Great Saphenous Vein Aneurysm and Venous Thromboembolism: A Case Report
Leon LR, Labropoulos N, Vazquez F and Pacanowski JP
DOI10.21767/2573-4482.20.05.5
1Department of Vascular and Endovascular Surgery at University of Arizona, Tucson, Arizona, USA
2Department of Vascular and Endovascular Surgery at Pima Vascular, Tucson, Arizona, USA
3Department of Vascular and Endovascular Surgery at StonyBrook, Long Island, New York, USA
4Universidad Autonoma de Guadalajara Medical School, Guadalajara, Mexicon
- *Corresponding Author:
- Leon LR Department of Vascular and Endovascular Surgery at University of Arizona Tucson, Arizona, USA Tel: +1-708-651-4242 E-mail: luisrleon1@gmail.com
Received Date: November 21, 2019; Accepted Date: May 04, 2020; Published Date: May 11, 2020
Citation: Leon LR, Labropoulos N, Vazquez F, Pacanowski JP (2020) Great Saphenous Vein Aneurysm and Venous Thromboembolism: A Case Report J Vasc Endovasc Therapy Vol.5 No.2:5
Abstract
Introduction: True aneurysmal degeneration of the great saphenous vein (GSV) is unusual. We report a case of venous thromboembolism due to a large GSV aneurysm.
Case report: A 59-year old man presented with a painful left groin lump. The patient had 7 years prior a diagnosis of a GSV aneurysm. During that period of time, he was not offered surgical treatment and eventually suffered an episode of symptomatic pulmonary embolism. Doppler ultrasound exam revealed a 4-cm GSV aneurysm. Aneurysmectomy was performed uneventfully.
Discussion and conclusions: Aneurysmal GSV degeneration is a relatively rare occurrence and has been infrequently described. Its described management strategies are varied but in most it seems that excision with SFJ ligation would be the most safe and effective therapeutic option. Further studies are needed.
Keywords
Great saphenous vein; Venous thromboembolism; Arthroscopy
Introduction
Great saphenous vein (GSV) aneurysms are relatively infrequently reported in the literature [1-13]. We report a case of a longstanding aneurysm of the GSV in a patient with a history of pulmonary embolism (PE).
Case Report
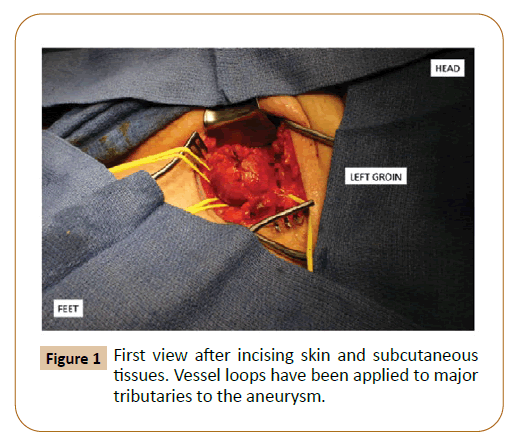
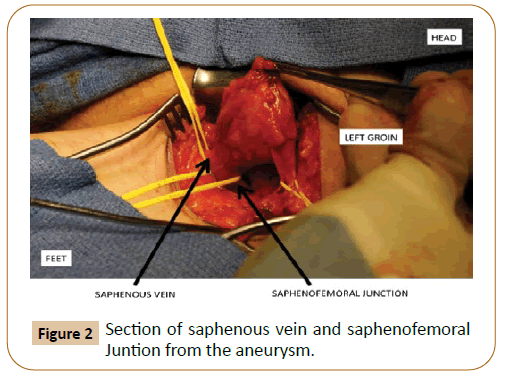
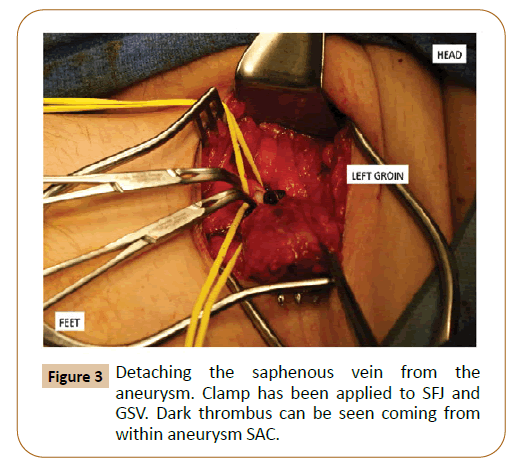
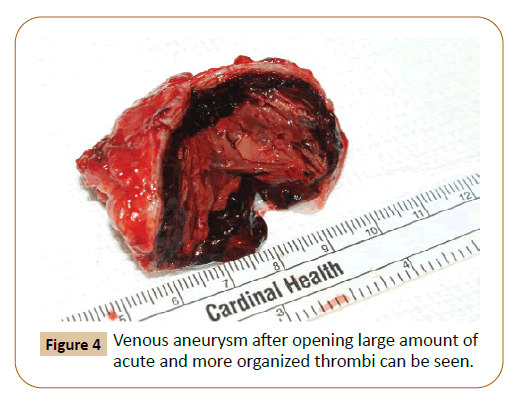
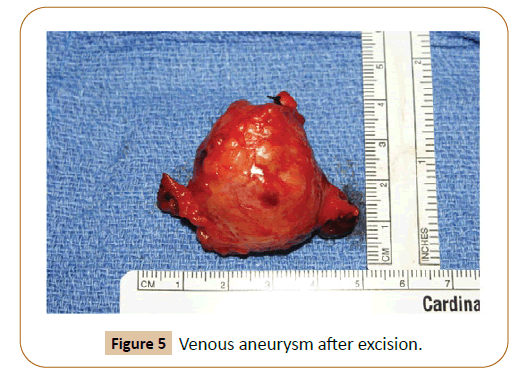
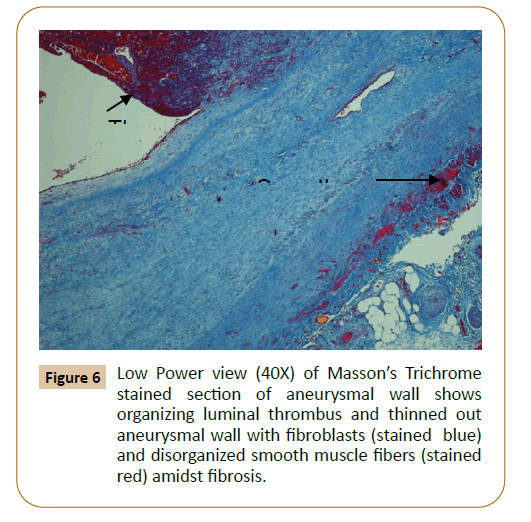
A 59 year-old Greek Orthodox Monk male presented to our office with a tender left groin mass and bilateral lower extremity severe heaviness, discomfort and swelling, associated with visible varicose veins. With the exception of benign prostate hypertrophy, hypertension and osteoarthritis the patient was quite healthy. He never used tobacco products and his only past surgery was a knee arthroscopy. He did report that his mother had a propensity to form blood clots and had suffered multiple PE but had himself never been diagnosed with a thrombophilia. Interestingly, he first was diagnosed with a GSV aneurysm seven years prior his current presentation when being evaluated for nonspecific abdominal pain. Ultrasound at that time described a compressible 3.3-cm x 4.1-cm aneurysm of the left GSV. He was lost to follow up from that admission until six years later when he presented to a local emergency department with acute shortness of breath and pleuritic chest pain. During evaluation he was found to have numerous bilateral PE and was again noted to have a left GSV aneurysm without another embolic source. He was started on Coumadin and was followed by his primary care physician but without any definitive therapy to address the venous aneurysm. The patient eventually presented again a year later with complaints of pain over the left groin mass and it was at this point that we established contact with him. He underwent a repeated ultrasound, which re-demonstrated a 3-cm x 4-cm left GSV aneurysm as well as severe reflux of the GSV bilaterally. Due to his history of PE, continued groin pain and significant disability from reflux symptoms in both legs, the patient elected to undergo aneurysm excision and bilateral GSV stripping. At surgery, the aneurysm was found to be 3-cm x 4-cm near the sapheno-femoral junction SFJ (Figures 1-4). On sectioning it was found to have a thick wall with significant acute and chronic thrombus (Figure 5). The patient followed an uncomplicated postoperative course and has returned to his monastic duties. (Figure 6)
Discussion
Aneurysmal GSV degeneration is a relatively rare phenomenon that has been infrequently studied to date. As far as their etiology, increased venous flow and turbulence adjacent to arteriovenous malformations might lead to primary venous aneurysms. Some GSV aneurysms have been described as a result of complications from surgery [14] or after drug injection [15]. However this was not the case of our patient who appeared to suffered from a primary aneurysm.
While venous aneurysms of the deep system in the lower extremities are well recognized as a risk for thrombosis and PE, aneurysms of the GSV also carry this risk [1,3]. Sequelae of thrombosis and PE are most frequently reported in addition to symptoms associated with mass effect and venous reflux. Often these patients present for surgical evaluation of a hernia or soft tissue mass and the diagnosis is sometimes missed. With more patients undergoing duplex interrogation of their lower extremities, venous aneurysms of the lower extremities are being found with increasing regularity. A diagnostic confusion with other etiologies (i.e. soft tissue masses, inguinal hernias), and delayed in definitive therapy, could both affect prognosis just like in the case of our patient. Delay in diagnosis or surgical therapy increase the risk of thromboembolism and death.
The natural history of these aneurysms is uncertain and, as such, management is variable. A review of the literature revealed management strategies ranging from chronic anticoagulation to ligation with or without excision to excision with interposition grafting with the goal to preserve the continuity of the GSV [1-5]. In the popliteal vein, the risk of PE despite therapeutic anticoagulation with Coumadin is as high as 30%. There are several case reports of PE from aneurysms of the GSV despite anticoagulation [1,3] In the majority of patients it would seem that excision with SFJ ligation would provide the most durable and expedient solution with a low overall risk of morbidity and mortality. We admit however that some bias cannot be excluded from our comments and therefore, further study of the natural history and the methods to treat these aneurysms is warranted.
Conclusion
Pathologic descriptions of venous aneurysms are few. Histologic cross sections of a venous aneurysm often show the aneurysm wall to be composed of focally thinned and disorganized smooth muscle with luminal thrombosis in some cases.
Conflicts of Interests
None
References
- Gillespie DL, Villavicencio JL, Gallagher C, Chang A, Hamelink JK, et al. (1997) Presentation and management of venous aneurysms. J Vasc Surg 26: 845-852.
- Chen SI, Clouse WD, Bowser AN, Rasmussen TE (2009) Superficial venous aneurysms of the small saphenous vein. J Vasc Surg 50: 644-647.
- Pascarella L, Al-Tuwaijri M, Bergan JJ, Mekenas LM (2005) Lower extremity superficial venous aneurysms. Ann Vasc Surg 19: 69-73.
- Akoudad H, Chaouki S, Cherti M, Benmimounm EG, Arharbi M (2001) Aneurysm of the internal saphenous vein: report of a case. Ann Cardiol Angeiol 50: 142-145.
- Wu EH, Kong C, Hsieh IC, Lien LC (2008) Great saphenous vein thrombosis causing acute pulmonary embolism suggested by combined CT venography and pulmonary angiography. Emerg Radiol 15: 263-265.
- Keshelava G, Beselia K, Nachkepia M, Chedia S, Janashia G, et al. (2011) Surgical treatment of the great saphenous vein aneurysm resulting in pulmonary embolization in two patients. Ann Vasc Surg 25: e13-e15.
- Spanos K, Giannoukas AD (2016) Surgical Treatment of a Thrombosed Proximal Great Saphenous Vein Aneurysm. Eur J Vasc Endovasc Surg 51: 274.
- Kota AA, Stephen E, Samuel V, Premkumar P, Selvaraj D, et al. (2018) Primary great saphenous vein aneurysm in a child. J Vasc Surg Venous Lymphat Disord 6: 765.
- De Miranda JS, Damous SH, Júnior MP, Yoo JH, Yassushi ET, et al. (2015) Great saphenous vein aneurysm: A differential diagnosis of femoral hernia and review. Int J Surg Case Rep 8: 154-157.
- Çiçek MC, Çiçek ÖF, Yalçınkaya A, Taşoğlu I (2015) Groin swelling in a four-year-old boy: primary great saphenous vein aneurysm. Ann Vasc Surg 29: e11-e12.
- Simsek E, Bugra O (2014) Great saphenous vein aneurysm presenting as an inguinal hernia. Asian J Surg 37: 208-210.
- Plett M, Hofmann SC, Kusenack U, Lehmann P (2014) Atypical aneurysm of the great saphenous vein clinically presenting as a subcutaneous tumor of the thigh. J Dtsch Dermatol Ges 12: 511-513.
- Hosokawa Y, Yoneda K, Nakai K, Moriue J, Kubota Y (2013) Completely thrombosed venous aneurysm in great saphenous vein. Ann Dermatol 25: 268-270.
- Eidson JL, Shepherd LG, Bush RL (2008) Aneurysmal dilatation of the great saphenous vein stump after endovenous laser ablation. J Vasc Surg 48: 1037-1039.
- Marković M, Dragaš M, Koncar I, Banzić I, Pejkić S, et al. (2016) Secondary venous aneurysm following intravenous drug abuse: A case report. Vojnosanit Pregl 73: 500-503.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences