Single Coronary Artery as a Possible Source of Myocardial Ischemia
Ivo S Petrov1, Zoran J Stankov1, Naidenka I Zlatareva-Gronkova1 , J ivka D Stoykova1, V iktoria S Dimitrova1, Latchezar D Penev1, Krassimira A Dulgerova 1 , Blagovest S Stoimenov 2, Dimitar M Dimitrov3 , Diana Trendafilova 3 and Тodor Kundurdjiev4
1Department of Cardiology, Medical Faculty of Sofia University, ACIBADEM City Clinic, Sofia, Bulgaria
2Department of Cardiology, Alexandrovska University Hospital, Sofia, Bulgaria
3Department of Cardiology, Saint Ekaterina University Hospital, Sofia, Bulgaria
4Department of Cardiology, Medical University, Sofia, Bulgaria
- *Corresponding Author:
- Viktoria Sasheva Dimitrova
Department of Cardiology,
Medical Faculty of Sofia University,
ACIBADEM City Clinic, Sofia,
Bulgaria,
E-mail: viktoria_raeva@abv.bg
Received date: August 26, 2022, Manuscript No. IPJVES-22-14399; Editor assigned date: August 29, 2022, PreQC No. IPJVES-22-14399 (PQ); Reviewed date: September 09, 2022, QC No. IPJVES-22-14399; Revised date: September 19, 2022, Manuscript No. IPJVES-22-14399 (R); Published date: September 26, 2022, DOI: 10.36648/2471-9943.7.8.4604.
Citation: Petrov IS, Stankov ZJ, Zlatareva-Gronkova NI, Stoykova JD, Dimitrova VS, et al.(2022) Single Coronary Artery as a Possible Source of Myocardial Ischemia. J Vasc Endovasc Therapy Vol.7 No.8: 4604.
Abstract
Context: A Single Coronary Artery (SCA) is а rare congenital disorder. Its clinical presentation varies from asymptomatic to serious ischemic evidence, usually diagnosed by coronary angiography or post-mortem.
Case series: We aim to explain frequency, variety of clinical presentation, related to anatomical variants of the SCA, and to propose an evidence based diagnostic and treatment algorithm. For a 5 year-period among 11,597 consecutive selective coronary angiographies we detected 10 individuals (0.9‰) with a SCA. Acute Coronary Syndrome (ACS) was the most common clinical presentation in the study group, followed by palpitations and stable angina pectoris. Atrial fibrillation and reduced LV systolic function were often evident in the study group. The origin of SCA of the right coronary sinus was more often related to ACS. The origin of SCA of the left coronary sinus was accompanied by rhythm disorders and moderately reduced LV systolic function.
Conclusion: Clinical manifestation, anatomical course, and atherosclerotic involvement of SCA guided the choice of therapeutic strategy, including the method for myocardial revascularization.
Keywords
Single coronary artery; Myocardial ischemia; Left ventricle dysfunction; Atrial fibrillation; Revascularization
Introduction
The term Single Coronary Artery (SCA) is used to describe specific Coronary Artery Anomaly (CAA) in which only one coronary artery is arising from the aorta by a single coronary ostium and providing perfusion for the entire myocardium [1-3]. The prevalence of SCA is ranged between 0.024% [1] and 0.066% [2] in the population who undergo Coronary Angiography (CA).
In most cases SCA is asymptomatic, but in some patients may lead to symptoms, including angina pectoris, Myocardial Infarction (MI), congestive Heart Failure (HF), syncope, lifethreatening cardiac arrhythmias, or Sudden Cardiac Death (SCD) [4]. As soon as SCA anatomy is evident, further examination for myocardial ischemia is obligatory. In most cases, a pathologic course of SCA could cause a decrease in blood flow delivery to the underlying myocardium, independently of atherosclerotic stenoses evident or not.
According to the site of origin and anatomical distribution of the branches, Lipton et al. [1] proposed a very pragmatic angiographic classification. Based on it, the primary division was made between the ‘R’ right-type and ‘L’ left-type according to the coronary sinus of origin of SCA. Furthermore, each case is subdivided as belonging to group I, II, or III according to the anatomical course of the artery, in type ‘I’ SCA follows the normal course both of the right and the left coronary artery. Type ‘II’ SCA, after leaving the right or the left coronary sinus to provide the contralateral coronary artery, crosses the base of the heart by a wide range of transverse connecting vessel. Type ‘III’ SCA, after leaving the right coronary sinus of valsalva gives Left Anterior Descending (LAD) and Left Circumflex Arteries (LCx) arising separately from the proximal part of the vessel. Finally, SCAs are classified according to their relation to the aorta and pulmonary artery, ‘A’ the left main passes anterior to the pulmonary artery, ‘B’ the left main passes between the aorta and pulmonary artery, ‘P’ the left main passes posterior to the aorta. Yamanaka et al. [3] have added to this classification the ‘S’ septal, indicating interarterial connection through the interventricular septum/ and ‘C’ indicating combined type [5]. In this series, the “septal” subtype was the most common, whereas the “between” subtype was the least common [6].
More recently, Angelini et al. [4] proposed a classification of CAAs according to the anatomical course within the interventricular and atrioventricular grooves, as well as the location of the penetrating side branches. Angiography is often sufficient to define CAAs, however, Coronary Computed Tomography Angiography (CCTA) and Magnetic Resonance Angiography (MRA) are useful to confirm and describe them in detail [7]. Coronary revascularization is recommended when there is significant and documented ischemia [5]. In patients with CAAs, the causes of ischemia can be multifactorial including atherosclerosis, slit-like ostium, ostial ridge, acute-angle take-off, coronary spasm, an interarterial course with associated hypoplasia, and an intramural course /at the aortic wall/ with lateral compression or exercise-related narrowing [6]. The scissors-like mechanism could explain the ischemia related SCD, due to a course of SCA between the aorta and main pulmonary artery [7-14]. A simplified modification of angelini and Khatami’s classification [10] is currently used in clinical practice. It divides CAAs into two groups: Group A, anomalies of origin and distribution; and Group B, intracoronary communications and coronary artery fistulae [9,10]. All presented cases correspond to group (b) of Angelini classification and simplified version of CAAs [10] – group A. Angelini et al. [11] proposed that a common proximal trunk, which joins 2 or 3 coronary arteries, should be named a mixed trunk. The only normally observed mixed trunk is the left main (common trunk, or stem) [11,12].
Methods
Study population
For a five year-period and based on clinical and instrumental indications, we performed selective CA of 11,597 patients, of which we detected the patients with SCA. The evaluation of the patients was performed by cardio logical exam, ECG, TTE, CA, ECG- and scintigraphy stress tests, CCTA. The results of the instrumental findings were discussed in “heart team” meetings.
CCTA evaluation
The CT scans were performed by ECG gated acquisition on 128-slice CT scanners (Philips Ingenuity TM, Netherlands). In order to obtain maximum image quality a sublingual nitroglycerin spray in all patients and intravenous beta-blocker were administered to achieve the intraprocedural target heart rate (<65/min) in selected patients, when contraindications were absent. The CT scans were analyzed by a team of radiologist and a cardiologist.
Statistical analysis
Statistical analyses were performed using statistical software SPSS for Windows version 20.0. Continuous variables were presented as mean and Standard Deviation (SD). The category variables were presented as a number and percentage with 95% confidence interval.
Results
Between 2016 and 2021 in 11,597 consecutive patients we discovered ten cases of a SCA, which corresponds to frequency of this anomaly of 0.9‰ (9:10000). Mean age of the SCA patients was 67.10 (SD=10.72), five males. Acute Coronary Syndrome (ACS) was the most common (5 patients) clinical presentation in the studied group, followed by palpitations (3 patients, or 30.0%, 95% Cl, 6.7-65.3) and stable angina pectoris (2 patients, or 20.0 %, 95% Cl , 2.5–55.6 ). Rhythm disturbances found by ECG recordings (7 patient, or 70.0%, 95% Cl, 34.8– 93.3), included supraventricular arrhythmias-Atrial Fibrillation (AF) (4 patient, or 40.0%, 95% Cl, 12.2–73.7), one with atrial flutter and one patient with sinus tachycardia (10.0%, 95% Cl, 0.3–44.5). ECG signs of myocardial ischemia were evident in 50% of the patients (95% Cl, 18.7–81.3). In this small group a prevalence of the infero and infero-lateral wall of Left Ventricle (LV) wall motion disturbances was evident (4 patients) on Transthoracic Echocardiography (TTE). In eight patients we observed reduced LV systolic, as 5 of them had moderate and three-mild reduction. The CA established an origin of SCA from the right coronary sinus in 7 patients, and from the left – in 3 patients. In 4 out of 5 patients presenting with ACS we detected an origin of SCA from the right sinus of Valsalva. One patient was referred for OMT alone after rejection of a flow-limiting stenosis. Five of six patients with angiographically significant Coronary Artery Disease (CAD) were treated by PCI, as the sixth one declined any further intervention. One patient was indicated for cardiovascular surgery of valves pathology. We discovered two clinical cases with associated inherited cardiovascular disease: One with noncompaction cardiomyopathy, indicated for ICD implantation, and one with bicuspid aortic valve, referred for Transcatheter Aortic Valve Implantation (TAVI). On six- and twelve-months follow-up no clinical events were detected Table 1.
| Clinical case | Sex (m/f) | Age (n) | Clinical presentation | Electrocardiographic findings | Transthoracic echocardiography / LVEF (%) | Stenosis evidence and localization | Treatment/ Recommendation | Lipton classification |
|---|---|---|---|---|---|---|---|---|
| 1 | f | 70 | Stable angina | AF, left anterior fascicular block, ST-depression and negative T-waves in anteroseptal precordial leads | moderate reduction | Non-significant stenosis in distal RCA /FFR-guided evaluation/ | OMT | L - I |
| 2 | f | 81 | ACS | AF, right BBB | moderate reduction | bifurcation stenosis of distal LAD segment and the septal branch | PCI + OMT | L - II |
| 3 | m | 67 | ACS | Infero-lateral ischemia | moderate reduction | hypoplastic and significantly stenotic LAD and LCx, intact DES in RCA without in-stent restenosis | PCI + OMT | R - II |
| 4 | f | 78 | Palpitations | Atrial tachycardia, left BBB | moderate reduction | no | OMT + surgical treatment | L- II |
| 5 | m | 68 | ACS | sinus tachycardia, inferior ischemia | moderate reduction | thrombotic occlusion of distal segment of RCA | PCI + OMT | R-III |
| 6 | m | 44 | Palpitations | AF | mild reduction | no | OMT + ICD | R-III |
| 7 | f | 60 | Stable angina | AF | preserved | severe ostial stenosis of the anomalous branch | PCI + OMT | R-II |
| 8 | m | 66 | ACS | Infero-lateral ischemia | mild reduction | native proximal dissection of RCA and 50% stenosis before bifurcation of PL and PD | PCI + OMT | R - I |
| 9 | f | 61 | ACS | Inferior ischemia | preserved | Subtotal ostial stenosis of RCA in SCA pattern | PCI + OMT | R - III |
Table 1: Clinical characteristics, diagnostic and treatment methods of different clinical cases.
ACS–Acute Coronary Syndrome; AF-Atrial Fibrillation; BBBBundle Branch Block; ICD-Implantable Cardioverter Defibrillator; LAD–Left Anterior Descending Artery; LCx – Left Circumflex Artery; OMT-OPTIMAL MEDICAL THERAPY; PCI–Percutaneous Coronary Intervention; RCA–Right Coronary Artery, SCA-Single Coronary Artery; TAVI-Transcatheter Aortic Valve Implantation.
The Cases
Case 1
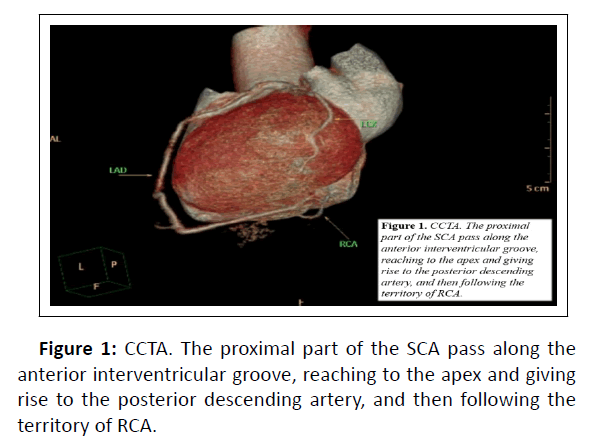
A 70-years-old female patient with a new onset of retrosternal chest pain with left scapular propagation, on new oral anticoagulant therapy in the last one year for paroxysmal AF. At admission, she presented with stable angina III CCS class, sinus rhythm, left anterior Fascicular Block (FB), ST-depression, and negative T-waves in anteroseptal precordial leads (V1-V4) on ECG. TTE found a moderate reduction in Left Ventricle Ejection Fraction (LVEF) with diffuse hypo kinesis. The blood lipid levels which were extremely elevated. We performed CA and found SCA originating from the left coronary sinus, with anterior course reaching the apex, then turning to the inferior heart surface. The ostium of RCA was not found. CCTA confirmed figure 1 that the ostial part of the vessel originates from the left coronary sinus and passes above the interventricular septum and bifurcates in two branches: LAD and LCx. The LAD passed along the anterior interventricular groove, reaching the apex and giving rise to the posterior descending artery, and then following the territory of RCA with natural anatomical course. By Lipton classification [1] this case was type L-I-A. There were no significant coronary artery stenosis, but moderate LV systolic dysfunction was observed. Total calcium score /Agatson/ was 1.01, which corresponds to a mildly increased risk of cardiovascular events. Seeing a contraindication for a treadmill stress-test, we recommended stress-test myocardial perfusion scintigraphy to precise the ischemia burden and treatment strategy like recommended in the presence of coronary Artery from the Opposite Sinus (ACAOS) and other potentially significant CAAs [13]. Myocardial single-photon emission CT showed borderline significant hypoperfusion of myocardial region supplied by RCA. The next diagnostic step was to examine the fractional flow reserve of distal RCA and the result was nonflow- limiting stenosis (FFR–0.83) and there was no intervention indicated.
Case 2
An 81-year-old female patient with chest discomfort and palpitations. Age, arterial hypertension, and dyslipidemia were the risk factors for CAD, on oral anticoagulant and rate control therapy for permanent AF. Physical examination demonstrated irregular pulse, tachycardia, and normal arterial pressure. The ECG showed AF and right Bundle Branch Block (BBB). TTE revealed moderate LV systolic dysfunction (LVEF-45%), moderate aortic and mitral regurgitation, and left atrium enlargement (PLAX-view: 47 mm). CA was relevant with SCA originating from the left sinus of Valsalva. RCA was originating from the LAD just after the bifurcation of the left main. This case was Lipton type L-II [1]. From the proximal part of LAD, a big septal branch was present. Critical bifurcation stenosis of the distal LAD segment and the septal branch (Medina 0:1:1) was sequentially and successfully treated with DES implantation, following the provisional T strategy with final kissing and proximal optimization technique. The patient was discharged on OMT, including short (for 1 month) triple antithrombotic therapy– aspirin 100 mg qd, clopidogrel 75 mg qd and Vitamin K Antagonist (VKA), followed by clopidogrel and VKA. Uneventful follow-up was demonstrated for 12 months.
Case 3
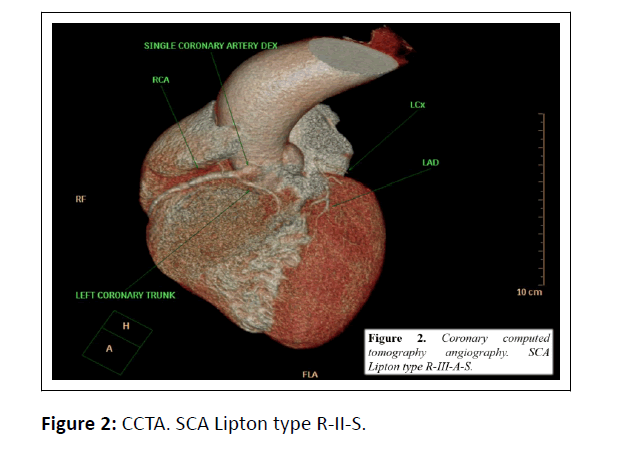
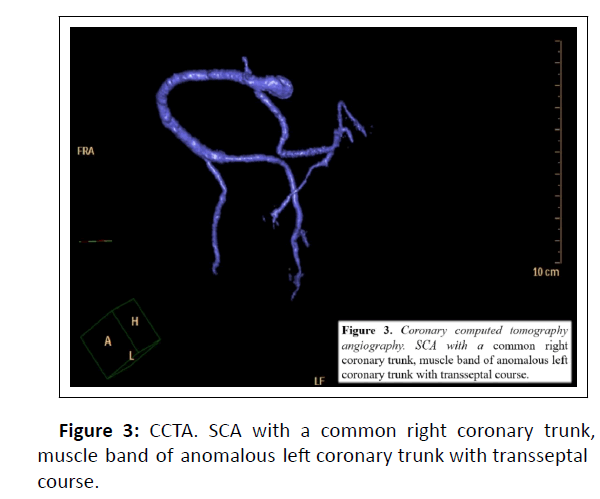
The third case refers to 67-years old male patient who presented with an angina equivalent. Risk factors for CAD were age, gender, arterial hypertension, dyslipidemia and smoking. The patient was with known multivessel CAD, and old inferior STEMI, after PCI and DES implantation of the RCA. The patient’s medical treatment included dual antiplatelet therapy, an ACE inhibitor, and statin. Left cardiac axis deviation and normal repolarization were presented on the ECG. The laboratory tests for myocardial necrosis were negative. TTE showed moderately reduced LV function with intact segmental kinetics. Clinical pretest probability for myocardial ischemia was 84%, so the patient was referred for non- invasive imaging. CCTA figure 2,3 revealed SCA arising from the right coronary sinus, muscle band of the anomalous left coronary trunk with the transseptal course, hypoplastic and significant stenotic LAD and LCx, patent DES in RCA without in-stent restenosis. SCA after arising from the right coronary sinus of valsalva bifurcated separately in LAD and LCx. The left was situated anterior to the pulmonary artery through the interventricular septum. This case was Lipton type [1] R-II-S. Left cardiac ventriculography confirmed moderately reduced LVEF, 41%. Total calcium score /Agatson/ was 296, which suggested the presence of atherosclerotic plaque and moderate risk of cardiovascular events. The patient was referred for urgent revascularization, but he refused both cardiac surgery and endovascular treatment.
Case 4
78-year-old female patient with palpitations and dyspnea at rest, with medical history of arterial hypertension and HF. She had interrupted her anticoagulation and antiarrhythmic therapy months before admission. The ECG showed atrial tachycardia and left BBB. Laboratory testing showed anemia. TTE revealed moderate LV systolic dysfunction, LVEF-42%, dilated LV chamber, dyskinesia of basal and middle septum, akinesia of apical segment, mild LV hypertrophy, severe aortic and mitral regurgitation, left atrium enlargement /PLAX view: 56 mm/ and severe pulmonary hypertension. CA showed SCA with right coronary system originating from the left main with no significant stenosis of the epicardial vessels. Left ventriculography demonstrated moderate LV systolic dysfunction, LVEF-43% and severe mitral regurgitation. This case was similar to our second case and was classified as Lipton type L-II [1]. The patient was indicated for mitral and aortic valve replacement, discharged on OMT, and referred to the Department of Cardiovascular surgery.
Case 5
A 68 years-old male patient presented with accelerating angina and dyspnoea with onset two hours before the admission. The ECG showed sinus tachycardia and inferior wall STEMI. The TTE revealed hypokinesia of inferior LV wall and significantly reduced LVEF of 38% and moderate mitral regurgitation. Thoracic X-ray confirmed signs of interstitial pulmonary congestion. Laboratory tests were positive for myocardial necrosis and dyslipidemia. CA demonstrated an SCA, originating from the right aortic sinus and acute thrombotic subocclusion of the distal RCA proximal to the PD-PL bifurcation. The left coronary system originated from the proximal part of RCA. Immediate PCI of RCA was performed. After balloon predilatation and DES implantation normal epicardial perfusion was restored in the culprit RCA. Contrast injection in the left coronary sinus proved the absence of coronary artery, arising from the left sinus of Valsalva. An observational aortography in anteroposterior position was performed which found out that LAD has a retro-aortic course and continues in the interventricular groove. The SCA class Lipton type [1] R-III. The patient was discharged on the fourth post procedural day without further events.
Case 6
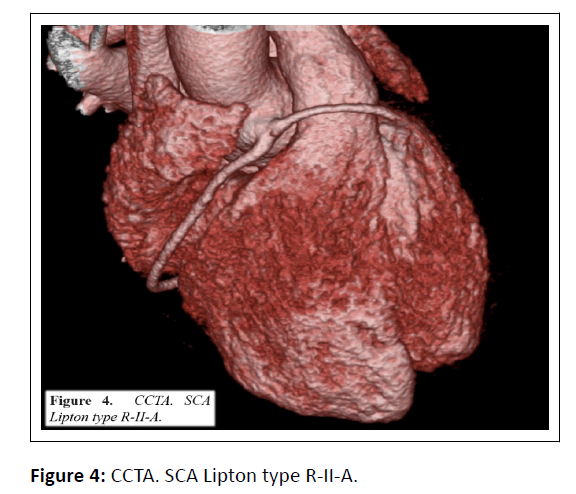
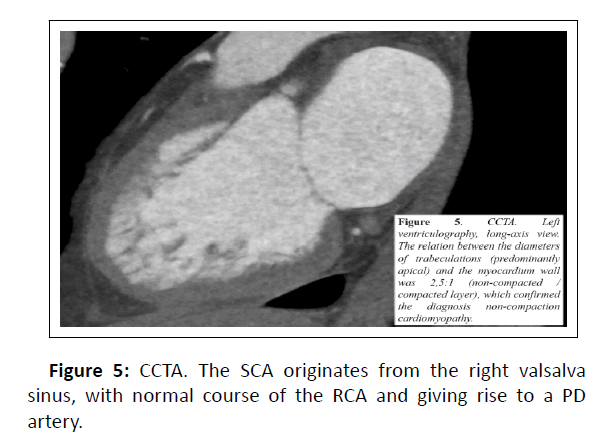
A 44-year-old male patient without comorbidities was admitted in the ICU with severe feeling of palpitations at rest during the last ten hours. A high-frequency AF was demonstrated on the ECG. Sinus rhythm was successfully restored with amiodarone and sustained with beta-blocker. Nevertheless, the patient had manifestations of HF NYHA III functional class. The TTE showed a moderate LV hypertrophy with apical trabeculations, LVEF% 47%, low grade tricuspid regurgitation with mild pulmonary hypertension. The CA identified a SCA, originating from the right coronary sinus. The short common trunk was divided into a RCA with a normal course and a left one that passes in front of the right ventricle and the pulmonary artery and bifurcating to LAD and LCx. The case was Lipton type [1] R-II-A figure 4. Left ventriculography showed LV systolic dysfunction and marked trabecularization of the LV myocardium. The CCTA was performed to confirm the diagnosis. The presence of a CAA and its course were confirmed and the relation between the diameters of trabeculations (predominantly apical) and the myocardium wall was 2, 5:1 (non-compacted / compacted layer), which confirmed the diagnosis no compaction cardiomyopathy figure 5. A HF treatment (ACE-inhibitor, a beta blocker, and diuretics), an antiarrhythmic drug to control the heart rhythm and a NOAC were started. An ICD implantation was indicated for SCD prophylactics, but the patient refused, and discharge asymptomatic.
Case 7
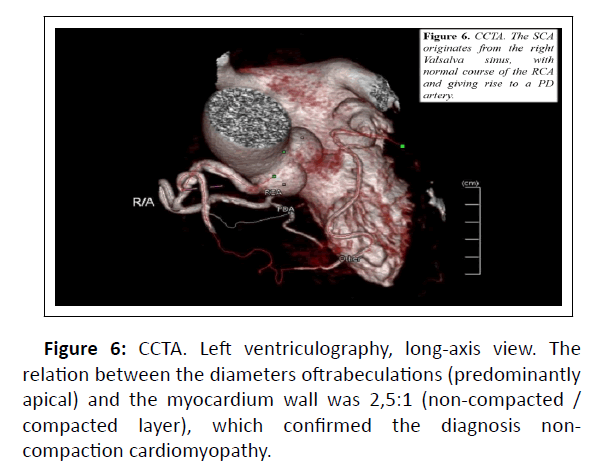
A 60-years-old female patient with stable angina, with previous history of paroxysmal AF, but at presentation she was in sinus rhythm, with arterial hypertension, hyperlipidemia and COPD. The TTE showed first grade diastolic disfunction and mild LV hypertrophy. A positive for ischemia stress test was performed with dynamic ST depressions in the inferolateral leads. The CCTA revealed a SCA, originating from the right Valsalva sinus, with normal course of the RCA and giving rise to a PD artery figure 6. At the origin of the common trunk, an acute take-off left main branch with frontal course over the right ventricle epicardial surface, reaching the apex, giving rise to a branch supplying the free LV wall and continuing in the anterior interventricular groove, bifurcating in to a diagonal and circumflex branch. A severe stenosis at the ostium of the anomalous branch was demonstrated by the selective CA. According to the proposed classification of Lipton et al. [1] the RII- A type was established. A decision for interventional treatment was taken. PCI strategy included ostial stenting with slight stent protrusion in the main branch. During the course in the ICU the patient was stable, with slight complaints of chest pain and non-significant rise in the high-sensitive troponin. She was discharged asymptomatic and in a stable clinical condition.
Case 8
A 66-years-old male patient was admitted for ACS. The comorbidities were an arterial hypertension and hyperlipidemia. The ECG presented a sinus rhythm and ST depression was registered in the inferolateral leads. The TTE showed inferior and lateral LV hypokinesis and mildly reduced LV EF. The GRACE score demonstrated an intermediate risk (119 points). The CA discovered a SCA, originating from the right Valsalva sinus, with normal course of the RCA and giving rise of PL and PD after bifurcation, with a possible native proximal dissection and 50% stenosis before the bifurcation. The proximal part of the single vessel represented a mixed trunk with separately arising LAD and LCx. Moderate stenoses in the middle segments of the LAD and the first diagonal branch, as well as on the bifurcation of LCx and the obtuse marginal, was detected. The R-III Lipton type [1] was defined. A decision for interventional treatment was taken for the native dissection of the proximal RCA and a DES was implanted. The patient was discharged on OMT, including dual antithrombotic, anti-ischemic and antihypertensive therapy with 12 months uneventful follow-up.
Case 9
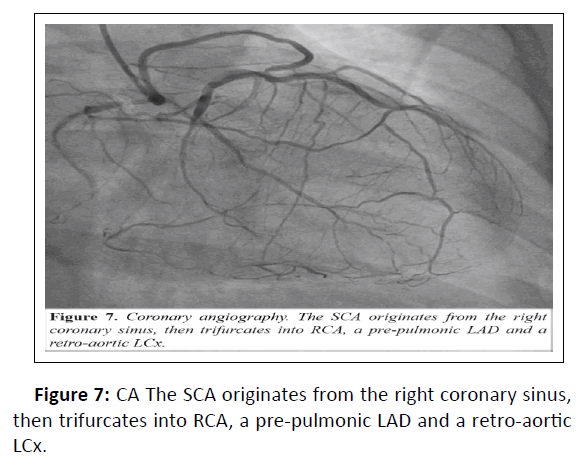
A 61-year-old female patient with obesity and dyslipidemia was admitted for new onset of chest pain. An inferior LV ischemia pattern was demonstrated on the ECG and elevated laboratory markers for myocardial necrosis were evident. TTE demonstrated a LV EF% of 55%. The CA failed to image a coronary ostium in left Valsalva sinus, but identified a SCA, originating from the right coronary sinus, with proximal trifurcation to RCA, a pre-pulmonic LAD and a retro-aortic LCx figure 7. According to the proposed Lipton classification [1] the R-III type was presented. The proximal part of RCA had a subtotal occlusion, treated with DES implantation. The patient was discharged asymptomatic, and 6th and 12th months uneventful follow-up were registered.
Case 10
A 75-years-old female patient with palpitations and dyspnoea at minimal effort in the last 3 months, accelerated a week ago.
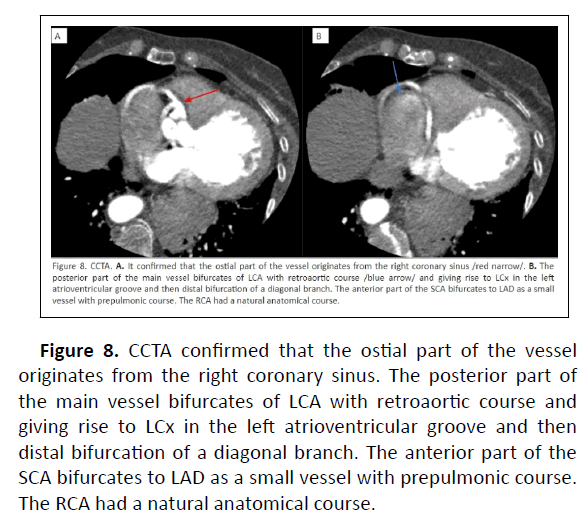
The concomitant diseases were arterial hypertension and chronic obstructive pulmonary disease. The physical exam presented stable hemodynamic, high-pitched, crescendodecrescendo, midsystolic ejection murmur at the right upper sternal border radiating to the neck, impaired mobility, and bilateral ankle oedema. The blood lipid levels were elevated. The ECG demonstrated sinus rhythm, left anterior fascicular block, ST-depression, and negative T-waves in the left (I, aVL) and septo-lateral precordial leads (V4-V6). TTE consisted a mild reduction in LVEF with normal segmental kinetics, but severe LV hypertrophy, dilated left and right atrium, a mitral valve leaflet prolapse (P2) and moderate mitral valve regurgitation, bicuspid aortic valve with severe stenosis (PG/MG=98/54 mmHg, AVA VTI–0.96 cm2) and severe insufficiency, mild tricuspid insufficiency and severe pulmonary hypertension (PAP=48 mmHg). On the x-ray of thorax, the left heart border was displaced leftward. A peripheral artery disease was rejected. We performed CA, as we found SCA originating from the right coronary sinus, with separate bifurcation of the LCA, giving rise separately of the LCx and the LAD. The left coronary sinus was free from the coronary ostia. CCTA confirmed that the ostial part of the vessel originates from the right coronary sinus figure 8. The posterior part of the main vessel bifurcates of LCA with retroaortic course and giving rise to LCx in the left atrioventricular groove and then distal bifurcation of a diagonal branch. The anterior part of the SCA bifurcates to LAD as a small vessel with psrepulmonic course. The RCA had a natural anatomical course. By Lipton classification [1] this case was type R-III SCA. There were no significant coronary artery stenoses, but a mild LV systolic dysfunction. The “mixed thrunk” [12] was inserted in 10.5 mm above the aortic ring. The aortic valve was bicuspid with raphe between the right and the left aortic valve leaflet (Sievers type I R/L). The HEART team decided to proceed to endovascular treatment (TAVI), due to the high surgical risk, including older age, frailty, poor mobility, and elevated comorbidity (chronic obstructive pulmonary disease, pulmonary hypertension, chronic kidney dysfunction), as also the life expectancy>1 year and the patient preference.
Figure 8: CCTA confirmed that the ostial part of the vessel originates from the right coronary sinus. The posterior part of the main vessel bifurcates of LCA with retroaortic course and giving rise to LCx in the left atrioventricular groove and then distal bifurcation of a diagonal branch. The anterior part of the SCA bifurcates to LAD as a small vessel with prepulmonic course. The RCA had a natural anatomical course.
Discussion
The frequency of the anomalous origin of the RCA is analyzed by Taylor and associates [20], who reviewed a variety of anatomic variables of 21 cases (including ostial size, length of intramural course, angle of take-off, and the presence of symptoms), and concluded that the age of presentation ≥ 30 years was associated with a lower incidence of SCD, compared with earlier clinical presentation, a finding confirmed by our examined group of patients. The frequency of this anomaly in autopsy studies varies from 0.026 among white population to 0.25% among Japanese and Hispanic origin population [15-17]. A retrospective analysis of a Portuguese study group, including 28 patients with right ACAOS with interatrial course confirmed that the older population with this high-risk condition had lower number of adverse cardiac events, as the conservative strategy was related with improved outcomes during the follow-up period [16]. As shown in our case series the clinical presentation of SCA anomaly can vary in wide range between lack of symptoms, moderate myocardial ischemia, syncope or STelevation myocardial infarction, and SCD. [7,8] Myocardial ischemia or SCD are usually associated with the course of SCA between the aorta and main pulmonary artery due to a scissorslike mechanism, especially during exertion [7-14]. To understand the clinical impact of SCA anatomycal type, the fundamental challenge is the establishment of a mechanism causing coronary artery flow disturbance, responsible for inadequate blood flow to the dependent myocardium [12].
The following pathophysiological mechanisms were evaluated by Intravascular Ultrasonography (IVUS) and described in the literature: [12] 1. Coronary hypoplasia-the intramural intussuscepted segment of the proximal ectopic artery is smaller in circumference than the more distal extramural vessel; 2. Lateral compression-the cross-section of the intramural segment is characteristically not circular, but ovoid. The smaller diameter is further compressed during each systole, which manifests as pulsatile behavior during the cardiac cycle, related to changes in stroke volume (and pulsatility of the ascending aorta) and to tachycardia, which is evident by IVUS imaging when an experimental pharmacological challenge simulates exercise conditions [15]; 3. Stenotic segment length. We know in any coronary stenoses, the segmental length is another determinant factor of the ischemia severity [12]. The Sinoatrial nodal artery supplies the sinoatrial node and arises from the Right Coronary Artery (RCA) in around 60% of people and the LCx in about 40% of cases [17]. According to a Spanish registry, anomalous origin of the LCx is the most frequent [18-26]. The sinus node and the atrio-ventricular node impaired blood supply in SCA anomaly could be manifested in Electrocardiography (ECG), varying from normal to abnormal readings [17,18]. From 13 Spanish hospitals presents 98 CAAs (0.4%) in a total of 23,300 coronary angiograms. They include 46 LCx (47%), 25 RCA (25.5%), 10 left main (10.2%), 3 LAD (3.1%), 6 SCA (6.1%), and 8 other anomalies (8.2%). The most frequent indication for CA was angina (43.9%). Similar to our group of patients, 51% of patients had associated atherosclerotic disease and 16.3% of patients underwent treatment for the CAAs. No gender-related differences in the incidence of CAAs were found, confirmed by our series of patients. Like in most or the published studies, an anomalous origin of the LCx in this registry (arising from the right Valsalva sinus or the origin of the RCA) were the most frequent (47%) [18-26]. The anatomical relationship of the anomalous SCA with the aorta and pulmonary artery is an essential aspect, when describing a CAAs, because certain courses e.g interarterial are associated with a higher incidence of ischemia [19,20].As CA gives us a two-dimensional view of the coronary vasculature, the initial course could not be identified in some patients. This is the reason additional imaging methods such as TTE or transesophageal echocardiography, Magnetic Resonance Imaging (MRI), or CCTA frequently used in our practice, provide a more accurate three-dimensional view and are used to confirm these specific anatomical courses [21-24]. As a background for the different classifications serve three major collateral pathways at the cono-truncal level, which provide circulation between the right and left coronary systems in all congenital or acquired forms of one-sided coronary artery occlusion [1]. They include 1/ preconal ring, also known as Vieussens' arterial ring, 2/ retro-conal and 3/ retro aortic anastomotic ring, also known as Kugel atrial anastomotic network, coronary cascade, or intracoronary communication. F. Albuquerque et al. [16] performed CCTA-guided evaluation in 28 middle-aged individuals, 55 ± 17 years, with suspected CAD and a low-tointermediate cardiovascular risk and consisted a right ACAOS with interarterial course, as just 5 patients (17.9%) had shared ostia, or SCA anomaly. The majority of the patients had at least one high- risk anatomical feature /slit-like vessel origin, acute angle take-off (<480) intramural course and proximal vessel narrowing of the anomalous artery/, nevertheless a low number of adverse cardiac events was registered during a 45.5 months follow-up–just one patient, who was treated with non-urgent right-ACAOS related cardiac surgery, who had uneventful followup period [16].
Jahnke et al. [27] published a case of an SCA with coronary MRI and determination of the functional significance of concomitant CAD with adenosine perfusion imaging and dobutamine stress testing. Hypo perfusion of inferior and infer lateral segments required performing invasive CA and stenting of the distal segment of the dominant RCA [27]. This case demonstrates the role of cardiac MRI in the clarification of the pathophysiology of myocardial ischemia when SCA is present. Functional significance of SCA anatomy could be evaluated by means of stress-scintigraphy especially when LV systolic and diastolic functions are normal and in the presence of accompanying ECG abnormalities [28]. RCA atresia is another scenario to be distinguished from the SCA [29]. In both cases, RCA circulation is completely dependent on left coronary artery patency [29,30]. In a large series of 126,595 patients 0,019% had SCA, 40% of whom were associated with congenital heart diseases [31-33] conducted an echocardiographic registry by TTE of 2388 asymptomatic children and adolescents from 0–21 years of age and found coronary artery from the opposite sinus in 0.17% (4 of 2388) of subjects. Despite TTE is widely applicable in this age group, its role in adults is limited. Nowadays CCTA and MRA could be alternative of invasive CA for the diagnosis of CAAs. CCTA is a non-invasive, accurate, and sensitive technique, but is related to radiation exposure. Latter is absent in MRI, which allows assessment of ventricular size and function, shunt, perfusion, viability, and postoperative complications. On the other hand, the spatial resolution of MRI is inferior to CCTA and also is not applicable in patients with non-MRI compatible pacemakers and ICDs [33]. IVUS could be beneficial in case of presence of intramural segment of a coronary artery with interarterial course [33]. A study of 15 patients with interarterial coronary arteries (11, with intramural segments) assumes that a height-to-width ratio of greater than 1.3 can allow identification of an intramural segment with 100% sensitivity and 100% specificity [33-35]. A large Armed Forces Institute of Pathology study based on the 25-year review of autopsies for 6,3 million sudden nontraumatic deaths found that coronary artery from the opposite sinus was the most common cause and they account for 33% (64 of 126) of cardiovascular deaths, in all cases involved LCA with an interarterial course [33-35]. Two large autopsy registries of young athletes reported 23 deaths from left coronary artery from the opposite sinus and four deaths from right ones [19].
Agarwal et al. [33] describe the major anomalies with clinical consequences requiring treatment, including the ACAOS with interarterial course specifically with an intramural course, using recent technical advancements in echocardiography, CCTA, MRI, and CA for detailed coronary artery imaging. The highest risk of SCD is typically seen in cases with aortic intramural interconnecting segment (a proximal part of an anomalous coronary artery contained within the aortic wall or histologically defined as a coronary artery sharing the aortic wall media without an intervening adventitia) in association with an interarterial course of the anomalous coronary artery [33]. Treatment strategies in SCA group of patients include conservative, interventional and surgical treatment. Latter involves coronary unroofing (excising the common wall between the intramural proximal segment and the aorta to the point of exit of the coronary, creating a wide and perpendicular neoostium), coronary artery bypass grafting, and reimplantation (replacement of anomalous coronary artery to coronary sinus appropriately) [8-33]. In 2008 American Heart Association/ American College of Cardiology guidelines define a class I recommendation that surgical coronary revascularization is indicated when patients with a coronary artery from the opposite sinus have any of the following: 1/ anomalous left main coronary artery coursing between the great arteries; 2/ documented coronary ischemia secondary to coronary artery compression when the artery courses between the aorta and pulmonary artery, or intramurally; 3/ anomalous origin of the RCA coursing between the aorta and pulmonary artery with evidence of ischemia [37]. Based on clinical indications during a five-year period (December, 2016- December 2021) we performed selective CA of 11,597 patients. We found ten clinical cases of SCA, which complies with the frequency of this anomaly 0.09% of the study population. The age of the patients was ranged between 44 and 81 years. The results were confirmed and specified by CCTA in six of them. They all were classified by Lipton et al. [1] in several groups according to their origin, course, and their relation with the aorta and pulmonary artery. Female and male patients were in equipoise. Clinical presentation of ACS had 5 patients (50.0%), stable angina–2 (30.0%) and palpitations-3 patients (20%). Five clinical cases had moderate and three had mild left ventricular systolic dysfunction, as seven patients of the group presented with sinus rhythm disturbances–supraventricular cardiac arrhythmias (6 patients) and sinus tachycardia (one patient). Significant CAD had six of them, five of which were successfully treated with DES implantation, and one rejected any kind of interventional/ surgical treatment. In the five other cases an emergency endovascular revascularization was successfully performed. Four patients had not significant coronary artery stenoses, but had a specific course of SCA. One patient was referred for cardiovascular surgery in term of severe aortic and mitral valve regurgitation. An ICD was indicated for a patient with noncompaction cardiomyopathy to prevent a SCD. The last case of the series was referred for TAVI, as severe aortic stenosis in highsurgical- risk condition was presented. It was evident a higher frequency of right coronary sinus origin of the SCA (seven patients)–based on the Lipton classification[1]-R-III–four patients, R-II– three patents, as left origin is found in three patients (L-I-one, and L-II–two patients). ACS was dominant in the patients with right coronary ostial origin (4; 57.1%), as stable angina is equally presented in the two different ostial origins (1 in left, and 1 in right Valsalva sinus origin). Supraventricular arrythmias were common in left Valsalva coronary origin (2 patients), compared to right (2 patients), as conduction disorders (left or right BBB, left anterior FB) in left origin were common compared to the right-one (left anterior FB). Inferior and infero-lateral ischemia, detected by 12-leads ECG is consisted only in right ostial origin of the SCA, but just in two of seven patients (28.6%) was presented with moderately reduced LV EF. As compared to the above, all patients with left coronary origin had moderate LVEF reduction.
In our first case, we didn’t find any definitive signs of myocardial ischemia based on CA and clinical findings. Revascularization is recommended only if there is a significant atherosclerosis and documented ischemia [5], which was presented in seven of the cases. Based on clinical recommendations, we performed myocardial perfusion scintigraphy to detect an ischemic origin for patient’s symptoms and to further precise the treatment strategy. It demonstrated hypo perfusion in the RCA-related myocardial region. FFR was the next diagnostic step. The result was a distal coronary pressure/aortic pressure ratio–0.83, which rejected the need for further treatment. These anatomical findings from CA and CCTA should be differentiated from other CAAs, like a congenital absence of RCA, due to atresia. This anomaly was reported by Gupta et al. [29]. The RCA atresia is distinguished from the SCA by the presence of only one or two full diameter connecting collateral vessels, the retrograde filling through full diameter intracoronary communication, the absence of typical clinical angina and lack of evidence of myocardial scarring, the absence of ostial stump on CCTA, and RCA was filling retrograde almost up to its proximal part by LCx, continuing in the right atrioventricular groove. In SCA occasion RCA circulation is completely dependent on left coronary artery patency [30]. Different approaches are available to treat the myocardial ischemia and its consequences [28]. Presented a 63- year-old Chinese woman with unprovoked chest oppression for one month and multiple premature beats detected on cardiac auscultation and dynamic electrocardiography. CCTA demonstrated SCA arising from the right coronary sinus of Valsalva, in the absence of the left coronary artery. The distal segment of the posterior descending artery gives off a small branch in the rear of the cardiac apex and terminates at the anterior wall of the LV, another small-diameter aberrantcoursing artery which originated from the distal of posterior left ventricular artery supplies lateral wall of LV, or Lipton R-I type. As the calcium score is measured zero and no abnormity is showed in the systolic and diastolic function in LV angiography, the patient was referred for electrophysiology testing and radiofrequency ablation to treat ventricular premature beats. In our SCA group of patients, cardiac rhythm disorders were common (in six of the cases- 60%) and moderate LV systolic dysfunction in five of them (50%). This coronary anatomy may result in insufficient flow delivery not only to RCA but also to the left coronary system with or without coronary stenosis, explaining the LV systolic dysfunction. The Sinoatrial nodal artery could arise more frequently from the RCA as from the LCx [16]. Lack of adequate blood supply due to this anomaly may lead to ischemia in the sinoatrial or atrioventricular node with eventual fibrosis and dysfunction. This might be manifested in ECG varying from normal to abnormal readings related to ischemia or arrhythmia [17]. LV systolic dysfunction impairment could be due both to AF or coronary flow peculiarities of the vessels. When patent SCA is accompanied by significant valvular heart disease, which is subject to surgical treatment, like in our fourth case, it is essential to specify the course of the anomalous coronary vessel, as certain courses /e.g, interarterial/ are associated with a higher incidence of ischemia and sudden cardiac death both peri- and post-operatively, and require revascularization [7,8,14,19,20].
Conclusions
The SCA is a rare anatomical condition, with a frequency of 0.09% in the studied Bulgarian population. The relations between patient complaints on the one hand, and the structural and functional components of ischemic events on the other, in SCA anomaly, are subject to a variety of diagnostic methods. Atherosclerosis-related or not, SCA anomaly alone could be a possible source of myocardial ischemia. The high prevalence of ACS, atrial fibrillation and reduced LV systolic function are evident in the study group. The origin of SCA from the left coronary sinus was accompanied by rhythm disorders and moderately reduced LV systolic function. The clinical and instrumental evidence of ACS was more frequent in anatomical origin of SCA from the right sinus of Valsalva. The revascularization strategy (surgical or interventional) could be salvage in high-risk anatomy in preventing а life-threatening condition, even if patients have not severe atherosclerotic coronary stenosis. When the patient is indicated for, it is essential to assess and discuss the accurate surgical approach. Clinical manifestation, anatomical course, atherosclerotic involvement of SCA, the concomitant indication for cardio surgical procedure guided the therapeutic choice, including the method for myocardial revascularization. Management of these patients needs complex decisions taken by the multidisciplinary “heart team”.
References
- Lipton MJ, Barry WH, Obrez I, Silverman JF, Wexler L (1979) Isolated single coronary artery: diagnosis, angiographic classification, and clinical significance. Radiology 130: 39–47.
[Crossref], [Google scholar], [Indexed]
- Desmet W, Vanhaecke J, Vrolix M, De Werf FV, Piessens J, et al. (1992) Isolated single coronary artery: a review of 50,000 consecutive coronary angiographies. Eur Heart J 13: 1637–40.
[Crossref], [Google scholar], [Indexed]
- Yamanaka O, Hobbs RE (1990) Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Catheter Cardiovasc Diagn 21: 28–40.
[Crossref], [Google scholar], [Indexed]
- Angelini P (1989) Normal and anomalous coronary arteries: Definitions and classification. Am Heart J 117: 418–34.
[Crossref], [Google scholar], [Indexed]
- Ferhat O, Halit A, Mehmet ZB, Abdurrahman T (2012) A rare coronary artery anomaly: single coronary artery originate from right sinus valsalva r-iip sub-group type. Cardiol Res 3: 140-2.
[Crossref], [Google scholar], [Indexed]
- Mohanty A (2015) A review on ' single coronary artery'. J Interv Radiol 11: 941-63.
- Matthew C, James P, Scott K, Michael Q, David, H (2009) Single Coronary Artery. J Am Coll Cardiol 53: 455.
- Shirani J, Roberts WC (1993) Solitary coronary ostium in the aorta in the absence of other major congenital cardiovascular anomalies. J Am Coll Cardiol 21: 137-43.
[Crossref], [Google scholar], [Indexed]
- Grollman JH Jr, Mao SS, Weinstein SR (1992) Arteriographic demonstration of both kinking at the origin and compression between the great vessels of an anomalous right coronary artery arising in common with a left coronary artery from above the left sinus of Valsalva. Cathet Cardiovasc Diagn 25: 46–51.
- Guntekin U, Saglam E, Tuncer M, Gunes Y, Gumrukcuoglu H (2009) Incidence of coronary artery anomalies in applied coronary angiography at our clinic. MN Kardiyoloji 16: 19–24.
- Angelini P (2007) Coronary artery anomalies an entity in search of an identity. Circulation 115: 1296-305.
[Crossref], [Google scholar], [Indexed]
- Angelini P, Villason S, Chan AV, Diez JG (1999) Normal and anomalous coronary arteries in humans. In: Angelini P, ed. Coronary artery anomalies: a comprehensive approach. philadelphia: lippincott williams and wilkins. 27–150.
[Crossref], [Google scholar]
- Angelini P, Velasco JA, Flamm S (2002) Coronary anomalies: Incidence, pathophysiology and clinical relevance. Circulation 105: 2449–54.
- Angelini P (2002) Coronary artery anomalies-current clinical issues: Definitions, classification, incidence, clinical relevance, and treatment guidelines. Tex Heart Inst J 29: 271–8.
[Crossref], [Google scholar], [Indexed]
- Alexander RW, Griffiths GC (1956) Anomalies of the coronary arteries and their clinical significance. Circulation 14: 800–5.
[Crossref], [Google scholar]
- Topaz O, DeMarchena EJ, Perin E, Sommer LS, Chahine RA (1992) Anomalous coronary arteries: angiographic findings in 80 patients. Int J Cardiol 34: 129–38.
[Crossref], [Google scholar], [Indexed]
- Albuquerque F, Goncalves PDA, Marques H, Ferreira A, Freitas P, et al. (2021) Anomalous origin of the right coronary artery with interarterial course: a mid-term follow-up of 28 cases. Scientific Reports . [Crossref], [Google scholar]
- Barriales-Villa R, Moris C, Sanmartin JC, Fernandez E, Pajin F, et al. (2006) Anomalous coronary artery registry of thirteen spanish hospitals (RACES). Rev Esp Cardiol 59: 620-3.
[Crossref], [Google scholar]
- Basso C, Maron BJ, Corrado D, Thiene G (2000) Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes. J Am Coll Cardiol 3: 1493-1501.
[Crossref], [Google scholar], [Indexed]
- Taylor AJ, Byers JP, Cheitlin MD, Virmani R (1997) Anomalous right or left coronary artery from the contralateral coronary sinus: “high risk” abnormalities in the initial coronary artery course and heterogeneus clinical outcomes. Am Heart J 133: 428-35.
[Crossref], [Google scholar], [Indexed]
- Vicente T, et al. Utilidad de la ecocardiografia transesofagica en el diagnostico de anomalias coronarias. Rev Esp Cardiol 49: 657-2. (1996)
- Ropers D, Moshage W, Daniel WG, Jessl J, Gottwik M, et al. (2001) Visualization of coronary artery anomalies and their anatomic course by contrast-enhaced electrom beam tomography and three-dimensional reconstruction. Am J Cardiol 87: 193-7.
[Crossref], [Google scholar], [Indexed]
- Barriales-Villa R, Moris C (2001) Usefulness of helical computed tomography in the identification of the initial course of coronary anomalies. Am J Cardiol 88: 719.
[Crossref], [Google scholar], [Indexed]
- Bunce NH, Lorenz CH, Keegan J, Lesser J, Reyes EM, et al. (2003) Coronary artery anomalies: assessment with free-breathing three- dimensional coronary MR angiography. Radiology 227: 201-8.
[Crossref], [Google scholar], [Indexed]
- Barriales-Villa R, Muniz AL, Hernandez LC, Roman LS, De La Hera JM, et al. (2001) Congenital anomalies of the coronary arteries in adults described in 31 years of coronary angiographic studies in the principality of asturias: Main clinical angiographic characteristics. Rev Esp Cardiol 54: 269-81.
[Crossref], [Google scholar]
- Click RL, Holmes DR, Vlietstra RE, Kosinski AS, Kronmal RA (1989) Anomalous coronary arteries: location, degree of atherosclerosis and effect on survival; A report from the coronary artery surgery study. J Am Coll Cardiol 13: 531-7.
[Crossref], [Google scholar], [Indexed]
- Jahnke C, et al. (2006) Diagnosis of a “Single” Coronary Artery and Determination of Functional Significance of Concomitant Coronary Artery Disease. Circulation 113: e386-e387.
[Crossref], [Google scholar]
- Fengli F, Hongfeng J, Feng Y (2015) A rare case of single right coronary artery with congenital absence of left coronary artery in an adult: A case report; J Cardiothorac Surg 10: 57.
[Crossref], [Google scholar]
- Mohit DG, Girish MP, Vignesh V, Narang P, Trehan V, et al. (2015) Absent right coronary artery: A case of single coronary artery or congenital ostial atresia? Indian Heart J 67 s11-s13.
[Crossref], [Google scholar], [Indexed]
- Angelini P (2012) Congenital coronary artery ostial disease: a spectrum of anatomic variants with different pathophysiologies and prognoses. Tex Heart Inst J 39: 55–9.
- Roberts WC (1986) Major anomalies of coronary arterial origin seen in adulthood. Am Heart J. 111: 941-63.
[Crossref], [Google scholar], [Indexed]
- Angelini P, Walmsley RP, Libreros A, Ott DA (2006) Symptomatic anomalous origination of the left coronary artery from the opposite sinus of Valsalva. Clinical presentations, diagnosis, and surgical repair. Tex Heart Inst J 33: 171–9.
- Davis JA, Cecchin F, Jones TK, Portman MA (2001) Major coronary artery anomalies in a pediatric population: incidence and clinical importance. J Am Coll Cardiol 37: 593–7.
[Crossref], [Google scholar], [Indexed]
- Prachi PA, Dennie C, Pena E, Nguyen E, LaBounty T, et al. (2017) Anomalous Coronary Arteries That Need Intervention: Review of Pre-and Postoperative Imaging Appearances. RadioGraphics 37: 740–57.
[Crossref], [Google scholar]
- Eckart RE, Scoville SL, Campbell CL, Shry EA, Stajduhar KC, et al. (2004) Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med 141: 829–34. (2004).
[Crossref], [Google scholar], [Indexed]
- Miller JA, Anavekar NS, El Yaman MM, Burkhart HM, Miller AJ, et al. (2012) Computed tomographic angiography identification of intramural segments in anomalous coronary arteries with interarterial course. Int J Cardiovasc Imaging 28: 1525–32.
[Crossref], [Google scholar], [Indexed]
- Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, et al. (2008) ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: A report of the american college of cardiology/american heart association task force on practice guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease)—developed in collaboration with the american society of echocardiography, heart rhythm society, international society for adult congenital heart disease, society for cardiovascular angiography and interventions, and society of thoracic surgeons. J Am Coll Cardiol 52: e143–e263.
[Crossref], [Google scholar], [Indexed]
- Angelini P, Velasco JA, Ott D, Khoshnevis GR (2003) Anomalous coronary artery arising from the opposite sinus: descriptive features and pathophysiologic mechanisms, as documented by intravascular ultrasonography. J Invasive Cardiol. 15:507–14.
- Kaku B, Shimizu M, Yoshio H, Ino H, Ishise S, et al. (1996) Clinical features of prognosis of Japanese patients with anomalous origin of the coronary artery. Jpn Circ J 60: 731–41.
[Crossref], [Google scholar], [Indexed]
- Yan GW, Bhetuwal A, Yang GQ, Shui Fu Q, Hu N,et al. 2018 Congenital absence of the right coronary artery: A case report and literature review; Section Editor(s): NA., Medicine: 97- p e0187.
- Pejkovic B, Krajnc I, Anderhuber F, Kosutic D (2008) Anatomical aspects of the arterial blood supply to the sinoatrial and atrioventricular nodes of the human heart. Int J Med Res 36: 691–8.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences