Double Aortic Arch with TOF: Single Stage Single Incision Approach
Soumya Guha, Jai Bhagwan, Anubhav Gupta, Vijay Grover and Vijay Gupta
DOI10.21767/2573-4482.18.03.13
Soumya Guha*, Jai Bhagwan, Anubhav Gupta, Vijay Grover and Vijay Gupta
Department of Cardiothoracic and Vascular Surgery, PGIMER and Dr. RML Hospital, New Delhi, India
- *Corresponding Author:
- Dr. Soumya Guha
Department of Cardiothoracic and Vascular Surgery
PGIMER and Dr. RML Hospital
New Delhi-110001, India
Tel: 919999790836
E-mail: surya_blue@yahoo.co.uk
Received Date: July 26, 2018; Accepted Date: August 23, 2018; Published Date: August 30, 2018
Citation: Guha S, Bhagwan J, Gupta A, Grover V, Gupta V (2018) Double Aortic Arch with TOF: Single Stage Single Incision Approach. J Vasc Endovasc Therapy. 3:13.
Abstract
Introduction: Double Aortic Arch (DAA) is a rare accompaniment of Tetralogy of Fallot (TOF). Traditionally DAA surgery is accomplished through a posterolateral thoracotomy, which may be combined with a median sternotomy for total correction of TOF either in the same setting or as a staged procedure. In this case report we present the more economical single stage approach via median sternotomy.
Background: Double aortic arch is the most common complete vascular ring and comprises 1% of operable congenital cardiac disease. The most common cyanotic congenital heart lesions associated with DAA are TOF and transposition of great arteries. Literature on the approach to DAA with TOF is confusing as some propound a staged approach via postero-lateral thoracotomy and subsequent sternotomy, some a single stage approach using both median sternotomy and postero-lateral thoracotomy, while we agree with Zhou Dan et al. in approaching via median sternotomy as a single stage approach to correct both DAA and TOF.
Case: A 3-year-old presented with a diagnoses of DAA with TOF, confirmed by relevant imaging. Median sternotomy was used and the non-dominant left arch distal to left subclavian artery was divided before intracardiac repair for TOF.
Conclusion: The difficulty in handling the non-dominant arch from the midline accounts for the prevalence of the two incision approach wherein the arch is tackled by a separate posterolateral thoracotomy. This case report describes successful management of TOF with DAA via median sternotomy, where we used an interesting technique to successfully clamp and divide the difficult to access non-dominant arch.
Keywords
Double aortic arch; Tetralogy of fallot; Unique approach; Single stage single incision approach; Median sternotomy
Introduction
Double aortic arch (DAA) is a rare accompaniment of Tetralogy of Fallot (TOF). Division of the non-dominant arch is traditionally accomplished through a posterolateral thoracotomy, which may be combined with a median sternotomy for total correction of TOF either in the same setting (single stage 2 incisions) or as a staged procedure (2 stages 2 incisions). An alternative approach would be to divide the non-dominant aortic arch via the median sternotomy itself, when it is present with Tetralogy of Fallot (single stage single incision). This case report describes the more economical successful management of TOF with DAA via median sternotomy as a single stage approach, in a 3-year-old child.
Case Report
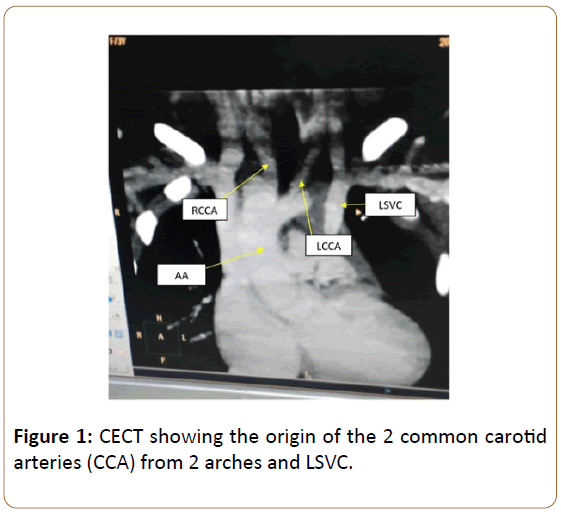
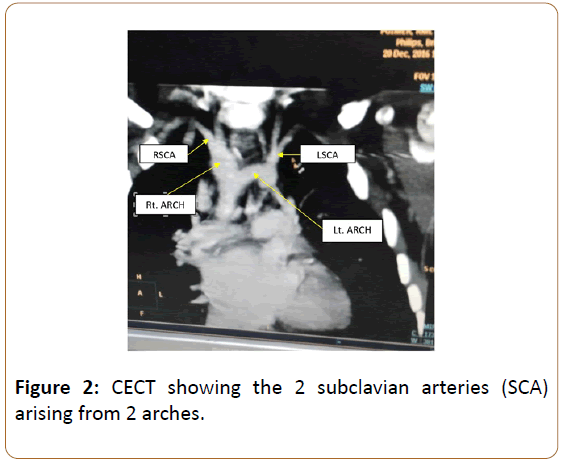
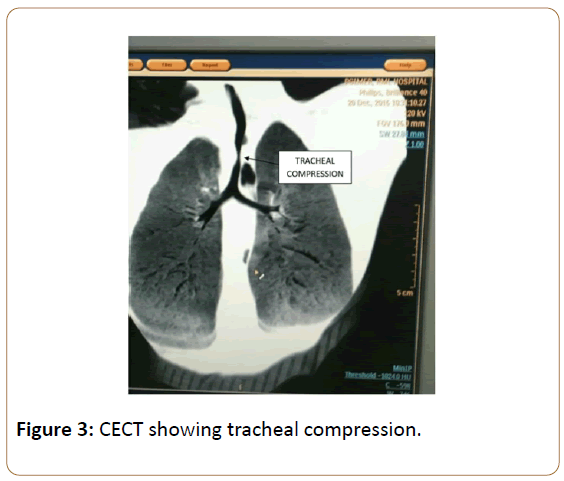
A 3-year-old female child presented with tachypnea and central cyanosis. She had previously undergone posterior sagittal anorectoplasty with colostomy for anorectal malformation. She had a non-functioning left kidney with normal renal function tests. Her chest radiograph was consistent with TOF and revealed dual indentations over trachea. Echocardiography and cardiac catheterisation confirmed the diagnoses of TOF with double aortic arch and bilateral superior vena cavae. CT Angiography revealed left common carotid and subclavian arteries arising from a non-dominant left sided arch without atresia. Right common carotid and subclavian arteries originated from the dominant right arch continuing as right sided descending thoracic aorta (Figures 1,2). Oesophageal and tracheal compression were present (Figure 3).
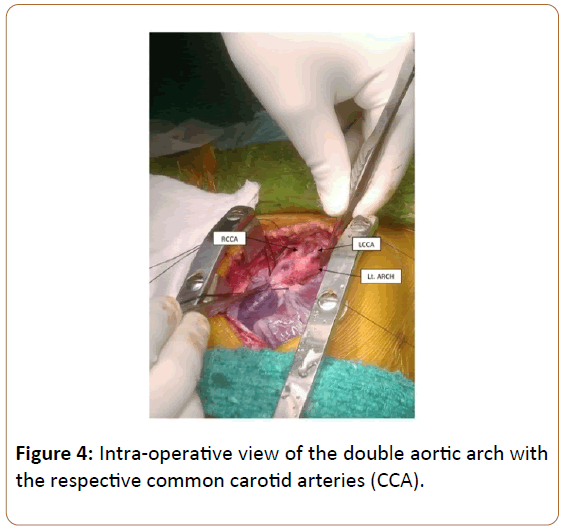
The patient was taken up for Intra-cardiac repair with division of left arch. Intra-arterial pressure monitoring lines were placed in the left radial and femoral arteries. After standard median sternotomy both arches were identified by origin of common carotid arteries (Figure 4). Proximal left arch and left subclavian artery were looped and ductus was divided. Left arch distal to subclavian artery was test clamped with no significant radio-femoral pressure variation. Cardiopulmonary bypass was instituted with aorto-bicaval cannulation. The arch distal to left subclavian artery needed to be divided between two arterial clamps.
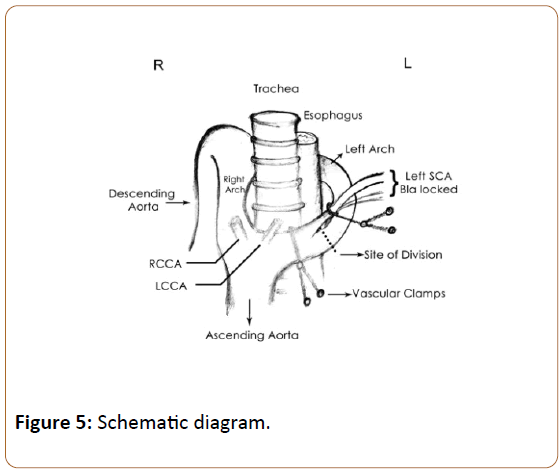
The length of distal arch accessible from this approach would have been short and would have left a very short stump after division for over sewing. To circumvent this problem the proximal vascular clamp was shifted proximal to the subclavian origin after doubly snaring the subclavian artery with a vessel loop to prevent back bleed (blalocking of left subclavian artery). The distal vascular clamp placed on the non-dominant arch distal to left subclavian artery, as distally as possible. The arch distal to left subclavian artery was divided (Figure 5). The divided ends were oversewn in double layer with continuous prolene sutures. Following division of the left arch the underlying trachea and oesophagus were exposed and a ring of fibrous tissue around them was divided. The Left SVC was then cannulated and the Intra-cardiac repair for TOF was done in standard fashion. Post-operative recovery was uneventful. After 4 months of follow-up the patient is doing well.
Discussion
Double aortic arch is the most common complete vascular ring and comprises 1% of operable congenital cardiac disease [1]. The right arch is dominant in 75% of cases, while the left arch is dominant in 20% cases. In 5% cases, there is co-dominance [2,3]. Symptoms depend on the degree of tracheal and oesophageal compression. The most common cyanotic congenital heart lesions associated with DAA are TOF and transposition of great arteries [4]. TOF is a well described cyanotic congenital cardiac anomaly, characterized by the presence of infundibular septal deviation, right ventricular out flow obstruction, aortic override and right ventricular hypertrophy [3]. The gold standard investigation in TOF is cardiac catheterization, however MR angiography can also prove useful [5].
Zhou Dan et al. in a series of 15 cases of double aortic arch with associated cardiac anomalies, have recommended the median sternotomy approach [6].
Staged repair of TOF with DAA via median sternotomy followed by posterolateral thoracotomy at a later date has been reported [4]. Talwar et al. described the repair of double aortic arch via postero-lateral thoracotomy and the cardiac malformation via sternotomy in the same setting [7]. The non-dominant arch is divided at the atretic segment. In the absence of an atretic segment the non-dominant arch is divided between the ipsilateral subclavian artery and the descending aorta [2,8]. The distal non-dominant arch beyond the ipsilateral subclavian artery is often difficult to access from the midline, and accounts for the controversy regarding the approach (thoracotomy vs. median sternotomy). The exposure to the non-dominant arch is limited from median sternotomy owing to its posterior turn, causing difficulty in placing clamps and still having enough length to cut and over sew. We modified the placement of clamps to simplify the division of non-dominant arch. We used a combination of 2 vascular clamps and one vascular loop to achieve this (Figure 5). The limited dissection of the arch beyond the left subclavian artery also prevented the divided segment from retracting posteriorly. The fibrous ring around the trachea which is invariably present must be divided to avoid recurrence of tracheal obstruction.
Conclusion
Double aortic arch can be associated with various congenital cardiac anomalies. The difficulty in handling the non-dominant arch from the midline accounts for the prevalence of the two incision approach wherein the arch is tackled by a separate posterolateral thoracotomy. We believe that division of the non-dominant arch can be safely undertaken from the midline when coexisting cardiac anomalies mandate an intracardiac repair under cardiopulmonary bypass which also facilitates division of the non-dominant arch.
References
- Harper AR, Dai M, Prabhatha RM (2011) Tetralogy of fallot with double aortic arch. Cardiol Young 21: 695-696.
- Emani SM (2010) Sabiston &Spencer: Surgery of the Chest. Elsevier, USA.
- Kouchoukos NT, Blackstone EH, Kirklin JK, Hanley FL (2012) Kirklin/Barratt-Boyes: Cardiac Surgery. Elsevier, USA.
- Pankaj B, Munesh T, Bhan A (2013) Dysphagia in an adult tetralogy of fallot with double aortic arch. Images Paediatr Cardiol 15: 6-13.
- Romeih S, Al-Sheshtawy F, Salama M, Blom NA, Abdel-Razek A, et al. (2012) Comparison of contrast enhanced magnetic resonance angiography with invasive cardiac catheterization for evaluation of children with pulmonary atresia. Heart Int 7: e9.
- Dan Z, Qiangfu H, Liang T, Changyu L, Linnan D, et al. (2016) Repair of double aortic arch in patients with concomitant cardiac anomalies. J Card Surg 31: 635-638.
- Sachin T, Anubhav G, Shiv KC, Balram A (2009) Absent left pulmonary artery and double aortic arch in tetralogy of fallot: reconstruction using homograft saphenous vein or iliac artery. Interact CardioVasc Thorac Surg 8: 277-279.
- McElhinney DB (2015) Double aortic arch treatment & management. Pediatrics: cardiac disease and critical care medicine.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences