Burden of Aortic Dissection in Minorities: The Way Forward
Oloyede EO, Crawford RS, Harris DG, Sarkar R and Johnson WR
DOI10.21767/2573-4482.100012
Oloyede EO1*, Crawford RS2, Harris DG3, Sarkar R2 and Johnson WR1
1University of Maryland School of Medicine, Division of Cardiology, Hypertension Section, Baltimore, Maryland, USA
2Center for Aortic Disease, Department of Surgery, University of Maryland School of Medicine and University of Maryland Medical Center, Baltimore, Maryland, USA
3Department of Surgery University of Maryland Medical Center, Baltimore, Maryland, USA
- *Corresponding Author:
- Ebenezer Oloyede
University of Maryland School of Medicine, Division of Cardiology, Hypertension Section, Baltimore, Maryland, USA
Tel: 4438138767
E-mail: o.oluwasegun@gmail.com
Received date: March 29, 2016; Accepted date: May 17, 2016; Published date: May 23, 2016
Citation: Ebenezer Oloyede, et al. Burden of Aortic Dissection in Minorities: The Way Forward. Journal of Vascular & Endo Surgery. 2016, 1:2. doi: 10.21767/2573-4482.100012
Abstract
Aortic dissection (AD) is a catastrophic but potentially preventable medical emergency. Delay in diagnosis and treatment of AD contributes to its high morbidity and mortality, especially in this population. We conducted a review of articles that describe the risk factors, gaps in management, and outcomes of AD in U.S. minority populations. Very few data exist on prospective, population-based AD, especially in underserved minority populations. AD confers significant burden on both the patient and the health system. From the economic and public health standpoint, disparities in access to health disproportionately affect minorities and can give rise to needless costs. Most of the risk factors for AD in minorities are modifiable and addressing them in a timely manner using a bidirectional approach ("Upstream" and "Downstream") could be cost-effective in reducing the burden of AD. Community health Workers (CHWs) have been shown to be effective in coordinating care for other emergency medical conditions in minorities but not for AD. We propose the integration of the CHWs and patientcentered medical home (PCMH) models into the care coordination effort for preventive and follow-up care of AD patients. Our main objective is to draw the attention of clinicians, researchers and policy makers to the current challenges of AD in minorities and sensitize them to our proposed evidence-based patient-centered, multidisciplinary community-based framework for addressing the burden of AD, in addition to conducting more prospective, population-based AD research in underserved minority populations.
Keywords
Aortic dissection; Burden; Hypertension; Prevention; Minorities and health disparities; Community health workers; Patient-centered medical home
Introduction
Aortic dissection (AD) is a catastrophic but potentially preventable medical emergency. Only a few population-based studies on incidence, presentation, management and outcomes exist in minorities, despite evidence suggesting the incidence of AD is increasing alongside the growing and aging U.S population [1]. The reason for the upward trend is likely multifactorial.
The burden of AD on patients and the health care system is cause for great concern. More incident cases are being identified due to greater utilization of cross-sectional imaging studies, advancements in imaging techniques, and the growing population [2]. Within that growth, United States census data indicates minorities now constitute 37% of the U.S. population and are projected to comprise up to 57% in 2060. Evidence also suggests that the incidence of AD (particularly Type B) may be higher in Blacks compared to Whites (52.4% vs 39.3%) [3,4]. The need for early recognition of the impact of AD on America’s work forces, economy and health system is paramount. Delay in diagnosis and treatment contributes to the high morbidity and mortality of AD. Hypertension, cigarette smoking, and cocaine use are the most common risk factors associated with AD among U.S minorities [5], although other less common risk factors like genetic mutations and connective tissue disorders have also been identified.
In the United States, the prevalence of cardiovascular disease and hypertension is highest among minorities (especially Hispanics and Blacks) [6,7]. Additionally, more advanced disease and poor prognosis are more common among minorities, including poor hypertension control rates [8]. Patients with AD require intensive follow-up for blood pressure control, monitoring for signs and symptoms of end organ ischemia, and surveillance for aneurysmal degeneration of the dissected aorto-iliac segments. It follows that better hypertension and risk factor management will play an instrumental role in the secondary prevention of AD and its associated morbidity and mortality.
Community Health Workers working within the context of a patient-centered medical home (PCMH) are a very useful health care resource and can serve as an effective adjunct to the care coordination effort for reducing the burden of Aortic Dissection. Unfortunately, not many studies have explored the use of community health workers in the prevention and follow-up care of AD patients. In the United States, evidence indicates that CHWs can contribute to reducing cardiovascular disease (CVD) burden by participating in the efforts to reduce cardiovascular risk factors and in the management of hypertension, particularly among hard-to-reach subpopulations [9].
It is imperative to emphasize that this article acknowledges the well-documented predictors of AD in all patients and does not discriminate in favor of any race-based patient profile. The differences noted here and the suggested ways forward are solely meant to sensitize clinicians to the fact that this is a significant problem in minorities. This will also help clinicians interested in targeting their cardiovascular preventive efforts toward populations experiencing health disparities. In this review, we seek to draw attention to the burden of AD among minorities and propose the CHWs and patient-centered medical home (PCMH) models, which have worked in the past in other pathologies, for mitigating its trends.
The main objective of this review is to draw the attention of clinicians, researchers and policy makers to the current challenges of AD in minorities and sensitize them to our proposed evidence-based patient-centered, multidisciplinary community-based approach for addressing the burden of AD, in addition to conducting more prospective, population-based AD research in underserved populations.
Methods
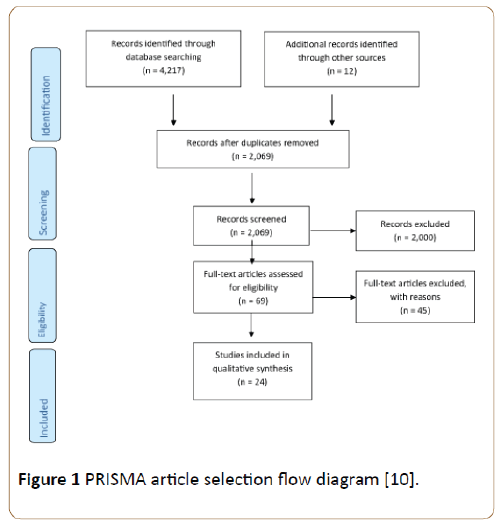
A systematic literature review of English language articles on aortic dissection epidemiology and outcomes among underserved minority populations was performed using PRISMA methodology10. Embase and PubMed were searched for “aortic dissection” AND (“community health worker” or “patient centered medical home”) AND (“minority” or “blacks” or “hispanics”) [10]. Articles that described epidemiology, outcomes, or disparities therein of aortic dissection in minorities were included for analysis. Additionally, citations from relevant articles were reviewed to identify manuscripts that may have been missed in the literature search. Finally, a search of government guidelines including from the Agency for Healthcare and Research Quality, Centers for Medicare and Medicaid Services (CMS), and the U.S. Preventive Services Task Force (USPSTF) on prevention and post-discharge follow-up care in minorities was performed. We then performed an evidence-based, patient-centered, bi-directional framework using a community-integrated, multi-disciplinary care coordination approach for AD prevention and follow-up care in “hard-to-reach” patient populations [11,12]. This is a review article and did not require patient informed consent, enrollment of human subjects, use of protected health information, and Institutional Review Board approval.
Results
After systematic database review, collection of articles, and removal of duplicate citations, 2,069 articles were screened for inclusion (Figure 1). Of these, 69 were relevant to our some or all of our selection criteria. 45 articles were excluded because they mainly focused on the pathophysiology and diagnosis of AD. In total, 24 articles were included for synthetic review, including 6 government guidelines. Of the primary articles, one study was a population-based prospective study while the remainders were retrospective studies. There is currently a paucity of data on prospective population-based, subpopulation incidence and outcomes of AD [8]. The true incidence of AD is difficult to determine because many incorrectly diagnosed cases sometimes escape notice.
Figure 1: PRISMA article selection flow diagram [10].
Furthermore, hospital-based registries often underestimate the incidence and case fatality for AD and its associated risk factors, especially for cases that did not make it to the Hospital, which further reiterates at the burden of AD may be greater than what the hospital records suggest. Additionally, race-specific patient outcomes data for AD is limited. Available studies, however, suggest that minorities are disproportionately affected by co-morbidities, barriers to access to care, and disease-specific morbidity and mortality [13]. The causes for such race-based disparities in the management and outcomes of aortic disease are unclear, and there are currently no strategies to address this situation [14]. One possible reason may be the disproportionately high prevalence of uncontrolled or malignant hypertension, a major risk factor for AD in minorities compared to their white counterparts [15]. For example, in an observational study involving 1,354 Black and White patients with AD enrolled in 13 U.S. centers participating in the International Registry of Acute Aortic Dissection (IRAD), 90% of the 189 Black study population had hypertension compared to 74% of the 1,165 Whites enrolled in the study [4]. The high prevalence of hypertension and lack of adequate control in minorities, especially treatment-resistant hypertension, may be a major factor responsible for the poor outcomes of hypertension related AD in this population. Although AD often occurs in a sudden, episodic malignant way that may not have been preventable by a tight B.P control, we believe that some case of hypertension-related AD can be prevented in high risk patients. A recent, first ever, prospective population-based epidemiological AD study by the Oxford Vascular Group in the U.K confirms previous observations about the strong association of hypertension with AD, and advocates for improvement in primary prevention of AD incidence and its associated case fatality through aggressive management of hypertension, which is more prevalent in minorities [16,17].
Discussion
Current challenges
Over the years, health disparities have been shown to be one of the significant structural flaws of the U.S. healthcare system [16]. A study in the 2003–2006 period by the Joint Center for Political and Economic Studies estimated that eliminating health disparities for minorities would save $229 billion in direct medical expenditures, and reduce indirect costs associated with illness and premature death by approximately $1 trillion [17]. Unfortunately, only a few of the existing disparities in accessing care seem to be improving [18].
More specific to AD, there is currently no established consensus strategy for screening high-risk patients. Although the U.S. Preventive Services Task Force (USPSTF) has recommended a one-time screening for abdominal aortic aneurysm (AAA) with ultrasonography in men ages 65 to 75 years who have ever smoked [19], there is currently no consensus screening protocol for AD [20]. There is also controversy over the sensitivity and specificity of screening tests, as well as their clinical validity [21]. For example, Creactive protein has been used in screening for both peripheral vascular diseases (PVD) and AD. Although sensitive, it lacks the desired specificity for AD [22-24]. Similarly, electro- and echocardiography lack sufficient accuracy [25,26].
At this time there is no test or combination of tests that can reliably predict development of AD. Therefore, we have to rely on screening for high risk patients for hypertension, smoking, family history of AD and symptoms associated with AD. Population screening for aortic disease can also be improved, first by general recognition and increased awareness by the medical community of familial patterns of aortic disease, and then by novel (genetic) mass screening techniques, especially in first-degree relatives [27,28]. Apart from the challenges associated with screening for AD, current diagnostic modalities, including imaging, biomarkers and genetic studies are expensive, time-consuming, or not widely available. The current approach when diagnosing AD relies heavily on various imaging techniques, including computed tomography and the initial aortic syndrome presentation, although certain patients manage to never make it to the Hospital even under such conditions. Magnetic resonance imaging is also currently being explored and protocols refined. High level of suspicion as well as early imaging is very important, especially in those presenting with both typical (e.g. back or abdominal pain) and atypical symptoms [4]. However, technical and logistical challenges limit the use of imaging tools as screening modalities in various circumstances [29]. Although there is no single accurate biomarker for AD, a number are still under investigation, and a panel of biomarkers may improve the diagnostic yield of this approach [30,31].
Implications
Aortic dissection entails significant implications for the patient. The sudden change from being healthy to being diagnosed with AD is irreversible and comes as a surprise to many patients, with its attendant spectrum of psychosocial and cost consequences.
More dramatically, the early mortality rate for AD approaches 1% per hour over the first 48 hours, making early diagnosis and treatment crucial to improving morbidity and mortality [31]. Poorly controlled chronic hypertension predisposes patients to hypertension-related penetrating aortic endothelial ulcers and intramural hematomas, culminating in AD in high risk patients. Highlights form the results of the AD study by the Oxford Vascular Study Group showed that 67.3% of the hypertensive study population (n=52) had poor pre-morbid B.P control despite being on some form of anti-hypertensive medication(s). Five years before the incident of AD, the percentage of B.Ps recorded at the participating primary care facilities in individual patients were noticed to be greater than 140/90 mm Hg. It is therefore recommended that rigorous control of hypertension and other associated risk factors are crucial in preventing and curtailing the progression of AD and its long-term complications in high risk patients [14].
The chances of survival for AD patients with no access to care are very slim, either in the short or long run. As stated above, the only established recommended treatment for patients with ascending AD, which is most common in Blacks [4], is immediate surgical repair, with mortality ranging from 8-16% [32]. In all cases, control of hypertension in the immediate post-operative period and close follow-up long term for those treated conservatively is of utmost importance and has a heavy impact in the resultant index of mortality [33]. Survival rate for aortic disease has been shown to be directly related to prompt diagnosis and precise management [34]. From the economic standpoint, disparities in quality and access to health care can give rise to needless direct and indirect costs. Details about the cost-effectiveness of surgical aortic dissection repair are outside the scope of this article but, suffice it to say that the cost of surgery, ICU stay, follow-up Hospital visits and CT scans could be staggering. A strategy of early recognition and appropriate control of risk factors for aortic dissection, such as uncontrolled hypertension with or without additional risk factors such as smoking and family history, would certainly provide a more cost-effective approach [31].
The community health workers model
In addressing the problem of hypertension as the most important risk factor for AD, there is a need to identify and effectively treat high-risk patients: i.e. patients with uncontrolled hypertension and other risk factors such as smoking, atherosclerosis, and genetic factors or positive family history of AD. Additionally, it is crucial for AD patients to remain compliant with their recommended treatment regimen to reduce the likelihood of recurrence and disease progression. An effective way of accomplishing this could be by employing the services of Community Health Workers (CHWs).
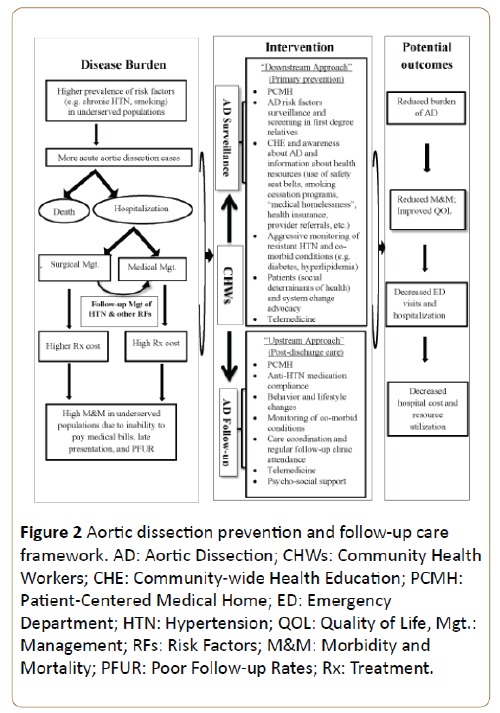
Given that most of the risk factors for AD in minorities are modifiable, addressing them in a timely manner using a bidirectional approach (“Upstream” and “Downstream”) as illustrated in Figure 2 could be a cost-effective way of decreasing the incidence and cost implications associated with AD. This strategy is in line with the 2012 U.S. Patient Protection and Affordable Care Act which advocates for the use of preventive measures to reduce disease burdens as one of its core tenets [33]. In order to mitigate the morbidity and mortality of AD among minorities, effective primary prevention, and more importantly, secondary prevention strategies are the suggested way forward. We therefore propose the integration of the community health care workers (CHWs) model into the care coordination effort for AD prevention and management.
Figure 2: Aortic dissection prevention and follow-up care framework. AD: Aortic Dissection; CHWs: Community Health Workers; CHE: Community-wide Health Education; PCMH: Patient-Centered Medical Home; ED: Emergency Department; HTN: Hypertension; QOL: Quality of Life, Mgt.: Management; RFs: Risk Factors; M&M: Morbidity and Mortality; PFUR: Poor Follow-up Rates; Rx: Treatment.
Community health workers (CHWs) or Care Coordinators are lay members of the community who work collaboratively with the local health care system and usually share the culture, ethnicity, language, socioeconomic status, and life experiences with the community they serve [34]. Studies have shown that most patients can finish their medical story within 90 seconds, but the average physician interrupts them within 18 seconds, due in part to time restrictions of busy clinical practice [35]. CHWs understand the health needs of their community and are able to spend more time providing culturally oriented health education, counseling, and other services such as screening and assisting patients in obtaining the access to care they need. CHWs can also be strategic in providing care coordination and linkage between the Hospital, the community and the primary care clinic [36].
A retrospective comparison study was conducted at University of Maryland between 1991 and 1994 assessing the impact of the CHWs model on healthcare utilization by African- American Medicaid patients with diabetes with or without hypertension. The study, performed on 117 patients, showed a decline in ED admissions by 40%, Hospitalization by 33%; an average savings of $2,245 per patient per year and a total savings of $262, 080, in addition to improved quality of life [35]. Table 1 provides a comparison overview of healthcare utilization before and after CHWs outreach intervention.
| Comparisons of healthcare utilization, one year before and after initial contact | |||||||
|---|---|---|---|---|---|---|---|
| One Year Before | One Year After | Within Group Change | |||||
| Healthcare Utilization Group | Mean | SD | Mean | SD | Mean | SE | Percent |
| ER visits (all) | 1.49 | 2.2 | 0.93 | 1.8 | -0.56 | 0.2 | -38 |
| ER admissions | 0.64 | 1.4 | 0.32 | 1.3 | -0.32 | 0.1 | -53 |
| Total Hospital admissions | 0.95 | 1.5 | 0.66 | 1.4 | -0.29 | 0.2 | -30 |
| Length of hospital stay | 6.35 | 11.8 | 6.69 | 26.2 | 0.34 | 2.6 | 5 |
| Medicaid reimbursements (M $) | 8266 | 15 | 6020 | 18 | -2,246 | 1792 | -27 |
Table 1: The effectiveness of CHWS outreach program (adapted from Fedder do et al.) [35].
Other more recent studies have also shown the important roles that CHWs play in preventive and post-discharge followup services for minority patients with chronic diseases [12,37,38]. One of the main challenges for AD patients after diagnosis is regular follow-up care to ensure adequate blood pressure control.
Despite the high morbidity and mortality of AD, many minorities are lost to follow-up and fall out of care post discharge due to ineffective care coordination and linkage between surgical and medical teams. Currently, CHWs are under-utilized in the screening and follow-up efforts for minority patients with AD. The implication of such a program could produce a substantial impact in the minority population.
Most patients with hypertension and other concomitant risk factors for cardiovascular disease should be placed on appropriate antihypertensive medications, with aggressive attention to concurrent risk factors [37]. CHWs can assist with improving compliance with these medications and instituting other management recommendations, including diet, exercise and smoking cessation. Employing the “Upstream” approach (follow-up care) of this CHWs model (Figure 2) should result in an improvement in post-discharge follow-up clinic attendance rates and consequent mitigation of the previously described risk factors over time, including hypertension, smoking, and medication non-compliance [38,39].
Inclusion of CHWs as members of the patient-provider team enhances the quality of care received by patients, especially those from low resource settings. Evidence-based recommendations for CHWs to intervene in both community based cardiovascular research and patient-provider team efforts demonstrate their importance in helping to eliminate disparities in CVD. CHWs’ role in cardiovascular research has mainly focused on hypertension due to its high prevalence and because it constitutes a significant risk factor for CVD, including AD [40].
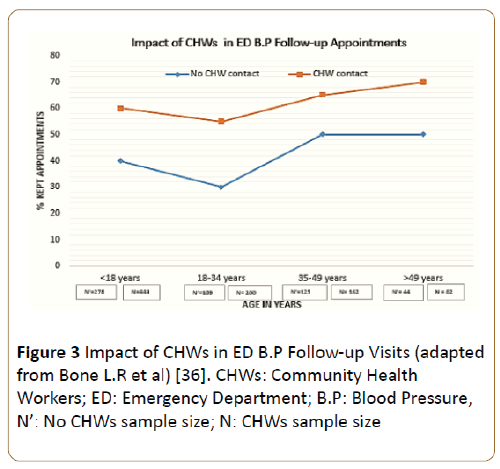
The services of CHWs have previously been successfully been employed in the emergency management of cardiovascular diseases. A 2-year demonstration study in which trained CHWs were introduced into the emergency department (ED) to support the efforts of providers in managing BP among high-risk black men showed a 19% improvement in appointment keeping and a 7% improvement in follow-up visit rates (Figure 3) [12,37].
Figure 3: Impact of CHWs in ED B.P Follow-up Visits (adapted from Bone L.R et al) [36]. CHWs: Community Health Workers; ED: Emergency Department; B.P: Blood Pressure, N’: No CHWs sample size; N: CHWs sample size
The data further supports the notion that CHWs are important in the screening efforts of high-risk patients with CVD as well as in helping to establish linkage to care, assure care coordination, enhance continuity of care and foster ED community integration for CVD follow-up care. Given the long patient follow-up clinic appointments that characterize a busy physician schedule, and the fact that some patients find long distance commuting between theirs home and the clinic challenging, CHWs can assist with providing community-wide health education to patients on the safety role the use of car seat belt plays in preventing trauma-related AD, in addition to educating hypertensive patients with a family history of AD on how to measure and keep a record of home ambulatory B.P, with instructions on next steps regarding persistently elevated home B.P readings [12,41].
Patients with a history of stable chronic AD require regular close monitoring post-discharge and subsequently on an annual basis. The period immediately after the initial diagnosis can be quite challenging, with multiple visits required for fine tuning of newly instituted medication regimens. It is not uncommon that the index dissection admission coincides with the first discovery of a malignant hypertension diagnosis. Patients can be admitted to the Hospital and be discharged on 3-4 new medications. What follows, can be a period of fluctuation, where B.P can either remain high, or become quite low outside of the stressful Hospital environment and the presence of numerous new anti-hypertensive agents. CHWs could be very valuable at a time where B.P monitoring is imperative and a patient’s experience with the new diagnosiss is poor [38,40,41]. It can ensure compliance, provide a mechanism for safe adjustment of doses, and save thousands of dollars in emergency room admissions. In addition, depending on the presence of aneurysmal degeneration of the aorta, there is need for regular evaluation of the aortic diameter at one, three, six month and yearly intervals [38]. In other disease states, this has been accomplished through telephone contacts, home visits, supporting behavior and lifestyle modification efforts, all designed to ensure compliance with physician recommendations [42].
The Centers for Medicare and Medicaid Services, Office of Minority Health (CMS OMH) emphasizes that minority patients with cardiovascular disease need special help in preventing readmissions and recently published a guide for preventing readmissions among racially and ethnically diverse Medicare beneficiaries [43]. Minority patients are less likely than their white counterparts to follow up with a primary care provider or an appropriate specialist after hospital discharge [44]. This is due in part to the fact that racial and ethnic minorities tend to have a lower rate of linkage to a source of continued care post discharge, which leads to a lower quality care [45]. To optimize the quality of care received, minority patients with AD, especially those at high risk for readmission, require early discharge and follow-up plans, counseling about the importance of early and regular follow-up [46], as well as a coordinated referral system using the CHWs model, to assure their navigation to a new primary care provider post-discharge [46,47].
Apart from employing the services of CHWs in the suggested “Upstream” approach (secondary prevention), we also propose a “Downstream” approach (primary prevention) in which CHWs can be incorporated into an AD risk factors screening and follow-up initiative in patients with a positive family history of AD [48]. A high clinical index of suspicion is necessary for identifying and screening patients with risk factors for AD [31,36] (Figure 2). In collaboration with primary care providers and relevant clinical subspecialties, CHWs can assist with identifying and then screening high risk minority patients from the community [48]. For example, patients with a positive family history of AD, chronic smokers, and patients with poor hypertension control, with or without other comorbidities need close monitoring. CHWs can also help provide public health education and awareness about AD, in addition to providing information about available resources like health insurance and other support services, as well as assist with the development of patient-centered and culturally-appropriate AD secondary prevention and postdischarge follow-up care protocol.
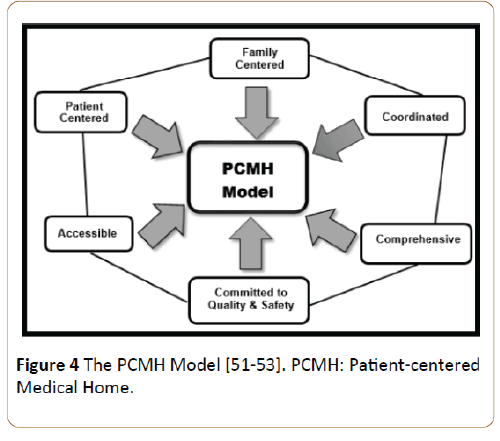
Ideally, CHWs residing in a community near where the patient lives can provide these services, the CHWs model can also be implemented within the framework of a Medical Neighborhood known as Patient-centered Medical Home (PCMH) [49,50] which is an innovative multidisciplinary team based approach to providing care and for transforming the organization and delivery of primary health care [51]. It functions as the core of medical neighborhood and is essentially a medical practice team working closely with patients and providing well-coordinated care [52]. PCMH has the following six important functional components, applicable to the post-discharge management of AD: comprehensive care and access to personal physician, physician-directed medical practice, patient-centeredness, coordinated care, accessible services, quality and safety [53]. The primary goal of PCMH is to enhance open communication with patients and increase health literacy. PCMH also aims at improving communication and coordination between health care providers and institutions, i.e. a high-functioning medical neighborhood that promotes information flow among clinicians and patients, which is very important in caring for AD patients [51,52]. Given that its locus is squarely within the primary care settings of the health system and the fact that many patients require a substantial amount of AD specialty care, the PCMH can play a significant role in creating and promoting a dynamic and functional medical neighborhood ideal for AD post-discharge care [53]. While the patient is the reference point in the medical neighborhood, PCMH is placed at its center (Figure 4), given its role as the intersection point between the patient and the primary coordinator of the patient’s care across various neighbors. Within the PCMH, the primary clinician caring for an AD patient may be a physician or nurse practitioner, assisted by CHWs. It is important to note that the “neighborhood” is not necessarily a geographic entity; rather, it is a set of care-focused multidisciplinary relationships involving the patient and his or her PCMH [53].
There is a great deal of research showing the effectiveness of PCMH through measurable outcomes. One of the primary outcomes is lower per person healthcare costs and better outcomes [54,55] while an AD specialist-oriented healthcare system is related to higher costs and limited improvement in surgical outcome [14,56]. Specifically, studies have shown that using the PCHM model can lead to better blood pressure control and reduced health disparities, decreased emergency room and hospital visits, improved preventive care, reduction in all-cause mortality and morbidity caused by cardiovascular diseases, and increased patient satisfaction [54-56].
Using this two-prong approach, we are optimistic that the burden of AD in minorities would decrease over time. In addition, we hope to improve the quality of life of those with an existing AD diagnosis. This strategy can also lead to a decrease in the frequency of ED visits, Hospital readmission rates, and costs incurred on the health system. Notably, the success of any CHWs model depends on a functional health system. “CHWs programs are neither the panacea for weak health systems nor a cheap option to provide access to health care for underserved populations [48]”.
Limitations
This paper faces some limitations. The scope of the article did not allow discussions about many of the similarities in the etiology, presentation, or outcomes in the management strategies of patients with AD that are effective and guideline based, irrespective of race. Consequently, and given that very few ethnic and racial-based studies on AD have been done, conclusions about the effectiveness of various strategies on AD outcomes among different racial populations should be made with discretion. The scope of this article did not also include some of the challenges associated with the use of CHWs, including failed CHWs programs based on unrealistic expectations, institutionalizing and mainstreaming community participation, poor planning and an underestimation of the effort and input required to make them work. Some of the quality enhancement prospects of PCMH have not been well documented and the implementation of PCMH models of care for primary care service delivery may sometimes lead to increased health care costs. Also, the specific role CHWs should play in the management of treatment-resistant hypertension was not clearly defined. Despite good preventive measures in place, it may still be difficult to accurately predict and prevent the incidence of some cases of AD, given its malignant, episodic pattern of occurrence. Finally, both the level of evidence and the Methodological Index for Non- Randomized (MINOR) Studies for retrospective studies validation were not assessed by the systematic review. Also, given that a significant number of the articles reviewed were from retrospective studies describing different primary and secondary endpoints, meta-analysis was not practical. These analyses could have further reduced the level of bias and enhanced the quality of the articles selected.
Conclusion
Morbidity and mortality associated with AD is very high. Early intervention of AD can prevent complications or death. Well-coordinated, quality outpatient care can potentially prevent the need for AD-related readmission. Hypertension and other risk factor associated with the onset and progression of AD are present in all patients regardless of race but, the prevalence of these risk factors is greatest among minorities. More prospective, population-based AD studies are required to help determine the true incidence of AD in minorities and clinical trials of B.P-lowering drugs should incorporate AD as one of the composite end points for determining the overall treatment impact. More proactive and better multi-disciplinary care coordination is important for ensuring optimal blood pressure control and addressing other AD risk factors in this population. The CHWs model operating within the PCMH environment is recommended as an effective approach for addressing the burden of AD in minorities.
Acknowledgement
The authors acknowledge the contribution of Dr. Jude Ediae to the initial draft of this article.
References
- Clouse WD, Hallett JW, Schaff HV, Spittell PC, Rowland CM, et al. (2004) Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc 79: 176-180.
- Golledge J, Eagle KA (2008) Acute aortic dissection. Lancet 372: 55-66.
- Mukherjee D, Eagle KA (2005) Aortic dissection-an update. Curr Probl Cardiol 30: 287-325.
- Bossone E, Pyeritz RE, O'Gara P, Harris KM, Braverman AC, et al. (2013) Acute aortic dissection in blacks: insights from the International Registry of Acute Aortic Dissection. Am J Med 126: 909-915.
- Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, et al. (2013) Oxford Vascular Study Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation 127: 2031-2037.
- Baruth M, Wilcox S, Egan BM, Dowda M, Laken M, et al. (2011) Cardiovascular disease risk factor clustering among African American adults. Ethn Dis 21: 129-134.
- National Health and Nutrition Examination Survey (2012) Hypertension Among Adults in the United States.
- Vogel TR, Cantor JC, Dombrovskiy VY, Haser PB, Graham AM (2008) AAA repair: sociodemographic disparities in management and outcomes. Vasc Endovascular Surg 42: 555-560.
- Perry HB, Zulliger R, Rogers MM (2014) Community health workers in low, middle, and high-income countries: an overview of their history, recent evolution, and current effectiveness. Annu Rev Public Health 35: 399-421.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA Statement For Reporting Systematic Reviews And Meta-Analyses Of Studies That Evaluate Health Care Interventions: Explanation And Elaboration. Ann Intern Med 151:65.
- Community-based model boosts BP control in high-risk population (2003) Dis Manag Advis 9: 126-128.
- Morrissey NJ, Giacovelli J, Egorova N, Gelijns A, Moskowitz A, et al. (2007) Disparities in the treatment and outcomes of vascular disease in Hispanic patients. J Vasc Surg 46: 971-978.
- Community Health Worker National Work force Study.
- Howard DP, Sideso E, Handa A, Rothwell PM (2014) Incidence, risk factors, outcome and projected future burden of acute aortic dissection. Ann Cardiothorac Surg 3: 278-284.
- Fuchs FD (2011) Why do black Americans have higher prevalence of hypertension: an enigma still unsolved. Hypertension 57: 379-380.
- National Health Disparities Report (2003).
- Joint Center for Political and Economic studies (2009) Annual Report.
- National Health Care Disparities Report (2011).
- Abdominal Aortic Aneurysm: Screening.
- Wen D, Zhou XL, Li JJ, Hui RT (2011) Biomarkers in aortic dissection. Clin Chim Acta 412: 688-695.
- Morello F, Piler P, Novak M, Kruzliak P (2014) Biomarkers for diagnosis and prognostic stratification of aortic dissection: challenges and perspectives. Biomark Med 8: 931-941.
- Ranasinghe AM, Bonser RS (2010) Biomarkers in acute aortic dissection and other aortic syndromes. J Am Coll Cardiol 56: 1535-1541.
- Listijono DR, Pepper JR (2012) Current imaging techniques and potential biomarkers in the diagnosis of acute aortic dissection. JRSM Short Rep 3: 76.
- Cecconi M, Chirillo F, Costantini C, Iacobone G, Lopez E, et al. (2012) The role of transthoracic echocardiography in the diagnosis and management of acute type A aortic syndrome. Am Heart J 163: 112-118.
- John A (2010) Elefteriades, Emily A. Farkas. Thoracic Aortic Aneurysm Clinically Pertinent Controversies and Uncertainties. Journal of the American College of Cardiology 55.
- Juang D, Braverman AC, Eagle K (2008) Cardiology patient pages. Aortic dissection. Circulation 118: e507-510.
- Peng W, Peng Z, Chai X, Zhu Q, Yang G, et al. (2015) Potential biomarkers for early diagnosis of acute aortic dissection. Heart Lung 44: 205-208.
- Sheikh AS, Ali K, Mazhar S (2013) Acute aortic syndrome. Circulation 128: 1122-1127.
- Braverman AC (2010) Acute aortic dissection: clinician update. Circulation 122: 184-188.
- Patel AY, Eagle KA, Vaishnava P (2014) Acute type B aortic dissection: insights from the International Registry of Acute Aortic Dissection. Ann Cardiothorac Surg 3: 368-374.
- https://www.hhs.gov/healthcare/rights/law/.
- Belzer EJ (1999) Improving patient communication in no time. Fam Pract Manag 6: 23-28.
- Fedder DO, Chang RJ, Curry S, Nichols G (2003) The effectiveness of a community health worker outreach program on healthcare utilization of west Baltimore City Medicaid patients with diabetes, with or without hypertension. Ethn Dis 13: 22-27.
- Bone LR, Mamon J, Levine DM, Walrath JM, Nanda J, et al. (1989) Emergency department detection and follow-up of high blood pressure: use and effectiveness of community health workers. Am J Emerg Med 7: 16-20.
- Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, et al. (2010) ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. Catheter CardiovascInterv 76: e43-e86.
- Kangovi S, Mitra N, Grande D, White ML, McCollum S, et al. (2014) Patient-centered community health worker intervention to improve posthospital outcomes: a randomized clinical trial. JAMA Intern Med 174: 535-543.
- Brownstein JN, Bone LR, Dennison CR, Hill MN, Kim MT, et al. (2005) Community health workers as interventionists in the prevention and control of heart disease and stroke. Am J Prev Med 29: 128-133.
- Adair R, Christianson J, Wholey DR, White K, Town R, et al. (2012) Care guides: employing nonclinical laypersons to help primary care teams manage chronic disease. J Ambul Care Manage 35: 27-37.
- Cooper LA, Roter DL, Bone LR, Larson SM, Miller ER, et al. (2009) A randomized controlled trial of interventions to enhance patient-physician partnership, patient adherence and high blood pressure control among ethnic minorities and poor persons: study protocol NCT00123045. Implement Sci 19: 4-7.
- Ferdinand KC, Patterson KP, Taylor C, Fergus IV, Nasser SA, et al. (2012) Community-based approaches to prevention and management of hypertension and cardiovascular disease. J ClinHypertens (Greenwich) 14: 336-343.
- https://www.cms.gov/Newsroom/MediaReleaseDatabase/Press-releases/2016-Press-releases-items/2016-01-26.html.
- DeLia D, Tong J, Gaboda D, Casalino LP (2014) Post-Discharge Follow-Up Visits and Hospital Utilization by Medicare Patients 2007–2010. Medicare & Medicaid research review 4.
- Phillips KA, Mayer ML, Aday LA (2000) Barriers to care among racial/ethnic groups under managed care. Health Aff 19: 65-75.
- Hansen LO, Young RS, Hinami K, Leung A, Williams MV (2011) Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med 155: 520-528.
- Saitz R, Larson MJ, Horton NJ, Winter M, Samet JH (2004) Linkage with primary medical care in a prospective cohort of adults with addictions in inpatient detoxification: room for improvement. Health Serv Res 39: 587-606.
- Community health workers: What do we know about them.
- Findley S, Matos S, Hicks A, Chang J, Reich D (2014) Community health worker integration into the health care team accomplishes the triple aim in a patient-centered medical home: a Bronx tale. J Ambul Care Manage 37: 82-91.
- Strategic Goal : Strengthen Health Care.
- https://pcmh.ahrq.gov/page/defining-pcmh.
- Janamian T, Jackson CL, Glasson N, Nicholson C (2014) A systematic review of the challenges to implementation of the patient-centred medical home: lessons for Australia. Med J Aust 201: S69-73.
- The Patient-Centered Medical Home (PCMH).
- Greenfield S, Nelson EC, Zubkoff M, Manning W, Rogers W, et al. (1992) Variations in resource utilization among medical specialties and systems of care. Results from the outcomes study 267: 1624-1630.
- Phillips RL, Starfield B (2004) Why does a U.S. primary care physician workforce crisis matter. Am Fam Physician 70: 440-446.
- Forrest CB, Starfield B (1996) The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. J FamPract 43: 40-48.
- Baileit M, Hughes C, Beesla R (2010) The patient-centered medical home: A purchaser guide. Patient Centered Primary Care Collaborative 03-35.
- Macinko J, Starfield B, Shi L (2003) The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998. Health Serv Res 38: 831-865.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences