Bend but Don't Break? A Case of Supera Stent Fracture in the Popliteal Artery
Valle JA, Famouri A and Rogers RK
DOI10.21767/2573-4482.100039
Valle JA, Famouri A and Rogers RK*
University of Colorado, Aurora, CO, USA
- *Corresponding Author:
- R Kevin Rogers
Program Director/Vascular Medicine and Intervention, Interventional Cardiology
University of Colorado, Mail Stop B132, Leprino Building
12401 East 17th Avenue, Room 560, Aurora
CO 80045, USA.
Tel: 720848-6506
Fax: 720848-7315
E-mail: kevin.rogers@ucdenver.edu
Received date: February 07, 2017; Accepted date: February 15, 2017; Published date: February 21, 2017
Citation: Valle JA, Famouri A, Rogers RK. Bend but Don’t Break? A Case of Supera Stent Fracture in the Popliteal Artery. J Vasc Endovasc Surg. 2017, 2:1. doi: 10.21767/2573-4482.100039
Abstract
Peripheral intervention to the femoropopliteal segment has been associated with increased rates of stent fracture. The Supera peripheral stent has been designed to withstand the torsional and compressive forces in the femoropopliteal vascular bed, with observational data supporting its use in these segments. While this data has been promising, it remains limited. Hereby, we present the first report of a Supera peripheral stent fracture, and highlight the importance of ongoing evaluation and longer term follow-up for such technological advances to ensure safety and efficacy in populations.
Keywords
Peripheral vascular intervention; Peripheral vascular disease; Stent fracture
Introduction
Peripheral arterial stent fracture is a known complication of peripheral intervention and is associated with increased risk of in-stent restenosis and re-occlusion of the target vessel [1,2]. While reported rates of stent fracture have varied widely overall [1], stent location has been implicated as a risk factor for fracture. Stent deployment in one such location, the femoropopliteal segment, has been associated with elevated rates of stent fracture [2]. The Supera peripheral stent (Abbott Vascular, Tamecula) has a novel, interwoven nitinol platform that was designed to have longitudinal and axial flexibility to specifically withstand the torsional and compressive forces encountered in the femoropopliteal anatomy. With 1,100 reported implantations across 7 registries, there have been no reported fractures at 1 year follow-up [3]. Thus, the Supera remains the only peripheral stent indicated for popliteal arterial lesions, due to its ability to withstand the torsion behind the knee. However, the data supporting its use is observational alone, with the majority only completing 1 year of follow-up [3]. In this case, we describe the first report of a Supera peripheral stent fracture.
Case Report
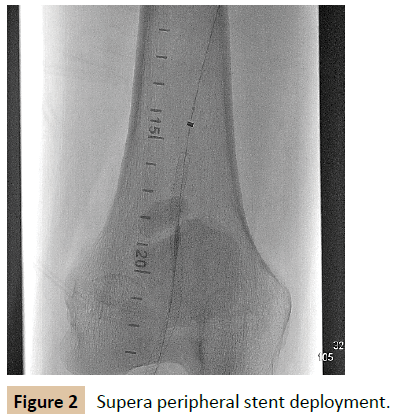
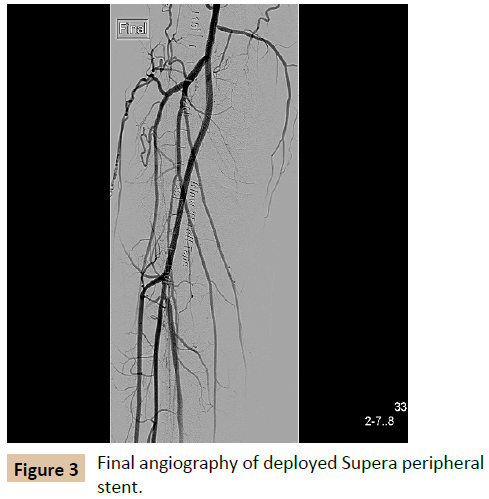
The patient is a 59 year-old male with lifestyle-limiting right calf claudication and ischemic rest pain (Rutherford category 3-4), who initially presented for evaluation after non-invasive studies had suggested the presence of a right popliteal occlusion. He underwent a complex intervention involving antegrade and retrograde attempts at recanalization, complicated by dissection preventing further attempts. A Vascular Surgery consultation was requested, but it was thought the patient did not have adequate conduits to support a surgical intervention for symptom relief. Following 3 months of ongoing medical optimization and a walking program, the patient returned for a peripheral angiography, and a repeat attempt at recanalization of the popliteal occlusion. After retrograde crossing of the lesion, orbital atherectomy was performed followed by pre-dilation with a 4.0 x 100 mm angioplasty balloon at high pressure (Figure 1). A 4.0 × 100 mm Supera self-expanding stent was then deployed across the popliteal lesion with particular care to avoid excessive elongation (Figure 2). Final angiography demonstrated a patent, well expanded stent in the right popliteal artery, and intact tibioperoneal vessels distally, without any evidence of dissection, distal embolization, or perforation (Figure 3).
Three months later, the patient returned to Peripheral Vascular Clinic with recurrence of ischemic symptoms involving his right calf and foot. His symptoms had initially been improved for approximately 2 months immediately after popliteal stenting. Over the following month, the patient had had worsening right lower extremity symptoms, with foot and calf discomfort on any kind of ambulation. Non-invasive studies with duplex ultrasonography demonstrated significant velocity increases across the distal superficial femoral artery and proximal popliteal artery, suggestive of high grade stenosis within the proximal stent.
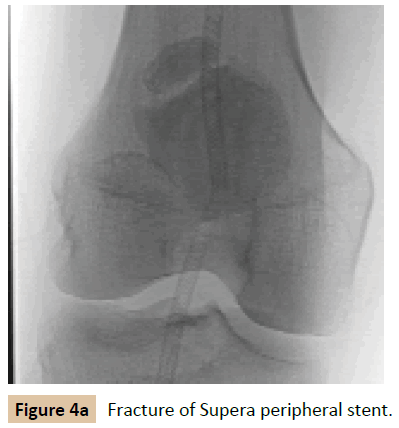
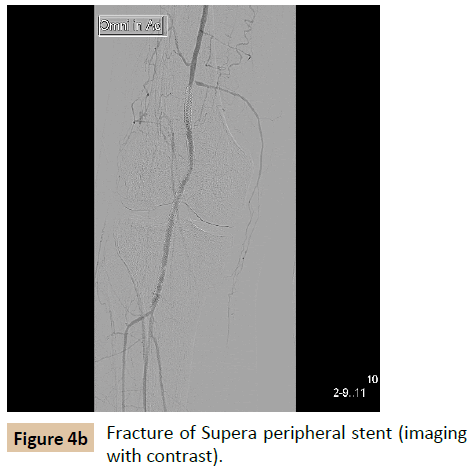
The patient underwent a repeat diagnostic angiography, which demonstrated fracture of the previously placed Supera stent, with complete non-union of stent struts in the mid stent (Figures 4a and 4b), and a long segment of severe (80%) in-stent restenosis proximal and distal to the fracture. Subsequent angioplasty was performed across the stent fracture with a scoring balloon. Given the prior fracture, the decision was made to avoid repeat stenting.
Discussion
This case represents the first report of a Supera stent fracture in the literature. While the unique design of Supera may decrease the incidence of stent fracture, there are no randomized trials comparing Supera to traditional stents to support this claim. Moreover, the registry data has been limited in long-term followup. Technological advances like the Supera are needed to optimize outcomes for the endovascular treatment of femoropopliteal disease, but further investigation and longer term follow-up are needed to fully evaluate these novel designs and their efficacy.
Conclusion
The Supera stent platform is a promising modality for the endovascular treatment of femoropopliteal peripheral vascular disease; however further investigation and longer-term followup are needed to ensure efficacy.
References
- Rits J, van Herwaarden JA, Jahrome AK, Krievins D, Moll FL (2008) The incidence of arterial stent fractures with exclusion of coronary, aortic, and non-arterial settings. Eur J Vasc Endovasc Surg 36: 339-345.
- Scheinert D, Scheinert S, Sax J, Piorkowski C, Braunlich S, et al. (2005) Prevalence and clinical impact of stent fractures after femoropopliteal stenting. J Am Coll Cardiol 45: 312-315.
- Bishu K, Armstrong EJ (2015) Supera self-expanding stents for endovascular treatment of femoropopliteal disease: a review of the clinical evidence. Vascular Health and Risk Management 11: 387-395.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences