P (2020) 5-Year Outcome for Endoleak Type 2 after Endovascular Treatment in Abdominal Aortic Aneurysm in Songklanagarind Hospital. J Vasc Endovasc Ther. 5 No. 5: 27.
Abstract
Objective: To study the incidence rate of endoleak type 2 in patients with abdominal aortic aneurysm treated with endovascular procedures. The results in Songklanagarind Hospital 5 years ago.
Methods: Retrospective research studies in patients receiving abdominal aortic aneurysm treatment using elective endovascular repair, retrospective studies from Jan 2012- Dec 2016 and have followed up for 2 years to evaluate the incidence of endoleak type II and physical factors such as gender, age, weight, height, body mass index, and any underlying illnesses that are related to the occurrence of leaks.
Results: In the year 2012-2016, there was a collection of data of patients diagnosed with aneurysm that had elective surgery. A total of 250 patients underwent surgery, with an average age was 76 (70,80) years, representing 194 males (77.6%). The average size of aneurysms is 6 centimeters and the incidence of endoleak type II was 73 people (29%). In related factors, Dyspilipidemia is likely to cause a significant endoleak type II (P <0.001). At the same time, it is found that in the first year after surgery, there is a chance of endoleak type II.
Conclusion: From this study, it was found that at the Songklanagarind Hospital, there was an endoleak type II 29% and found that the risk of dyslipidemia is related to the endoleak type II.
Keywords
Endoleak; Endovascular treatment; Abdominal aortic aneurysm
Introduction
Abdominal aortic aneurysm is the expansion of blood vessels more than 50% from normal diameter. The most common position is under the renal artery (Infrarenal aorta type). Currently, the disease is more prevalent in older men and women who smoke [1]. Aneurysm is the 15th leading cause of death in the United States in 2013 during the age of 60-64 years [2]. The mortality rate of patients with ruptured abdominal aortic aneurysm in the population aged over 45 years in the United States between 1999- 2009 is 5.6 per 100,000 population, with differences between males mortality rate is 9 people per 100,000 population and in females mortality rate is 3.2 people per 100,000 population [3]. Factors affecting arterial aneurysms include age, males, white people, a family history of aneurysms, smoking, hypertension, dyslipidemia, peripheral vascular disease, coronary artery disease, COPD [4]. More studies have shown that smoking is a very important factor for arterial artery disease [5]. Treatment of abdominal aortic aneurysm, there are 2 methods of treatment: open abdominal surgery. And methods of intravenous catheter therapy (endovascular), which began in 1986 by Volodos and has developed gradually, respectively [6]. In 2006, more than 60-70% of patients undergoing abdominal aortic aneurysm were treated with EVAR [7]. Type II endoleakage is caused by an area that blood flowing back. (back-bleeding side branches) such as inferior mesenteric artery, lumbar artery, middle sacral artery, which can be detected after surgery by computer tomography and can be found about 10-20% [8,9]. Incidence of endoleak type II is varied 8-45%. Optimal management of endoleak type II is controversial due to conflicting data. Some surgeons believe that endoleak type II have a benign course with spontaneous resolution and low aneurysm rupture rate, thus indicating a more conservative approach [10].
At present, there is no study of complications occurring in Thailand. Songklanagarind Hospital, Songkhla Province is a tertiary hospital, there are a large number of patients suffering from aortic aneurysm each year and tends to increase every year. This study analyzed data of aneurysm patients who came to treatment at Songklanagarind hospital to provide basic information for Songklanagarind Hospital and use information for the development of other patients, with an emphasis on endoleak type 2 as incidence rates, it affects treatment decisions about whether patients should be embolized or wait for the endoleak closed itself.
Method
Study design: Retrospective study.
Study setting: Songklanagarind hospital.
Target population: Patients who have been diagnosed with abdominal aortic aneurysm in Songklanagarind hospital.
Inclusion criteria: Patients diagnosed with abdominal aortic aneurysm in Songklanagarind Hospital according to ICD-10 are I71.4 (Abdominal aortic aneurysm, without ruptured). The patient is treated with endovascular repair during 1 January 2012 - 31 December 2016 and complete monitoring within 2 years.
Exclusion criteria: Patient incomplete information.
Data collection: Requesting permission to collect historical data through the Office of Human Research Ethics and the director of Songklanagarind Hospital. Retrospectively retrospective database of Songklanagarind Hospital through HISview program and isolate patients with ICD-10 diagnosis such as I71.4 (Abdominal aortic aneurysm, without ruptured).Selecting and excluding incomplete details. Collect data in EPIDATA format and analyze data using R software version 3.6.1 for window.
Statistical analysis: Continuous variable data such as age, weight, BMI were reported with mean and standard deviation or median (range). Discrete variables: gender, diameter of aneurysms, location of aneurysms, risk factors such as coronary artery disease, diabetes, kidney disease, COPD, hypertension, dyslipidemia, peripheral vascular disease, smoking. The incidences were reported with hazard ratio, Kaplan-Meier graph. The relationship between endoleakage occurrence and various related factors using Cox.P value was considered significant when it was <.05. Statistical analysis was performed by R software version 3.6.1 for Windows software.
Result
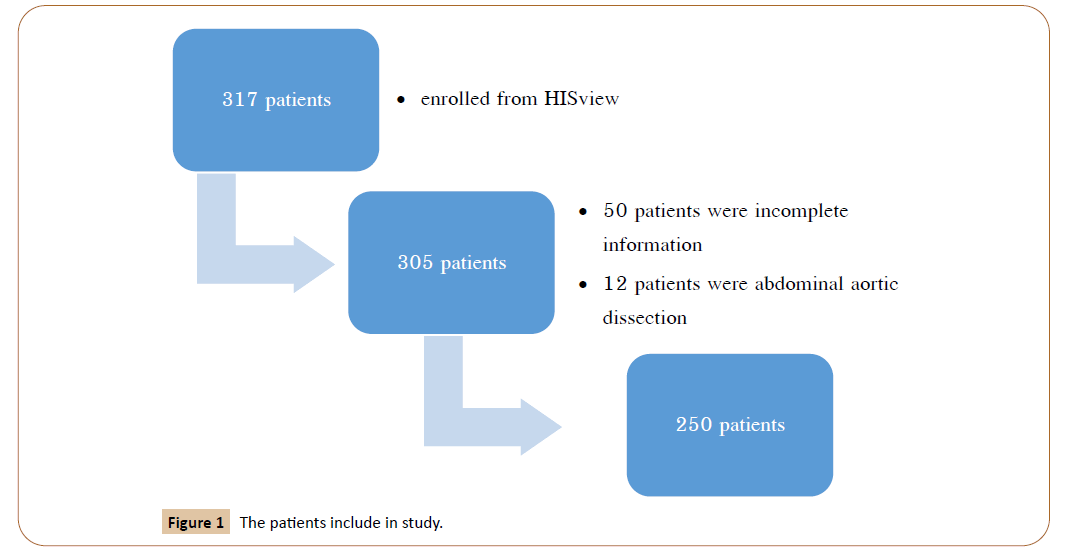
317 patients were enrolled from HISview program according by ICD 10, I71.4 (Abdominal aortic aneurysm, without ruptured). 12 patients were abdominal aortic dissection. 55 patients were incomplete information.Then the patients diagnosed with abdominal aortic aneurysm that had undergone elective surgery was 250 patients (Figure 1). 194 patients were male and 56 were female. A median age was 76 (range 70,80). The median size of aneurysm was 6 (5.4,7). The size of aneurysm <5 cm in 26 patients, 5-5.4 cm in 45 patients, 5.5-6.4 cm in 80 patients and >/= 6.5 cm in 99 patients. The demographics and comorbidities are reported in Table 1.
Table 1 Demographic data.
| All | EL-2 | No EL-2 | P-value | |
|---|---|---|---|---|
| Total | 250 | 73 | 177 | |
| Sex Male Female |
194(77.6) 56(22.4) |
51(69.9) 22(30.1) |
143(80.8) 34(19.2) |
0.086 |
| Age (median) | 76(70,80) | 76(71,80) | 76(69,80) | 0.241 |
| Age group <80 >/=80 |
184(73.6) 66(26.4) |
52(71.2) 21(28.8) |
132(74.6) 45(25.4) |
0.698 |
| Smoking Yes No |
172(68.8) 78(31.2) |
47(64.4) 26(35.6) |
125(70.6) 52(29.4) |
0.413 |
| Alcohol Yes No |
75(30) 175(70) |
20(27.4) 53(72.6) |
55(31.1) 122(68.9) |
0.671 |
| Body weight (kg) Mean(SD) | 56.4(10.9) | 57.5(10.6) | 55.9(11) | 0.28 |
| Body height (cm) Median(IQR) |
161(155.5,167) | 160(155,167.2) | 162(156.5,167) | 0.551 |
| BMI Mean(SD) | 21.6(3.8) | 22.1(3.9) | 21.3(3.7) | 0.134 |
| Duration from diagnosis to treatment | 63 (21.8,168.8) | 61 (32,230.5) | 64 (17,149) | 0.379 |
| Position Suprarenal Juxtarenal Infrarenal |
1 (0.4) 26 (10.4) 223 (89.2) |
0 (0) 7 (9.6) 66 (90.4) |
1 (0.6) 19 (10.7) 157 (88.7) |
1 |
| Size(median, IQR) | 6 (5.4,7) | 6 (5.5,7.1) | 6 (5.3,7) | 0.337 |
| Size(cm) <5 5-5.4 5.5-6.4 >/=6.5 |
26 (10.4) 45 (18) 80 (32) 99 (39.6) |
6 (8.2) 11 (15.1) 23 (31.5) 33 (45.2) |
20 (11.3) 34 (19.2) 57 (32.2) 66 (37.3) |
0.617 |
A total of 250 patients underwent surgery, with an average age was 76 (70,80) years, representing 194 males (77.6%) and 56 females (22.4%). The most position type of aortic aneurysm was infrarenal type 223 patients (89.2%). The median size of aneurysms is 6 centimeters (5.4,7) and the incidence of endoleak type II was 73 people (29%). Average body weight was 56.4kg (SD=10.9). The duration from diagnosis to treatment was 63 days. Patients who smoking that had endoleak type 2 is not significant between smoking or non-smoking (p-value = 0.413) (Table 1).
In related factors, patients with coronary artery disease, the incidence ofendoleak type 2 more than non-cardiovascular disease (24.7% vs 20.3%, p-value = 0.558). Patients with hypertension, the incidence of endoleak type 2 more than non-HT patients (75.3% vs 62.1%, p-value 0.063). Dyslipidemia is likely to cause a significant endoleak type II (P<0.001). At the same time, it is found that in the first year after surgery, there is a chance of endoleak type II (Table 2).
Table 2 Underlying disease related endoleak type II.
| All | EL-2 | No EL-2 | P-value | |
|---|---|---|---|---|
| Underlying disease Yes No |
218(87.2) 32(12.8) |
70(95.9) 3(4.1) |
148(83.6) 29(16.4) |
0.015 |
| Cardiovascular disease Yes No |
54 (21.6) 196 (78.4) |
18 (24.7) 55 (75.3) |
36 (20.3) 141 (79.7) |
0.558 |
| Diabetes mellitus Yes No |
35 (14) 215 (86) |
12 (16.4) 61 (83.6) |
23 (13) 154 (87) |
0.608 |
| Chronic kidney disease Yes No |
43 (17.2) 207 (82.8) |
12 (16.4) 61 (83.6) |
31 (17.5) 146 (82.5) |
0.984 |
| COPD Yes No |
36 (14.4) 214 (85.6) |
11 (15.1) 62 (84.9) |
25 (14.1) 152 (85.9) |
1 |
| Hypertension Yes No |
165 (66) 85 (34) |
55 (75.3) 18 (24.7) |
110 (62.1) 67 (37.9) |
0.063 |
| Dyslipidemia Yes No |
80 (32) 170 (68) |
35 (47.9) 38 (52.1) |
45 (25.4) 132 (74.6) |
<0.001 |
| CVA Yes No |
240 (96) 10 (4) |
73 (100) 0 (0) |
167 (94.4) 10 (5.6) |
0.037 |
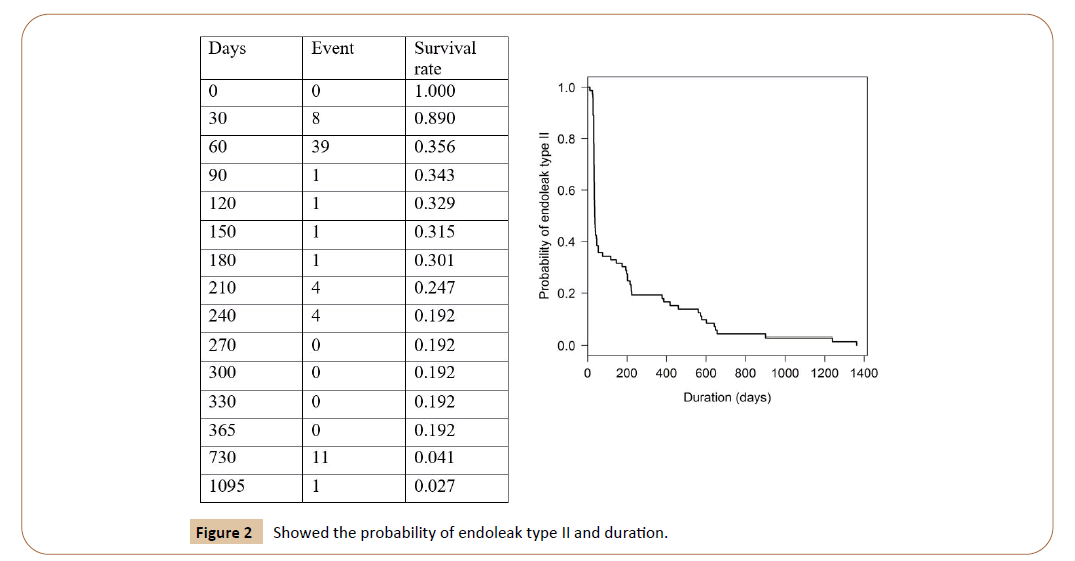
Incidence of endoleak type II was 73 patients (29%).The incidence was high in 6 months after endovascular treatment and tend to decrease continuously as follow. The median date of detection endoleak type II is 38 days after endovascular repair. From the study showed 47 of 73 patient who diagnosed endoleak type II was detected 8 patients within 30 days and 39 patients within 2 months. The 60-day survival for endoleak type II is 89% and tend to decrease.
In 73 patients of endoleak type II, 7 patients (9.5%) needed for embolization due to larger aneurysm sac after follow up, 10 patients (13.6%) resolved of endoleak type II after conservative treatment, 2 patients had done angiogram due to larger aneurysm sac and showed endoleak type I and extended EVAR was performed and the remaining patient had stable disease during follow up for 2 years (Figure 2).
Discussion
The incidence of endoleak type 2 cite in the literature varies between 8 to 45% [11]. It can cause by the variation of diagnosis method (ultrasound and CTA) and observer interpretation. Nevertheless, in Songklanagarind hospital, the incidence of endoleak type II after endovascular treatment was 29%, was accepted variance. It’s had difference due toraceand terrain. Current data are conflicting, and it has not been determined between conservative management or intervention had better outcome.
From literature review, conservative treatment of endoleak type 2 is based on the relatively high percentage of endoleak type II that resolve spontaneously 58% in 12 months [12]. Endoleak type 2 had no increase risk for aneurysm rupture. In this study we found only 10 of 73 patients (13.6%) that had spontaneously resolve but, 54 of 73 patients (74%) had stable endoleak type II after follow up for 2 years. The difference in percentage of spontaneous resolved cause may be due to not following up longtime enough.
Our finding in this study also support that endoleak type 2 are largely benign post-operation complications which require close surveillance, but not aggressive intervention. There are 11.7- 44.7% that needed for the intervention in literature review [13-16], only 9 patients (12.3%) needs intervention due to larger sac after follow up. No mortality case due to endoleak type II.
Conclusion
Overall, we found the incidence of endoleak type II after endovascular repair in Songklanagarind hospital is 29%. There are 13.6% that had spontaneously resolve and 74% had stable aneurysm sac after follow up for 2 year and only 12.3% that needed intervention treatment.
References
- Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, et al. (1991) Subcommittee on reporting standards for arterial aneurysm, ad hoc committee on reporting standards, society for vascular surgery and North American chapter, international society for cardiovascular surgery: suggested standard for reporting on arterial aneurysm. J Vasc Surg 13: 452-458.
- www.cdc.gov/nchs/data/dvs/lcwk1_2013.pdf
- Bown MJ, Sutton AJ, Bell PR, Sayers RD (2002) A meta-analysis of 50 years of ruptured abdominal aortic aneurysm. Br J Surg 89: 714-730.
- Alcorn HG, Wolfson Jr SK, Sutton-Tyrrell K, Kuller LH, O'Leary D (1996) Risk factors for abdominal aortic aneurysm in older adults enrolled in the cardiovascular Health Study. ArteriosclerThromb Vasc Biol 16: 963-970.
- Lederle FA, Johnson GR, Wilson SE, Chute EP, Littooy FN, et al. (1997) Prevalence and associations of abdominal aortic aneurysm detected through screening. Aneurysm Detection and Management (ADAM) Veterans Affairs Cooperative Study Group. Ann Internal Med 126: 441-449.
- Volodos NL, Shekhanin VE, Karpovich IP, Troian VI, Gur'ev I (1986) A self-fixing synthetic blood vessel endoprosthesis. Vestn Khir IM II Grek 137: 123-125.
- De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, et al. (2010) Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. N Engl J Med 362: 1881-1889.
- Chuter TA, Faruqi RM, Sawhney R, Reilly LM, Kerlan RB, et al. (2001) Endoleak after endovascular repair of abdominal aortic aneurysm. J Vasc Surg 34: 98-105.
- Baum RA, Carpenter JP, Golden MA, Velazquez OC, Clark TW, et al. (2002) Treatment of type 2 endoleak after endovascular repair of abdominal aortic aneurysm: comparison of transarterial and translumbar technique. J Vasc Surg 35: 23-29.
- Ricotta JJ (2010) Endoleak management and postoperative surveillance following endovascular repair of thoracic aortic aneurysms. J Vasc Surg 52: 91S-99S.
- Silverberg D, Baril DT, Ellozy SH, Carroccio A, Greyrose SE, et al. (2006) An 8-year experience with type II endoleaks: natural history suggests selective intervention is a safe approach. J Vasc Surg 44: 453-459.
- Gelfand DV, White GH, Wilson SE (2006) Clinical significance of type II endoleak after endovascular repair of abdominal aortic aneurysm. Ann Vasc Surg 20: 69-74.
- Jones JE, Atkins MD, Brewster DC, Chung TK, Kwolek CJ, et al. (2007) Persistent type 2 endoleak after endovascular repair of abdominal aortic aneurysm is associated with adverse late outcomes. J Vasc Surg 46: 1-8.
- El Batti S, Cochennec F, Roudot-Thoraval F, Becquemin JP (2013) Type II endoleaks after endovascular repair of abdominal aortic aneurysm are not always a benign condition. J Vasc Surg 57: 1291-1297.
- Fabre D, Fadel E, Brenot P, Hamdi S, Caro AG, et al. (2015) Type II endoleak prevention with coil embolization during endovascular aneurysm repair in high-risk patients. J Vasc Surg 62: 1-7.
- Sarac TP, Gibbons C, Vargas L, Liu J, Srivastava S, et al. (2012) Long-term follow- up of type II endoleak embolization reveals the need for close surveillance. J Vasc Surg 55: 33-40.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences