Giant Coronary Artery Aneurysm after Drug-Eluting Stent (DES) Implantation: Therapeutic Challenges and Management
Baruah DK and Tanuja P
DOI10.21767/2573-4482.100033
1Senior Consultant Cardiologist, Director Cath. Lab., Apollo Hospitals, Visakhapatnam, Andhra Pradesh, India
2Cardiology, Apollo Hospitals, Visakhapatnam, Andhra Pradesh, India
- *Corresponding Author:
- Baruah DK
Apollo Heart Institute
Waltair Main Road, Visakhapatnam 530002, Andhra Pradesh, India.
Tel: 8912508881
Fax: 8912508881
E-mail: baruahdk_9@yahoo.com
Received Date: December 13, 2016; Accepted Date: January 03, 2017; Published Date: January 06, 2017
Citation: Baruah DK, Tanuja P. Giant Coronary Artery Aneurysm after Drug-Eluting Stent (DES) Implantation: Therapeutic Challenges and Management. J Vasc Endovasc Surg. 2017, 2:1. doi: 10.21767/2573-4482.100033
Abstract
Implantation of drug-eluting stent can result a rare complication of coronary artery aneurysm. We report a case of giant coronary artery aneurysm presented with acute myocardial infarction, which was successfully treated by sequential implantation of two covered stents. At 2-month follow-up, the patient presented with mass effect of the thrombosis aneurysm compressing the right ventricle, improved with conservative management.
Keywords
Balloon angioplasty; Coronary artery; Aneurysm
Introduction
Introduction of Drug-Eluting Stent (DES) proved to be an important step forward in reducing rates of restenosis and target lesion revascularization after percutaneous coronary intervention, but at the same time potentially causing serious complications. One of the rare complications of DES is coronary artery aneurysm. Coronary Artery Aneurysm (CAA), defined as localized dilatation of the coronary artery exceeding 50% of the reference vessel diameter is considered as very rare, with a reported incidence of 0.3-6% after percutaneous coronary intervention [1]. It is termed as giant if diameter exceeds the reference vessel diameter by four times or if the aneurysm is 8 mm or more [2]. Possible mechanisms of aneurysm formation after DES implantation are delayed re-endothelialization, inflammation, and hypersensitivity reactions, apart from deep arterial wall injury (rupture or resection of the vessel media), and residual dissection [3,4]. Treatment of CAA is somewhat controversial, and there is no consensus on the modality of treatment in a given clinical situation. We report a case of giant CAA after DES implantation presenting with acute myocardial infarction and cardiogenic shock, which was treated by percutaneous coronary intervention using two sequential covered stents.
Case Report
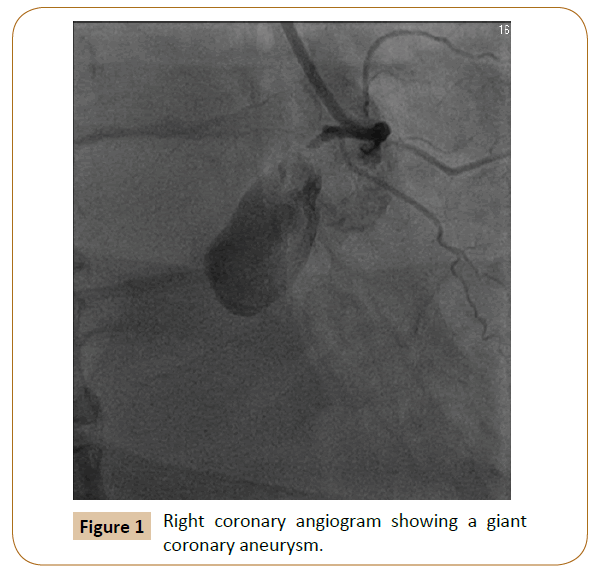
A 70 year old diabetic male presented to our institution with severe retrosternal chest pain of 10 h duration. He underwent Percutaneous Coronary Intervention (PCI) and stenting to Right Coronary Artery (RCA) using Everolimus Eluting Stent (Xience Pro, Abbott Vascular) in another city hospital 36 days prior to this episode. On general examination, the patient was restless, with profuse sweating and cold extremities. His pulse rate was 52/ min, regular, low volume; with blood pressure of 85/56 mm Hg. Examination of cardiovascular system did not reveal any specific findings except muffle heart sounds. 12-lead electrocardiogram showed sinus bradycardia, and inferior ST-elevation myocardial infarction (3 mm ST elevation in lead II, III, and AVF). Cardiac bio-marker was grossly elevated (Troponin-I=3564 ng/ml). Echocardiogram revealed inferior and posterior hypokinaesia, mild mitral regurgitation, and moderate left ventricular dysfunction (LVEF-44%). At this stage, probable clinical diagnosis was early (sub-acute) stent thrombosis. Patient was treated with intravenous 5% normal saline and injection dopamine at 5 μg/ kg of body weight administered intravenously. His hemodynamic condition did not show much improvement. So, it was decided to subject him for coronary angiogram with the intention to do primary PCI. After informed consent, coronary angiogram was done from right radial route which revealed normal left main, mild disease of left anterior descending coronary artery with 70 -80% stenosis of the first diagonal, and normal left circumflex artery. Right coronary injection revealed opening of the proximal right coronary artery into a large spherical cavity (22 mm in diameter) that filled with contrast medium in a swirling fashion with slow opacification without visualization of the distal artery (Figure 1).
Therapeutic Challenges and Management
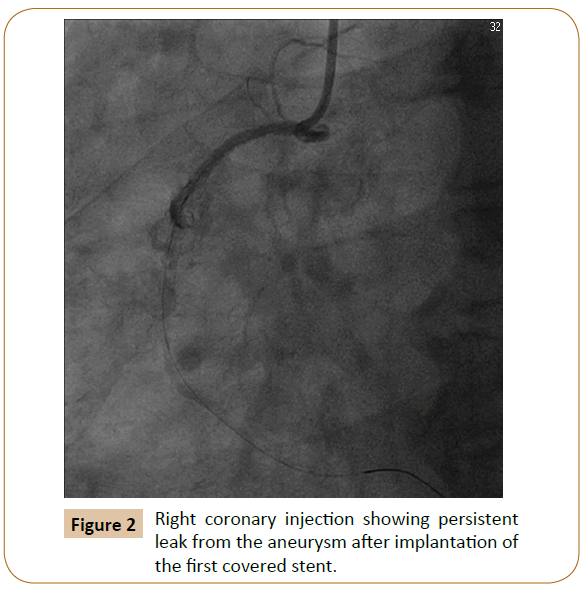
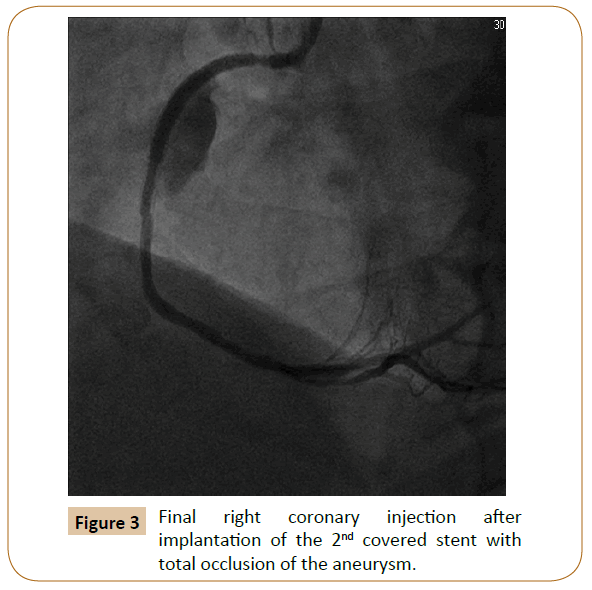
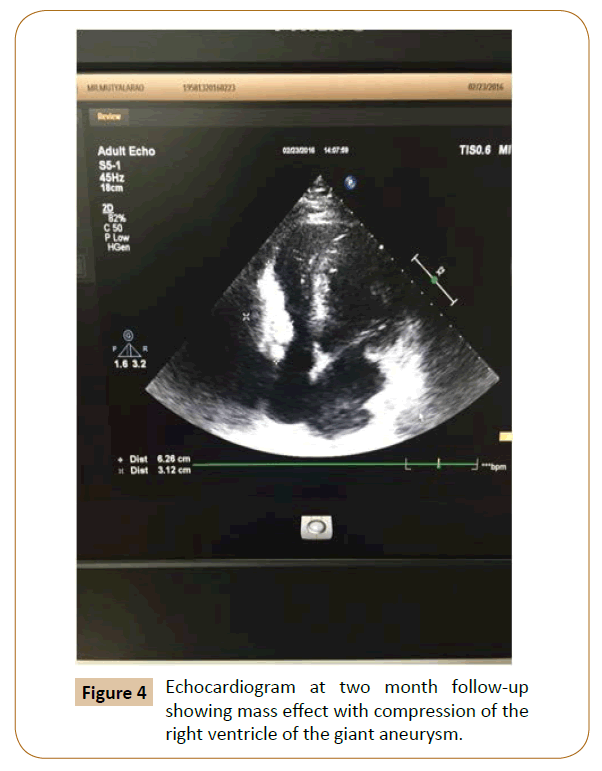
Despite an important anatomical abnormality of the coronary artery, the treatment options of CAAs are still poorly defined. Therefore, in real world practice, it poses a challenge to cardiologist in deciding the modality of treatment. Nevertheless, depending on clinical condition, etiology and associated lesions, either medical treatment (anti-platelet drugs, anti-coagulation) or PCI, and surgical repair can be considered [5]. In our case, surgery was considered; but our cardiothoracic team opined a very high surgical risk in that clinical situation. Therefore, we opted for percutaneous treatment as an alternative mode of therapy. However, there were certain challenging issues for percutaneous approach in this case: 1) Nature of the aneurysm-true or false, and related risk of aneurysm rupture during intervention. 2) Inability to delineate the full extension of the aneurysm as well as the distal coronary artery, and thus difficulty in assessing the distal landing zone of stent or any device. 3) Rapidly deteriorating condition of the patient preventing proper pre-assessment and planning. In fact, due to rapidly deteriorating hemodynamic condition we had to introduce Intra-Aortic Balloon Pump (IABP) from right femoral approach. Right coronary artery was engaged with a 6 French Right Judkin's guide catheter. A 014 inch soft floppy tipped guide wire was used to cross the stent, but it was repeatedly falling into the aneurismal sac. Finally, after repeated attempts stent could be crossed and wire was parked distally. Proximal end of the stent was gradually dilated with a 1.2 mm × 6 mm, and 2 mm × 10 mm balloons with a final dilatation using 3 × 15 mm non-compliant balloon at 12 atmospheric pressure. A 2.8 mm × 19 mm covered stent (Graft- Master, Jostent, Abbott Vascular Devices, Santa Clara, Calif.) was positioned at the point from where the aneurysm was thought to be filled, and was deployed at 18 atmospheric pressure. Post angiogram showed persistent leak into the aneurysm (Figure 2). Another 3.5 mm × 19 mm covered stent (Graft-master Jostent, Abbott Vascular Devices, and Santa Clara, Calif.) was just distal to the first stent and deployed at 14 atmospheric pressure. Post angiogram showed total occlusion of the aneurysm with good distal flow (Figure 3). His hemodynamic condition gradually improved with an uneventful recovery, and was discharged on 4th postoperative day. At 2 months follow up, the patient presented with breathlessness on exertion of NYHA class II, and ECG revealed old inferior wall MI. Transthoracic echocardiogram showed a large echogenic mass (thrombosed aneurysm) to-wards the free walls right ventricle with moderate compression of its cavity (Figure 4), with mild left ventricular dysfunction (LVEF-48%). He was prescribed additional low dose of diuretics, and at 90-days, he had significant improvement of symptoms though the echocardiographic findings remained the same. At one year follow up, the patient was asymptomatic and his left ventricular function improved to 51%.
Discussion
Coronary artery aneurysms after percutaneous coronary intervention are rare, with a reported incidence of 0.3% to 6.0%; and giant CAAs are very rare with a reported incidence of 0.02% [6]. Majority of giant CAAs involve the RCA adjacent to the right atrium, indicating that the adjacent area of atrial tissue is weak that helps in the formation and enlargement of aneurysm [7]. Commonest cause of CAA in adult is atherosclerosis; however, other causes include Kawasaki's disease, autoimmune disease (polyarteritis nodosa, systemic lupus erythematosus, and scleroderma), rheumatic, mycotic coronary emboli, syphilis, trauma, coronary artery dissection, congenital cause, and angioplasty [8]. Recently, with the advent of drug eluting stents there have been increasing reports of CAA implicating its role in the pathogenesis of coronary aneurysm. The proposed mechanism of stent-related aneurysm formation is multi-factorial. Inflammatory and allergic reactions to different metals like nickel and molybdenum have been reported after BMS implantation [9]. The triggers for inflammatory and allergic reactions after DES implantation are more complex because DES consists of 3 components: The anti-restenotic drug, the drug carrier vehicle (polymer), and the stent platform. Immunosuppressant used in DES such as Sirolimus inhibits inflammation, and chemotherapeutic agents like Paclitaxel, which is an anti-inflammatory agent, inhibits cell proliferation. In due course of time, once drug is eluted, the polymer in which the drug is embedded may elicit a hypersensitivity reaction and vasculitis that results in weakening of vessel wall and subsequent dilatation [10]. Mechanical factors considered in the formation of CAA are oversized balloons or high-pressure balloon inflation resulting in intimal and medial tear with weakening and stretching of the artery 3. These mechanical consequences may finally lead to the perforation of the media without penetration of blood through the adventitia resulting in aneurysm formation. Other possible contributory mechanisms of aneurysm are incomplete endothelialization of DES, and late acquired incomplete stent apposition, which is observed in 8% to 10% of patients with DES [10]. The stent used in our case was an Evorulimus-eluting polymer coated stent, but technical details of angioplasty were not known as it was performed in another centre.
In a review of coronary artery aneurysm, Jiro Aoki and others described three different types of aneurysms after DES or BMS implantation [11]. Type I aneurysm is a type of aneurysm that demonstrates rapid early growth with pseudo aneurysm formation detected within 4 weeks.
Arterial injury related to procedure is the likely contributor to aneurysm formation in these cases rather than the chronic arterial response to the stent, polymer, and drug. Type II aneurysm presents slowly (sub-acute to chronic), and usually is detected within 6 months or more after the procedure. Chronic arterial response to components of stent is considered as the basis for this type of aneurysm formation. Finally, Type III aneurysm is of mycotic or infectious in etiology. This is rare, and patients typically present with systemic manifestations and fever secondary to bacteremia. Our case has characteristics of type I aneurysm [12].
Conclusion
This case has demonstrated a giant coronary artery aneurysm after drug-eluting stent implantation, with its serious consequences, and percutaneous management using sequential covered stents in a difficult clinical scenario.
References
- Slota PA, Fischman DL, Savage MP, Rake R, Goldberg S (1997) Frequency and outcome of development of coronary artery aneurysm after intracoronary stent placement and angioplasty. STRESS Trial Investigators. Am J Cardiol 79: 1104-1106.
- Kato H, Sugimura T, Akagi T, Sato N, Hashino K, et al. (1996) Long-term consequences of Kawasaki disease: 10-21-year follow-up study of 594 patients. Circulation 94: 1379-1385.
- Bell MR, Garratt KN, Bresnahan JF, Edwards WD, Holmes DR (1992) Relation of deep arterial resection and coronary artery aneurysms after directional coronary atherectomy. J Am Coll Cardiol 20:1474-1481.
- Virmani R, Liistro F, Stankovic G (2002) Mechanism of late in-stent restenosis afterimplantation of apaclitaxel derivate-eluting polymer stent system in humans. Circulation 106: 2649-2451.
- Virmani R, Guagliumi G, Farb A (2004) Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation109: 701-705.
- Dianyuan L, Wu Q, Sun L, Song Y, Wang W, et al. (2005) Surgical treatment of giant coronary artery aneurysm. J Thorac Cardiovasc Surg 130:817-821.
- Nichols L, Lagana S, Parwani A (2008) Coronary artery aneurysm: a review and hypothesis regarding etiology. Arch Pathol Lab Med 132: 823-828.
- Nobrega TP, Klodas E, Breen JF, Liggett SP, Higano ST, et al. (1996) Giant coronary artery aneurysms and myocardial infarction in a patient with systemic lupus erythematosus.Cathet Cardiovasc Diagn 39: 75-79.
- Wright WP, Alpert MA, Mukerji V, Santolin CJ (1991) Coronary artery aneurysm-a case study and literature review. Angiology42: 672-679.
- Koster R, Vieluf D, Kiehn M (2000) Nickel and molybdenum contact allergies in patients with coronary in-stent restenosis. Lancet 356: 1895-1897.
- Ako J, Morino Y, Honda Y (2005) Late incomplete stent apposition after sirolimus-eluting stent implantation: a serial intravascular ultrasound analysis. J Am Coll Cardiol 46: 1002-1005.
- Aoki J, Kirtane A, Leon MB (2008) Coronary Artery Aneurysms after Drug-Eluting Stent Implantation.JAm Coll Cardiol 1: 14-21.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences