Post-traumatic Hepatic Artery Pseudoaneurysm after Blunt Abdominal Trauma Treated by Embolization with Cyanoacrylate Injection: A Case Report and Review of the literature
Abreu IESG, Diogenes CA, Chaves FKP and Ferreira BRS
DOI10.21767/2573-4482.18.03.25
Abreu IESG*, Diogenes CA, Chaves FKP and Ferreira BRS
Department of Vascular Surgery, Hospital Geral Fortaleza, Bento Albuquerque, Fortaleza, Brazil
- *Corresponding Author:
- Dr. Italo Eugenio Souza Gadelha De Abreu
Department of Vascular Surgery
Hospital Geral Fortaleza
Bento Albuquerque, Fortaleza, Brazil
Tel: 558632624563
Fax: 558696865271
E-mail: italoeugenioabreu@gmail.com
Received Date: October 20, 2018; Accepted Date: December 11, 2018; Published Date: December 18, 2018
Citation: Abreu IESG, Diogenes CA, Chaves FKP, Ferreira BRS (2018) Post-traumatic Hepatic Artery Pseudoaneurysm after Blunt Abdominal Trauma Treated by Embolization with Cyanoacrylate Injection: A Case Report and Review of the literature. J Vasc Endovasc Therapy. 3:25.
Abstract
Introduction: Post-traumatic hepatic artery pseudoaneurysm is uncommon. It must always be treated due to the high risk of complications, especially its rupture.
Presentation of case: The aim of this study is to report a case of a patient suffering from blunt abdominal trauma that showed extensive liver laceration that underwent a surgical approach with hemostatic rabies.
Discussion: In the postoperative period, the presence of a pseudoaneurysmal formation of the hepatic artery was evidenced. The arteriography was successfully performed by embolization with cyanoacrylate injection.
Conclusion: The case reported demonstrated that a pseudoaneurysm of the hepatic artery must be treated as early as possible because of the high risk of rupture and the associated high morbidity.
Keywords
Pseudoaneurysm; Hepatic trauma; Hepatic artery; Arteriography
Introduction
Hepatic artery pseudoaneurysm (HAP) is a rare but dangerous complication, and may be caused by acute or chronic damage to the hepatic artery. It occurs in about 1% of patients who experience blunt or penetrating abdominal trauma, normally in patients with associated liver damage [1].
Aneurysms of the visceral arteries are uncommon, but may be fatal due to its rupture. About 50% of the cases reported with hepatic artery aneurysms are pseudoaneurysms [2,1].
The location and frequency of artery aneurysms and pseudoaneurysms are primarily of splenic and its branches (45%-70% of cases), followed by hepatic (approximately 19%-20% of cases), renal artery (15%-25%) and celiac trunk (4%-5%) [3].
Normally, are devoid of endothelial lining on their walls. They are usually the result of direct tissue trauma or infection in the vascular wall. The pseudoaneurysm of the hepatic artery is a severe pulsatile hematoma caused by extravasation of the blood through rupture of the arterial wall. Early diagnosis and treatment lead to the best results.
Patients generally do not present with symptoms and the diagnosis is incidental [3]. However, although they are asymptomatic, they should always be treated in view of the high risk of complications, especially rupture. The current treatment of first choice is endovascular embolization.
The endovascular treatment of visceral pseudoaneurysms has been shown to be safe and effective in elective and urgent cases, presenting a high success and low rate of complication [3].
It's rupture may become fatal. Rapid identification and appropriate treatment is essential for patient survival.
Methodology
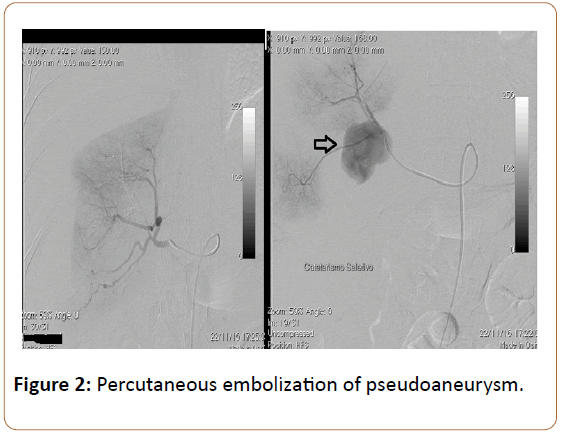
This study reports a case of a patient with post-traumatic hepatic artery pseudoaneurysm who was treated successfully by percutaneous embolization using cyanoacrylate injection.
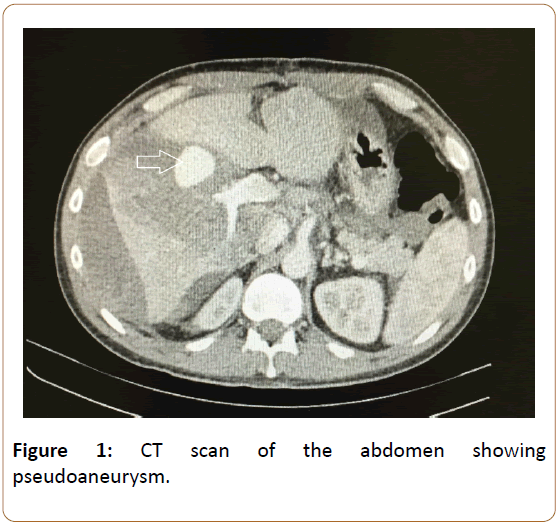
Report
A 34-year-old man was victim of blunt abdominal trauma due to an automobile accident. He was admitted to the emergency department, presenting severe abdominal pain and signs of peritonitis, US fast positive for fluid in abdominal cavity with hypovolemic shock, Laboratory showed hemoglobin=8 g/dL, hematocrit=31% and with blood pressure (BP) levels of 80/40 mm Hg. Exploratory laparotomy, which revealed a large amount of blood in the abdominal cavity, subcapsular hematoma and extensive hepatic laceration in segments V and VI, hemostatic suture with epiploplastia was performed. During the inicial post-operative period, the patient showed hematocrit decrease along with fever, signs of sepsis despite administration of large spectrum antibiotherapy with cefepime and metronidazol. Computed tomograph (CT) showed that the liver had a moderate volumetric increase, an irregular, non-singing hypodense image, measuring approximately 7.9 cm by 4.4 cm with gaseous foci in the middle, located predominantly in the segment V of the liver. The aspects were compatible with liver abscess. Then a second was performed on the after the inicial laparotomy, one liter and the presence of small collections of abscesses in the subphrenic region, but without active bleeding. The second post-operative period was uneventful, and the patient was discharged well on post-operative day. Fifteen days after discharge, the patient returns to the emergency department with tachycardia, fever, nausea and vomiting, "mild abdominal distension with persistent pain. Blood tests revealed leukocytosis 16000. The case was discussed at the clinical session and the intravenous empiric antibiotic therapy was initiated. An abdominal CT was performed that showed the presence of aneurysmal formation in the hepatic right hepatic artery topography, measuring 3.2 x 2.5 cm (pseudoaneurysm). In view of the finding, arteriography with hepatic artery catheterization was performed, and a pseudoaneurysm of the right hepatic artery was evidenced and embolized with cyanoacrylate injection, with success. The patient tolerated the procedure well with hospital discharge and without complications. At six months follow-up, he remains well (Figures 1 and 2).
Discussion
Hepatic artery pseudoaneurysm (PAH) is an uncommon as serious complication of acute or chronic liver injury of the hepatic artery. There are many causes of PAH, it But it is mainly caused by blunt, penetrating or iatrogenic abdominal trauma. Hepatic artery pseudoaneurysm may also occur in chronic pancreatitis due to the extension of a contiguous abscess or after hepatic transplantation [1]. The patient in the reported case was a victim of blunt abdominal trauma, developing hepatic abscess formation and, later, with PAH.
About 60% of PAHs are clinically quiet and found incidentally [4]. However, manifestations usually present with abdominal pain, associated with fever, hypovolemia and jaundice [5]. In the case reported, the patient presented all these symptoms.
PAH may present late clinical manifestations after abdominal trauma, including hemorrhage, abscesses, hemobilia and biliary peritonitis [5]. Although PAH can resolve spontaneously through thrombosis, there is a high risk of rupture, which is associated with a high mortality rate, requiring identification and early intervention [1].
The greatest complication of visceral aneurysms is rupture, which can occur in about 20% of cases of aneurysms and 70% of pseudoaneurysms. Such complications lead to an associated mortality rate varying from 25% to 100% [3]. Patients may present with upper or lower acute gastrointestinal bleeding, signs of an acute abdomen accompanied by jaundice or fever, or postoperative hemorrhage from an intra-abdominal drain [1].
Contrast abdominal (CT) is the complementary initial examination for diagnosis and follow-up of these patients, since it facilitates the evaluation of the hepatic parenchyma, in addition to monitoring the healing process. Ultrasonography may help distinguish PAH from a postoperative hematoma, but selective angiography remains the most sensitive test for detecting PAH [4]. Angiography may also show active bleeding and anatomical variations of the hepatic artery. Thus, some authors recommend an initial computed tomography if there is suspicion of PAH, followed by a reliable angiography [1].
HAP can be treated by exclusion, excision, revascularization or by endovascular therapy Endovascular treatment has high rates of successfull resolution with low morbi-mortality rates [6]. Open surgery has a mortality rate of 21%. In particular, endovascular embolization is the preferred treatment for intrahepatic aneurysms [2]. Considering that surgery is associated with significant morbidity and mortality, embolization has been shown to be safer and more effective, thus emerging as the primary treatment line and the most commonly used option.
In a multicentric retrospective series of patients with visceral aneurysms and pseudoaneurysms treated by endovascular intervention, twenty five patients were analyzed 19 patients with aneurysm and 5 with pseudoaneurysms. The treatment rate was considered successful, covering 96% (24/25) of the patients. The complication rate was 12% and the mortality rate was 0%.
The patient's embolization of this report was done with injection of Cyanoacrylate (N-Butyl 2-Cyanoacrylate), being an embolic material used in the blockade of visceral pseudoaneurysms. In a study of 14 visceral pseudoaneurysms treated with embolization, Cyanoacrylate showed that all patients recovered immediately after the embolization procedure. Cyanoacrylate allows fast and permanent embolization, with rapid polymerization when in contact with blood, being a safe, effective and low cost treatment method with a high success rate [7].
Despite its relative rarity, rapid identification and appropriate management of PAH may result in an excellent outcome with no associated mortality [8,9]. It is important to emphasize that in order to avoid high mortality associated with pseudoaneurysm, diagnosis and early treatment is important.
References
- Finley DS, Hinojosa MW, Paya M, Imagawa DK (2005) Hepatic artery pseudoaneurysm: A report of seven cases and a review of the literature. Surg Today 35: 543-547.
- Student KBD, Roushan N (2016) Hepatic artery pseudoaneurysm; simple or difficult to diagnose?. Arch Iran Med 19-521.
- Cappucci M, Zarco F, Orgera G, Lopez-Rueda A, Moreno J, et al. (2017) Endovascular treatment of aneurysms and pseudoaneurysms of visceral arteries using coated stenstents: Analysis of immediate and long-term results. Span Surg 95: 283-292.
- Soudack M, Epelman M, Gaitini D (2003) Spontaneous thrombosis of hepatic posttraumatic pseudoaneurysms: sonographic and computed tomographic features. J Ultrasound Med 22:99-103.
- Francisco LE, Asunción LC, Antonio CA, Ricardo RC, Manuel RP, et al. (2010) Post-traumatic hepatic artery pseudoaneurysm treated with endovascular embolization and thrombin injection. World J Hepatol 2:87-90.
- Loffroy R, Favelier S, Pottecher P, Genson PY, Estivalet L, et al. (2015) Endovascular management of visceral artery aneurysms: when to watch, when to intervene?. World J Radiol 7-143.
- Won Y, Lee SL, Kim Y, Ku YM (2015) Clinical efficacy of transcatheter embolization of visceral artery pseudoaneurysms using N-butyl cyanoacrylate (NBCA). Diagn Interv Imaging 96: 563-569.
- Marone EM, Mascia D, Kahlberg A, Brioschi C, Tshomba Y, et al. (2011) Is open repair still the gold standard in visceral artery aneurysm management?. Ann Vasc Surg 25: 936-946.
- Agha RA, Fowler AJ, Saeta A, Barai I, Rajmohan S, et al. (2016) The SCARE statement: Consensus-based surgical case report guidelines. Int J Surg 34: 180-186.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences