Intraoperative Anterior Scalene Anomaly in a Patient with Arterial and Neurogenic Thoracic Outlet Syndrome
Dominique L. Tucker and Julie Ann Freischlag
DOI10.36648/2634-7156.21.6.14
Dominique L. Tucker1,2 and Julie Ann Freischlag1*
1Department of Vascular and Endovascular Surgery, Wake Forest Baptist Medical Center, Winston-Salem, USA
2Case Western Reserve University School of Medicine, Health Education Campus, Cleveland, USA
- *Corresponding Author:
- Julie Ann Freischlag
Department of Vascular and Endovascular Surgery, Wake Forest Baptist Medical Center, Winston-Salem, USA
Tel: +3367163408
E-mail: jfreisch@wakehealth.edu
Received Date: February 21, 2021; Accepted Date: March 23, 2021; Published Date: March 30, 2021
Citation: Dominique LT, Julie AF (2021) Intraoperative Anterior Scalene Anomaly in a Patient with Arterial and Neurogenic Thoracic Outlet Syndrome. J Vasc Endovasc Ther. 6 No. 3: 14.
Abstract
Compression of the neurovascular structures of the upper extremity as they pass through the thoracic outlet result in thoracic outlet syndrome. The myriad of symptoms associated with the syndrome vary based on the structure(s) compressed: the subclavian artery/vein or the inferior trunk of the brachial plexus. This is a common site of compression especially in the presence of upper extremity injury, overuse or anatomical abnormalities. Majority of patients present with neurogenic pain and weakness; herein, we present the case of a patient with symptoms of both arterial and neurogenic compression caused by aberrant anterior scalene anatomy. These patients are excellent surgical candidates for first rib resection and anterior scalenectomy. A transaxillary approach offers the clinician an adequate window to identify anatomical abnormalities intraoperatively and safely excise the first rib and anterior scalene muscle.
Introduction
Thoracic outlet syndrome (TOS) involves the compression of the neurovascular structures coursing through the thoracic outlet and presents in three forms: neurogenic, venous, and arterial. NTOS is the most common form of TOS, comprising approximately 94-97% of TOS patients presenting secondary to compression of the inferior trunk of the brachial plexus [1]. Neurogenic TOS patients are classically females in the 3rd to 5th decade of life, who present with pain, weakness, numbness and parenthesis of the upper extremity [2]. Arterial TOS, the least common subtype (~1-2% of total patients), presents with acute or chronic ischemia secondary to aneurysm, occlusion or thromboembolisation of the subclavian artery [1]. Patients present with upper extremity pain, white pallor in the hands, and decreased pulses.
Neurogenic TOS presenting with arterial symptoms can be seen frequently, comprising ~5% of patients [3,4]. Concomitant arterial and neurogenic symptoms lead to earlier presentation refractory to conservative management. Conservative management, such as physical therapy and scalene blocks, are contraindicated in ATOS as chronic arterial compression increases endothelial wall stress increasing the risk of subclavian sequels [5]. First rib resection and anterior scalenectomy (FRRAS) has demonstrated improvement in both the patient’s quality of life, as measured by SF-12 and DASH scores, and alleviation of symptoms [4]. We present the case of a patient with symptoms of both arterial and neurogenic compression caused by aberrant anterior scalene anatomy.
Case Presentation
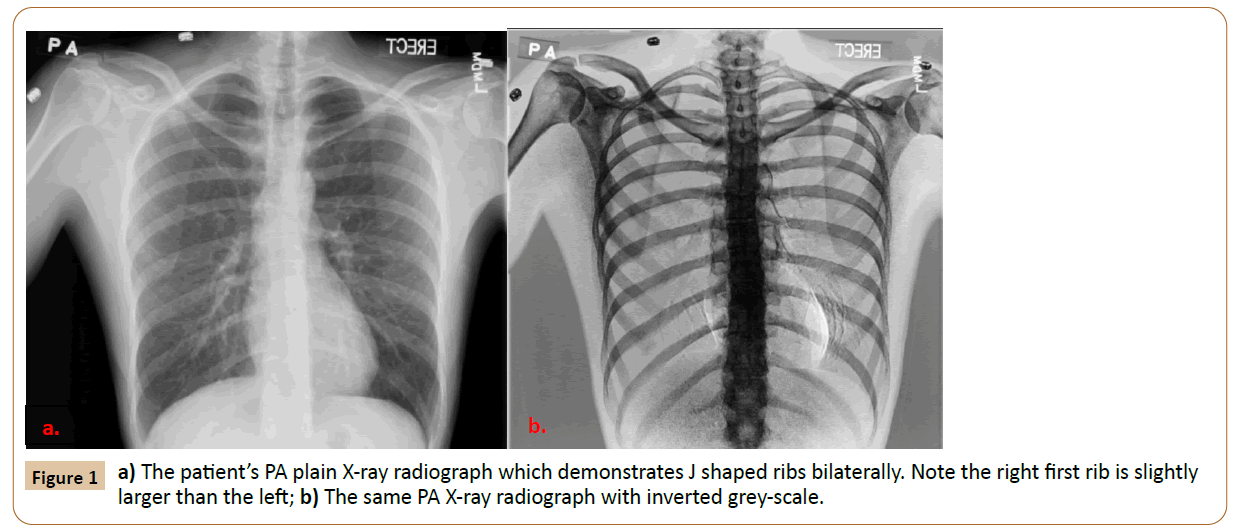
A 36-year-old female right hand dominant construction worker presented with a ten-year history of bilateral pain, paresthesias, pallor, and discomfort in their bilateral upper extremities. The patient’s symptoms began during deployment in Iraq while carrying heavy body packs and tactical body armor each day. In high school, the patient played volleyball and ran track, but noticed no symptoms. The patient had failed multiple courses of physical therapy since symptoms began. Symptoms were worse at night, and previous medications prescribed included Percocet and Lortab which interrupted with the patient’s current work responsibilities. Physical examination showed a large right anterior scalene and a positive bilateral elevated arm stress test (EAST) with pallor and fatigue of the right hand at 15 seconds. Adson test was positive bilaterally with right-sided pulse obliteration. Strength was decreased bilaterally in the ulnar distribution. Her chest X-ray demonstrated small cervical ribs bilaterally, with exaggerated J shaped first ribs-the right was larger than the left (Figure 1). The patient was diagnosed with right neurogenic TOS (NTOS) with arterial compression on abduction with failure to improve with physical therapy.
A right transaxillary FRRAS was performed. Intraoperatively, the patient was found to have a prominent lower first rib and an anatomic variant of the anterior scalene, which originated posterior to the subclavian artery with a small slip of muscle anterior to the artery. The small slip of muscle anterior to the artery was divided, and the large scalene muscle posterior to the artery was removed without difficulty along with the first rib. The patient had an uneventful recovery and was discharged home on post-operative day one. Post-operative right-sided paresthesia was treated with gabapentin, and the patient now experiences no symptoms.
A year later, the patient’s symptoms progressed on the left side. Physical examination showed a large, tender left anterior scalene and a positive EAST in left arm with pain and fatigue at 30 seconds. Adson test was positive on the left side. Strength was decreased in an ulnar and radial distribution. The patient was diagnosed with left NTOS, and a left transaxillary FRRAS was performed. Intraoperatively, the subclavian vein, artery and brachial plexus were found in typical anatomic position, and the operation proceeded without complications.
Discussion
The anatomic variant of the scalene muscle encasing the surrounding structures predisposed the patient to neurovascular compression on the right side, but not the left. Compression of the neurovascular bundle as it transverses the scalene triangle likely occurred secondary to anatomic abnormalities, repeated trauma and physical activity in our patient. Typically, the anterior scalene muscle is anterior to subclavian artery and inferior truck with the middle scalene posterior to these structures. However, common variants where the superior trunk (C5, C6) pierce the anterior scalene predispose to NTOS [6]. The presence of a scalenusminimus muscle is found unilaterally in 46% of adult cadavers-this muscle originates from the transverse process of C6/7 and inserts at the first rib distal to the artery [7]. In a study of 102 cadavers, 1 had a subclavian artery that pierced the anterior scalene [7]. Anatomic variation in the neck is common, “textbook,” neck anatomy was found in 14% of the aforementioned cadavers, and highlights the importance of preoperative imaging in TOS which decrease the diagnostic burden and facilitate management [7].
A higher incidence of bony abnormalities, such as a cervical rib, is found in TOS patients; bony abnormalities predispose to neurovascular compression, and removal of the cervical rib along with the first rib and anterior scalene is appropriate to provide symptomatic relief [8,9]. Cervical ribs are twice as common in women, and complete resection results in better alleviation of symptoms compared to thrombolytics alone [10]. While this patient did not have prominent cervical ribs, the presence of the J shaped rib, in our experience, can similarly cause compression of the nerve root due to its inferior course. Moreover, acquired hypertrophy of the scalene muscle from repetitive use of the upper extremity, seen in athletes and abnormal muscle attachments can narrow the space through which neurovascular bundles pass. This chronic inflammation from repeated trauma results in fibrosis and scarring of the extravascular space.
Conclusion
The presence of bony and muscular anomalies in the scalene triangle are predisposing factors for TOS, and these patients are excellent surgical candidates for FRRAS. Clinicians should note these abnormalities and watch patients for new onset symptoms contra-laterally.
Acknowledgements and Disclosures
The authors declare no relevant industry financial disclosures or conflicts of interest.
Patient’s Informed Consent
The patient was consented, and gave permission for this publication.
References
- Freischlag J, Orion K (2014) Understanding thoracic outlet syndrome. Scientifica (Cairo)14:1-6.
- Orlando MS, Likes KC, Mirza S, Cao Y, Cohen A, et al. (2015) A decade of excellent outcomes after surgical intervention in 538 patients with thoracic outlet syndrome. J Am Coll Surg 220: 934-939.
- Likes K, Rochlin DH, Call D, Freischlag JA (2014) Coexistence of arterial compression in patients with neurogenic thoracic outlet syndrome. JAMA surgery 149: 1240-1243.
- Chang DC, Rotellini-Coltvet LA, Mukherjee D, De Leon R, Freischlag JA (2009) Surgical intervention for thoracic outlet syndrome improves patient’s quality of life. J Vasc Surg 49:630-637.
- Marine L, Valdes F, Mertens R, Kramer A, Bergoeing M, et al. (2013) Arterial thoracic outlet syndrome: a 32-year experience. Ann Vasc Surg 27:1007-1013.
- Leonhard V, Smith R, Caldwell G, Smith HF (2016) Anatomical variations in the brachial plexus roots: implications for diagnosis of neurogenic thoracic outlet syndrome. Ann Anat Anz 206: 21-26.
- Harry WG, Bennett JD, Guha SC (1997) Scalene muscles and the brachial plexus: anatomical variations and their clinical significance. Clinical anatomy: The Official Journal of the American Association of Clinical Anatomists and the British Association of Clinical Anatomists. 10:250-252.
- Henry BM, Vikse J, Sanna B, Taterra D, Gomulska M, et al. (2018) Cervical rib prevalence and its association with thoracic outlet syndrome: a meta-analysis of 141 studies with surgical considerations. World Neurosurg 110:e965-e978.
- Chang KZ, Likes K, Davis K, Demos J, Freischlag JA (2013) The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg 57:771-775.
- Sanders RJ, Hammond SL (2002) Management of cervical ribs and anomalous first ribs causing neurogenic thoracic outlet syndrome. J Vasc Surg 36: 51-56.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences