Recurrence Discussion in Varicose Veins Therapy-A Critical Examination of The Vein Stump Discussion
Ulf Th Zierau and Wolfgang Lahl
DOI10.21767/2573-4482.19.04.13
SAPHENION®-Surgeon, Berlin/Rostock, Germany
- *Corresponding Author:
- Zierau UT
Founder and CEO of SAPHENION®- Surgeon, Vascular Surgeon, Phlebologist, Endovascular Specialist Artery, Endogenous Specialist Berlin/Rostock, Germany
Tel: 0491708302447
E-mail: dr.zierau@yahoo.de
Received date: May 10, 2019; Accepted date: May 24, 2019; Published date: May 31, 2019
Citation: Zierau UT, Lahl W. Recurrence Discussion in Varicose Veins Therapy-A Critical Examination of The Vein Stump Discussion. J Vasc Endovasc Therapy 2019, Vol.4 No.2:13.
Abstract
The recurrence discussion in varicose veins is mainly led to a tendentious venous stump discussion. Radical stripping vs. endovenous laser as a vehicle for the fundamental scientific, turning away from the endovenous procedures, in the treatment of varicose disease. This is no new phenomenon, it`s nearly as old as the different therapy options himself. Since 1911 we have seen the discussion between the radical surgery fraction and the endovenous fraction.
Keywords
Long vein stump; Recurrence rate laser vs. radical stripping; Recurrence rate endovenous techniques; Manufacturer's recommendation long stump
Introduction
The recurrence discussion in varicose veins is very intensive and controversal. On one side the collegues with experiences in 20 years of catheter based endovenous ablation, on the other side collegues without any experience in these techniques. Here we find insistence on radical therapy techniques. This is all the more surprising since Ferdinand Sauerbruch in 1929 considered radical vein surgery to be no longer up-to-date.
Saphenion would like to discuss the scientific work of Prof. Achim Mumme, Head of Vascular Surgery at the Catholic Hospital Bochum in the journal "Phlebologie" [1]. Meanwhile, he declared in TV the "stripping" to gold standard again [2]!
Another reason is the current review in a district Court procedure in Neubrandenburg for the reimbursement of costs for endovenous procedures on the venous system. The expert, Prof. Ernst Klar, Head of University Surgery Hospital Rostock, largely accepts the arguments of Prof. Mumme.
Long venous stump after catheter therapycause of higher recurrence rate?
Prof. Mumme writes: “In the case of endovenous procedures for the treatment of truncal venous insufficiency, the principle of crossectomy (lateral branch obstruction in the inguinal region, in the foreground) is dispensed with and almost always a vein stump remains (long stump of the saphenous vein, author) , crossectomy is an indispensable part of the treatment concept in surgical treatment, however, and leaving a truncal vein stump is considered a treatment error, which favors the development of recurrent varicose veins. In the field of GSV-junction there is therefore currently no uniform treatment principle“.
What is considered as therapy recommendation in one procedure (endovenous procedure) is a treatment error in the other procedure!
Against this background, long-term results of the competing procedures are relevant. In particular, the question must be clarified whether the departure from the principle of crossectomy actually has no effect on the recurrence rate.
A literature search looked for prospective randomized trials with a follow-up period of at least 5 years in which endovenous laser procedures were compared with the crossectomy and stripping operation and in which the duplex sonographic detection of vein junction was performed. The duplex sonographic junction recurrence is considered a surrogate parameter for the later occurring clinical junction recidive. Laser therapy (EVLA) was studied in 6 randomized trials and radio wave therapy in one study. In favor of a better homogeneity of the comparison groups, the only radiowave study was excluded, so that only laser studies were included.
In none of the studies was the rate of duplex sonographic recurrence after laser lower than after crossectomy and stripping. In one study, the recurrence rates were the same and 5 studies showed an advantage for the surgery. In these studies, the rate of duplex sonographic recurrence after laser was 1.7-5.6 times higher than after surgery.
The data from the medium-term follow-up studies indicate that the departure from the principle of radical surgical crossectomy, at least in the case of the laser, is at the expense of a higher rate of recurrence. In view of the great socio-medical significance of the recurrence of the disease, these figures are alarming, since high follow-up costs for the treatment of recurrences must be expected. Whether the principle of crossectomy can also be implemented endovenously is questionable.
However, to what extent the principle of crossectomy can be understood in an endovenous way is still unclear. There is no evidence that an endovenous occlusion of the crosse at the level of the deep vein also persists in the long term.
In addition, it is unclear whether the heat ablation directly at the deep vein leads to consequential damage such as thromboembolism, scarred stenosis (constriction d.A,) or damage to the lymphatic tissue.
Other problems exist in medical terms. Finally, in the application notes of various methods, the heat ablation of the proximal 1-2 cm of the trunk vein is expressly prohibited.
Until these issues have been resolved, heat ablation directly on the deep vein should only be done within ethically verified studies. High recurrence rates of laser therapy confirm the necessity of the crossectomy.
The high recurrence rates of laser therapy are alarming and, in retrospect, raise the question as to whether the paradigm shift made with the introduction of heat ablation methods was justified. The negative effects of the saphenous stump known from operative therapy with regard to the development of recurrences apparently also apply if the stump is the result of an endovenous treatment. Demensprechend must be considered as a consequence of the endovenous therapy that no Crossenstumpf with morbidly altered V. saphena magna may be left behind. Finally, this acceptance of the principle of crossectomy would also end the paradox that has existed for years, that on the one hand (endovenous therapy) is permitted, which on the other hand (surgery) is regarded as a treatment error and is therefore prohibited. In fact, so far two (!) Randomized studies have confirmed the positive effect of a combination of EVLA and crossectomy. In combination with surgical cystectomy, laser therapy has similar cervical reflux rates as the crossectomy and stripping operation.
Much of the operations carried out in Germany are aimed at eliminating crossbones. According to data published by Noppeney in 2005, of a Germany-wide quality assurance register, the proportion of operations on relapse was about 15%. In specialized centers, the proportion of re-crossectomies is even higher. In the infirmary of Frings et al. their share was 24%. Accordingly, the socio-economic importance of the Crossezidive is high. Already in the year 2000, the costs in Germany amounted to approx. €64 million. At the time, it was still all about "surgical recurrences". At present, however, we are seeing an increasing substitution of varicose veins surgery with endovenous procedures.
This development should lead to considerable socio-medical effects. In view of the higher rates of recurrence of laser ablation in Germany by factor 4 or 5.6, follow-up costs at the astronomical level threaten the later elimination of stomp veins. Extrapolated from the figures from the year 2000, these cheat about € 256 million to € 358.4 million per year if only lasers were used instead of the radical surgical operation. Such extrapolations are certainly fraught with great uncertainties.
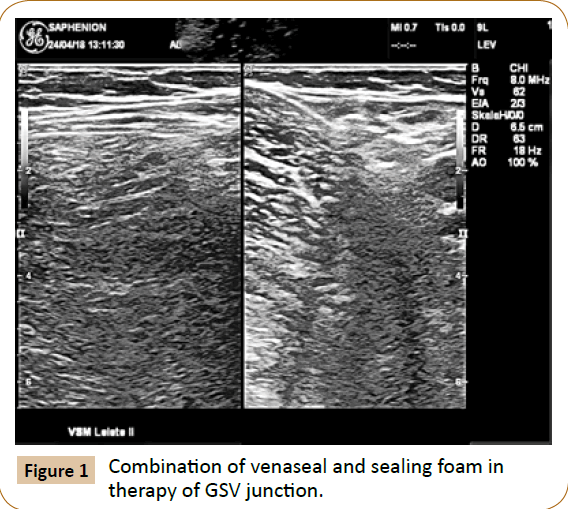
Nevertheless, they illustrate the burdens that would be expected if the relapse-poor operation were substituted by endovenous methods [3] (Figures 1 and 2).
Our thoughts and experiences to the topics
Basically, we agree with Prof. Mumme. The effective treatment of the vein junction is not just since today sine qua non. We too have learned the Crossectomy in the appropriate clinics and universities and carried out many thousands of stripping operations in the hospital and then in our own practice [4-7]. At Saphenion, crossectomy is still considered necessary. However, crossectomy is also endovenous very well - if not better - feasible.
We have an ultrasound device intraoperatively and can show all lateral veins in the inguinal region during the catheter procedure.
In the endovenous procedures radio wave and vein glue, as well as in the microfoam, the principle of crossectomy is not dispensed with. All the colleagues we know, whether traveling with the new laser devices, working with the radio wave catheter or, as we do, with the venous adhesive, push the catheter as far as possible (about 1 cm from junction) and then start the therapy. So it comes with the thermal process to the boiling of the vein wall to the confluence, as well as the glue for sealing to the sealing of vein junction. This requires-of course-the experience of about 150 interventions (s. a. my presentation at the "hot iron Heidelberg 2017"). Then the modification of the therapy can be started. To what extent the laser operating at very high temperatures sets injuries to the deep venous system or to the lymphatic or nervous system in the case of estrogen-related therapy, we can not judge. We left the laser in 2008 and then switched to the radio wave catheter before working with the vein glue in 2012 [8-14].
Even with endovenous therapy, it is not true that a long stump is accepted. Again, the junction is treated, either with microfoam or with a renewed catheter maneuver [15-18].
Unfortunately, Prof. Mumme only compared the laser process with stripping for his work. The 6 studies chosen by Prof. Mumme are also no longer up-to-date. For 3 years, long - term results from the radio wave or VenaSeal catheter have been available [19-25]. Bearing in mind that the radio wave catheter has a higher closure efficiency than the laser and the glue once again more effective than radio wave, the statements on the topic are only very limited to discuss.
As already mentioned, the current study literature on long-term results of the radio wave and the VenaSeal vein glue was not spotted by Prof. Mumme at all. In this respect, the statement prohibits, endovenous procedures produce faster and more recurrences. The results speak a completely different language [26,27].
The indication of an almost 6 times higher recurrence rate in the laser compared to the radical stripping op is in itself clearly polemical and tendentious, as Prof. Mumme considers only the laser (which laser at all, linear or radial laser?) isolated [7].
We agree with Prof. Mumme - recurrences are not beautiful and must always be treated. But we also see stripping in up to 60% depending on the study. In our vein center many relapses come after stripping surgery. But here is also cited Van Dongen: "... you always have to educate the patient that the varicose veins are a chronic process and we can not really stop the new development ...." [3]. By the way, after radiowave or vein glue therapy, we have seen significantly fewer recurrences for nearly 7 years in the follow-up [8,15,16].
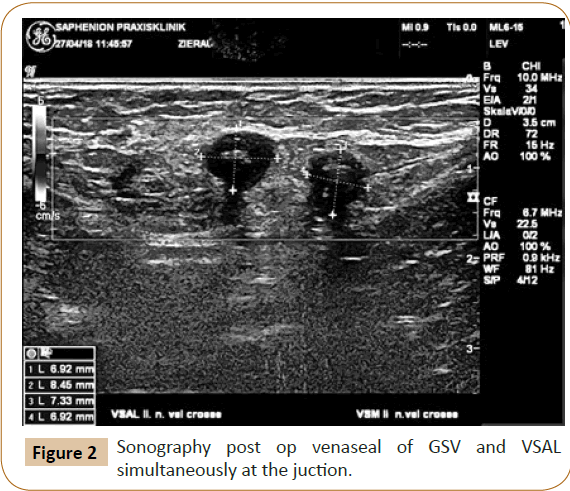
The proof of a long-term closure of the vein glue is provided by regular duplex sonographic follow-up checks. We have seen a closure rate of 96.4% over 81 months [15,18,25,27].
Prof. Mumme is right here! That was a reason for us to stop using the Linearlaser from 2008 onwards. Also we have seen nerve and lymphatic damage [7].
We are also aware that manufacturers of various endovenous technologies always point out that they are about 5 cm away from the crosse. This also applies to the vein glue [17]. However all procedures are clearly modifiable after appropriate experience. And you clarify in any case, the patient on the therapy process. Normally, our patients almost always ask whether the catheter is in the pelvic vein or the vein glue flows into the pelvic vein-so they understood the problem [15,27].
In the laser we agree with Prof. Mumme. But we would also like to hear current users of the laser system. And perhaps the collegue of Prof. Mumme in Bochum, Prof. Stücker, now head of the venous center at the Catholic Hospital Bochum, to report on his own experience with laser and radio wave [7,20,21].
We also agree completely with Prof Mumme here. Crossectomy must also be used in endovenous procedures. And as described above, this is done by most of us colleagues known in various ways. However, the high recurrence rates only in the (older) laser studies are really not the reason to want to demonize all endovenous procedures for massive cost increases in the future. Conversely, a shoe is sewn: a clear definition for all endovenous procedures and exclusively outpatient therapy (because stationary much more expensive [22].
Here we can not agree - we do not see higher recurrence rates, we see recurrences especially after radical surgery. Now you could say that this surgery was wrong. But that's not ours and we will not do colleague bashing. But the warning of rising costs for recurrence treatment through the large-scale introduction of all endovenous procedures is biased and not substantiated by factual evidence [7-10,20-22].
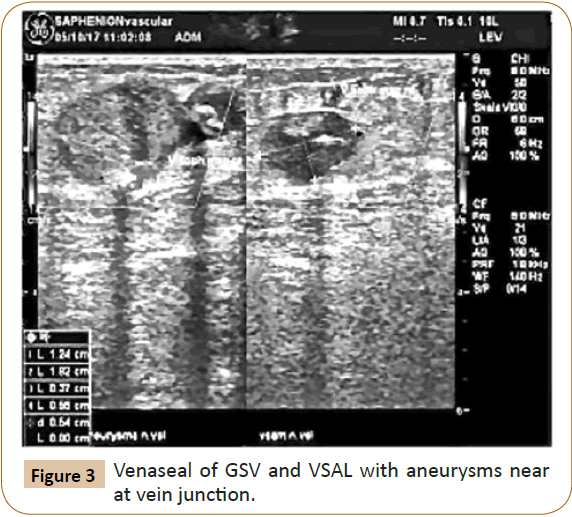
As already written by Prof. Mumme, to speak of astronomically rising costs related to the high recurrence rate of endovenous therapy is unsure. So again tendentious in this context [7,22] (Figure 3).
This is all the more true for the final conclusion: Stripping as a relapse-poor compared to radio wave and vein glue is a complete lack of awareness of the current study situation and the daily clinical experience in the specialist practices [8-10,17-27].
Conclusion
We have to start again in Germany with the radical "stripping" after Sauerbruch 1929 had put this procedure to the record. Around Germany, people are working diligently with endovenous techniques. Whether in Poland, in the Baltic Republics or in Russia! and even better, you also know the numbers: In Germany, 65-70% of all patients are treated by radical stripping, in the US more than 90% of patients are treated with endovenous catheters.
We don`t think, that 6 older studies about laser ablation vs. stripping give the right to ignore all the new endovenous techniques. We have a lot of studies about radio wave and also about VenaSeal. Also, the microfoam shows good experiences in the therapy of truncal varicose veins, if we take care in some general points (diameter of veins, length of veins).
And the author has forgotten the better results of radio wave and the VenaSeal. But all users of these techniques have to ablate also the junction. This is to make very good with the catheter system alone or in combination with microfoam or Sealing Foam. Just as we can no longer build airports and subways in Germany, so we are going back to the "stripping" by the American surgeon Babcock first described in 1906/1907.
And who thinks about the pain of the patient? Who thinks about the Quality of life (QoL-Index) after radical surgery?
Conflict of Interest
I do not have any potential conflict of interest.
References
- Flessenkämper I, Hartmann M, Hartmann K, Stenger D, Roll S (2016) Endovenous laser ablation with and without high ligation compared to high ligation and stripping for treatment of great saphenous varicose veins: Results of a multicentre randomised controlled trial with up to 6 years follow-up. Phlebology 31: 23-33.
- Hamann SA, Giang J, De Maeseneer MG, Nijsten TE, van den Bos RR (2017) Editor's choice-five year results of great saphenous vein treatment: A meta-analysis. Eur J Vasc Endovasc Surg 54: 760-770.
- Heberer G, Van Dongen RJ. (1989) Vascular surgery. Springer, USA.
- Hübner K, Blazek V, Breu FX. (2008) Praktische sklerotherapie. ViaVital-Verlag Essen, Germany. pp: 71-75.
- Jones WS, Vemulapalli S, Parikh KS, Coeytaux RR, Crowley MJ, et al. (2017) Treatment strategies for patients with Lower Extremity Chronic Venous Disease (LECVD). Technology Assesment Report.
- Kalteis M, Adelsgruber P, Messie-Werndl S, Gangl O, Berger I (2015) Five-year results of a randomized controlled trial comparing high ligation combined with endovenous laser ablation and stripping of the great saphenous vein. Dermatol Surg 41: 579-586.
- Mumme A, Mühlberger D, Sidhwa Y, Hummel T (2019). Alarming high rate of saphenofemoral recurrences after endovenous laser therapy. Phlebology 48: 18-22.
- Wittens CDAH, Davies AH, Bækgaard N, Broholm R, Cavezzi A, et al. (2015) Editor's choice-management of chronic venous disease: clinical practice guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 49: 678-737.
- Kheirelseid EA, Crowe G, Sehgal R, Liakopoulos D, Bela H, et al. (2018) Systematic review and meta-analysis of randomized controlled trials evaluating long-term outcomes of endovenous management of lower extremity varicose veins. J Vasc Surg Venous Lymphat Disord 6: 256-270.
- Lawaetz M, Serup J, Lawaetz B, Bjoern L, Blemings A, et al. (2017) Comparison of endovenous ablation techniques, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Extended 5-year follow-up of a RCT. Int Angiol 36: 281-288.
- Kremer K, Schumpelick V, Hierholzer G (1992) Chirurgische operationen-atlas für die Praxis. New York. pp: 682-685.
- Weber J, May R (1990) Funktionelle phlebologie; Georg thieme verlag stuttgart. New York. pp: 531-543.
- https://www.thieme-connect.de/products/ejournals/html/10.1055/a-0798-6120
- https://vascular-endovascular-therapy.imedpub.com/the-fate-of-saphenaviews-into-the-past.php?aid=23856
- https://vascular-endovascular-therapy.imedpub.com/venasealsupregsup-closure-results-over-6-years-treatment-a-followup-study-conducted-on-1950-truncal-saphenous-veins-in-1061-cases.php?aid=23546
- https://vascular-endovascular-therapy.imedpub.com/sealing-veins-vs-radiofrequency-ablation-oftruncal-varicose-veins5-years-experience.pdf
- https://www.massdevice.com/medtronic-touts-five-year-venaseal-study-data/
- https://vascularnews.com/veclose-venaseal-safe/
- Lawson JA, Toonder IM (2016) A review of a new Dutch guideline for management of recurrent varicose veins. Phlebology 31: 114-124.
- Djalali S, Mikulicic F, Berwarth H, Rosemann T, Rosemann A (2012) Will foam sclerotherapy and endovenous thermal ablation replace varicose vein stripping? Praxis 101: 1297-1307.
- Paravastu SC, Horne M, Dodd PDF (2016) Endovenous ablation therapy (laser or radiofrequency) or foam sclerotherapy versus conventional surgical repair for short saphenous varicose veins. Cochrane Database Syst Rev 2016: CD010878.
- Carroll C, Hummel S, Leaviss J, Ren S, Stevens JW, et al. (2013) Clinical effectiveness and cost-effectiveness of minimally invasive techniques to manage varicose veins: a systematic review and economic evaluation. Health Technol Assess 17: 136-141.
- Noppeney T, Rewerk S, Winkler M, Nüllen H, Schmedt HC (2007) Primary varicosis. Chirurg 78: 620-629.
- Gibson K, Morrison N, Kolluri R, Vasquez M, Weiss R, et al. (2018) Twenty-four month results from a randomized trial of cyanoacrylate closure versus radiofrequency ablation for the treatment of incompetent great saphenous veins. J Vasc Surg Venous Lymphat Disord 6: 606-613.
- Balint R, Farics A, Parti K, Vizsy L, Batorfi J, et al. (2016) Which endovenous ablation method does offer a better long-term technical success in the treatment of the incompetent great saphenous vein? Review. Vascular 24: 649-657.
- https://www.saphenion.de/news/vein-glue-on-2263-varicose-veins-81-months-application/
- https://www.youtube.com/watch?v=0z25AKuH_xw
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences