Surgical Correction of Popliteal Vein Reflux in Recurrent and Active Venous Ulcer Could Be a Final Decision
Khalid Mowafy, Mosaad Soliman, Abdelsalam Megahed and Ahmed Elshazly
DOI10.21767/2573-4482.18.03.22
1 Department of Vascular and Endovascular Surgery, Mansoura College of Medicine, Mansoura University, Egypt
2 Department of General Surgery, Mansoura College of Medicine, Mansoura University, Egypt
- *Corresponding Author:
- Khalid Abdel Aziz Mowafy
Department of Vascular And Endovascular Surgery,
Mansoura College of Medicine
Mansoura University, Egypt
Tel: 01223547905
Email : Khalid_mowaphy@mans.edu.eg
Received Date: October 26, 2018; Accepted Date: November 15, 2018; Published Date:November 22, 2018
Citation: Khalid AAM, Mosaad S, Abdelsalam M, Ahmed E (2018) Surgical Correction of Popliteal Vein Reflux in Recurrent and Active Venous Ulcer Could Be a Final Decision. J Vasc Endovasc Therapy. 3:22.
Abstract
Introduction: Candidates for deep venous valvular reconstruction typically have class 5/6 CEAP disease or disabling symptoms, such as severe edema (C4).
Aim of the Work: This study was conducted to further justify the durability of popliteal vein reflux correction in advanced chronic venous insufficiency patients.
Patients and Methods: This prospective non randomized study was carried out to evaluate the effectiveness of surgical correction of popliteal vein reflux .It was performed at vascular surgery department, Mansoura university, from January 2014 to January 2016 for 20 patients, divided as follow; 10 patients with secondary popliteal vein reflux underwent axillary vein valve tranfere, 10 patients with primary popliteal vein reflux underwent External Banding.
Results: On 12 months follow up: 2 cases (20%) showed recurrent ulcer and 8 cases (80%) showed complete healing of ulcer. Postoperative valve patency showed 3 cases with patent competent valves 30%. On 24 moth follow up only 1 case with competent valve with axillary vein valve transplant group and no valves were competent with external banding group.
Conclusion: In our study we recommend surgical correction in treatment of severe popliteal vein reflux patients.
Keywords
Vein reflux; Venous ulcer; Chronic venous; Vascular surgery; Ulcer
Introduction
Perpetual leg ulcer, regularly called endless lower appendage ulcer, is an injury of the real leg that shows truly no inclination to recuperate following three months of proper treatment or perhaps remains not completely mended at 12 weeks [1].
Venous leg ulcers (VLUs) are thought as open injuries between the knee and lower leg joint that happen in the notoriety of venous ailment. They are the most widely recognized reason for leg ulcers, representing 60%-80% ones [2].
The lower extremity calf-muscle pump is the primary mechanism for returning venous blood from the lower limb to the heart. The calf-muscle pump consists of calf muscles, deep-venous system, superficial venous compartment, perforating veins, and an out- ÃÆïÃâìÃâââ¬Å¡ow gate (popliteal vein). Dysfunction of any of the calf muscle pump components may result in elevated venous pressure or venous hypertension. Although there is no consensus on the specific pathogenic steps leading from venous HTN to venous ulceration, several hypotheses have been proposed [3].
Patients with venous ulcers will require medical and possibly surgical intervention to augment ulcer healing and prevent recurrence, surgical correction of superficial, perforating, or deep-venous system may be necessary for ulcer healing. The goal of surgical intervention is to improve venous hemodynamics when conservative therapy has failed treating all superficial and perforator vein insufficiency can reduce the recurrence risk, but it is still noted in up to 33% of patients with primary deep CVI and 70% of those with the post thrombotic syndrome. These facts demonstrate the importance of deep venous disease in the pathophysiologic process of CVI [4].
Rarely patients are observed with congenital absence of lower extremity venous valves, venous aplasia or dysplasia. More commonly patients with primary venous insufficiency have either floppy, redundant, elongated valve cusps or an enlarged venous diameter, both of which prevent normal valve cusp apposition [5]. In these cases, there is no apparent inciting event that caused the anatomic changes observed. As a consequence of these pathologic changes, spontaneously with standing or with additional stresses, reflux occurs in the affected valves. Except in the case of aplasia or dysplasia, in situ tightening (repair) of the structurally intact valve can render it competent and functional (Table 1) [6].
|
|
Axillary vein valve transplantation (n=10) | External Banding (n=10) | χ2 | P | ||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| History of DVT | 10 | 100 | 0 | 0 | 3.529 | 0.06 |
| Pain | 10 | 100 | 4 | 40 | 8.571 | 0.003* |
| Edema | 5 | 50 | 9 | 90 | 3.81 | 0.051 |
| Pigmentation | 10 | 100 | 8 | 80 | 2.222 | 0.136 |
| Dermatitis | 10 | 100 | 1 | 10 | 16.36 | <0.001* |
| History of previous surgery |
3 | 30 | 10 | 100 | 10.77 | 0.001* |
*Significant P<0.05
Table 1: Clinical presentation in patients with chronic venous insufficiency.
Secondary venous insufficiency is often the result of acute deep venous thrombosis (DVT) and in 40% to 70% of all affected patients may be the cause of chronic deep venous valvular incompetence [7]. The resulting inflammation and scarring with or without recanalization can cause foreshortening and fibrosis of the valve leaflets, small perforations, or valve adhesion and luminal narrowing. The valves are generally so damaged that in situ repair is not feasible. The options remaining to prevent complete system reflux are transplantation of a competent valve from a distant location, transposition of the incompetent venous system to a position distal to a local competent valve, or the use of less traditional valve substitutes [8]. Candidates for deep venous valvular reconstruction typically have class 5/6 CEAP disease or disabling symptoms, such as severe edema (C4) [9].
Aim of the Work
This study was conducted to further justify the durability of popliteal vein reflux correction in advanced venous insufficiency patients in terms of symptoms improvement, ulcer healing and symptoms/ulcer recurrence in patients who had recalcitrant nonhealing and recurrent leg ulcer as a last treatment decision.
Patient and Methods
This prospective non randomized study was carried out to evaluate the effectiveness of surgical correction of popliteal vein reflux .It was performed at vascular surgery department, Mansoura university, from Jan 2014 to Jan 2016 for 20 patients, divided as follow; 10 patients with secondary popliteal vein reflux underwent axillary vein valve tranfere, 10 patients with primary popliteal vein reflux underwent External Banding. All patients enrolled in this study were informed with all details of surgery, its benefit, operative and possible postoperative complications. A written consent was taken from all patients.
This study included 20 patients of both sexes with incompetent popliteal vein valve, and active venous ulcers (CEAP 6) and or history of recurrent ulcer (CEAP5),after failure of both superficial and perforators intervention in addition to strict commitment to conservative measures (Table 2).
| Axillary vein valve transplantation (n=10) | External Valvuloplasty (n=10) | χ2 | P | |||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| DuplexSFJ | ||||||
| Comp | 8 | 80 | 9 | 90 | 0.392 | 0.531 |
| Reflux | 2 | 20 | 1 | 10 | ||
| Popliteal vein valve | ||||||
| Sever incompetency | 10 | 100 | 7 | 70 | ||
| Moderate incompetency | 0 | 0% | 3 | 30 | 3.529 | 0.06 |
*Significant P<0.05
Table 2: Duplex findings in patients with chronic venous insufficiency.
Selection criteria
1. Patients suffering from chronic and active venous leg ulcer (CEAP6) resistant to conservative treatment>3 months and failed surgical treatment for perforators and saphenous system and duplex evidence of popliteal vein reflux.
2. Patients with history of recurrent venous ulcer despite strict Commitment to conservative measures (CEAP5) and duplex evidence of popliteal vein reflux.
Exclusion criteria
We excluded:
1. Patients with history of deep venous thrombosis within 6 months duration.
2. Patients with colour duplex scan finding of: Concomittent superficial vein reflux or perforators incompetence *(3 patients), Minimal popliteal valve reflux *(7 patients), evidence of proximal obstruction *(2 patients), Duplex finding of peripheral arterial insufficiency *(1 patient).
3. Evidence of coagulopathy
4. Generally unfit for surgery, psychiatric patients, and who refused to give a written consent.
5. *Excluded from the study.
Preoperative Assessment
A written consent was taken from all patients Included in the study and submitted to careful history taking, history of previous intervention or surgical procedures, DVT.
All patients were submitted to complete preoperative clinical examination that included general and local examination including skin fibrosis, venous ulcer pointed to the location, multiplicity, skin around, edge of the ulcer, necrotic tissue in the centre of the ulcer, the presence of granulation tissue, bleeding nidus, dilated veins, edema, leg pain and cutaneous changes, hyperpigmentation and lipodermatosclerosis associated with thickening and fibrosis of normal adipose tissue under skin (Table 3).
|
|
Axillary vein valve transplantation (n=10) | External Valvuloplasty (n = 10) | χ2 | P | ||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| Superficial thrombophlebitis | ||||||
| No | 8 | 80 | 10 | 100 | 2.222 | 0.136 |
| Recurrence | 2 | 20 | 0 | 0 | ||
| DVT | ||||||
| No DVT | 8 | 80 | 10 | 10 | 2.222 | 0.136 |
| DVT | 2 | 20 | 0 | 0 | ||
Table 3: Post-operative complication for deep system surgery.
Investigations
Patient underwent axillary vein valve transplantation had duplex scanning for competency of axillary vein valve.
All Patients were evaluated in the standing position to ensure maximum venous distention (Table 4).
|
|
Axillary vein valve transplantation (n=10) | External Valvuloplasty (n = 10) | χ2 | P | ||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| Follow up competent valve | ||||||
| 3 months | 8 | 80 | 10 | 100 | 2.222 | 0.136 |
| 6 | 4 | 40 | 8 | 80 | 3.333 | 0.068 |
| 9 | 3 | 30 | 4 | 40 | 0.22 | 0.639 |
| 12 | 2 | 20 | 3 | 30 | 0.267 | 0.606 |
| 18 | 1 | 10 | 2 | 20 | 0.392 | 0.531 |
| 24 | 1 | 10 | 0 | 0 | 1.053 | 0.305 |
Table 4: Valve competency after the surgery.
Venous duplex scanning (VDS) provided data concerning anatomy and hemodynamics. The presence and the duration of a deep reflux could be detected at femoral, popliteal and crural levels, While reflux could be evaluated using both color or pulsed-wave Doppler, we used pulsed-wave one. A small blip of color just after release of compression is considered physiologic, that represents a small amount of retrograde flow before complete closure of valves. Reflux was generally defined as greater than 0.5 seconds of flow reversal [10].
Venography was done in two patients presented by bilateral CVI, that showed ileocaval severe stenosis and they were excluded from our study (Table 5).
| Axillary vein valve transplantation (n=10) | External Valvuloplasty (n=10) | χ2 | P | |||
|---|---|---|---|---|---|---|
| No | % | No | % | |||
| Follow up 12 m | ||||||
| No healing | 2 | 20 | 0 | 0 | 5.067 | 0.167 |
| Healed | 7 | 70 | 8 | 80 | ||
| Incomplete Healing | 1 | 10 | 0 | 0 | ||
| Recurrent | 0 | 0 | 2 | 20 | ||
Table 5: Healing of ulcer in chronic venous insufficiency patient.
All patients were screened for hypercoagulability factors.
Patients were divided into 2 groups
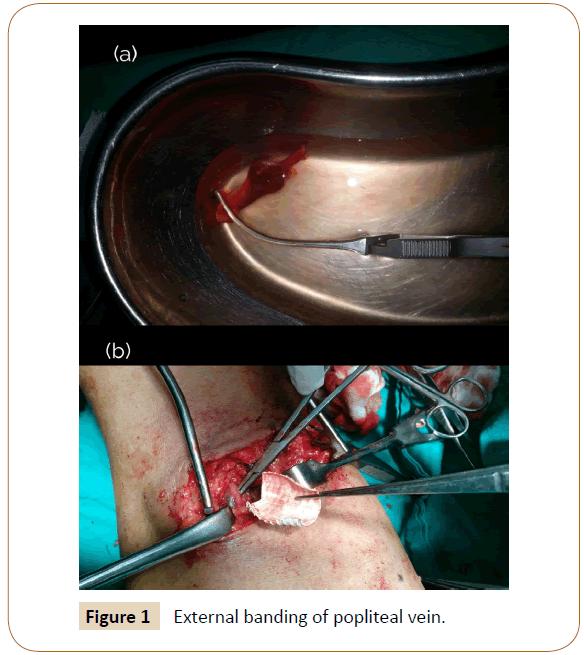
Group 1: 10 patients with primary reflux with incompetent popliteal vein valves with no duplex evidence of intraluminal wall thickening or fibrosis performed external vein banding for dilated floppy diseased vein. We used PTFE patch in all cases.
Surgical procedure: Preoperative duplex mapping for site of popliteal vein valve was mandatory before surgical intervention in all patients. Surgery was done under spinal anesthesia, patient with prone position; a lazy S access was made in the popliteal fossa to access popliteal vein. After identification of the vein proper the valve was dissected carefully and external banding by a polytetrafluoroethylene (PTFE) patch graft (Figure 1) was fashioned and encircled the valve. It was sutured by prolene 5/0 and was tested for competency by an intraoperative duplex sterilized probe, before sutures were taken to ensure valve competency.
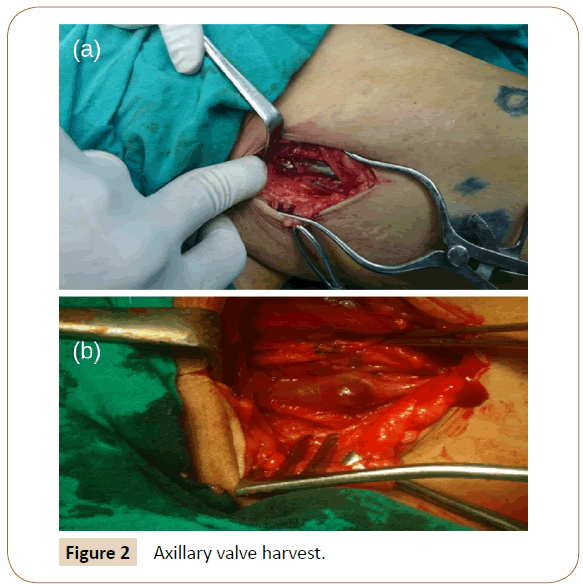
Group 2: 10 patients with secondary reflux performed axillary vein valve tranfere to the deformed popliteal vein with wall thickness and intraluminal trabecules, and cusp fibrosis (duplex criteria).
Surgical procedure: Patients who underwent axillary vein valve transferee used local Anesthesia first supine position with upper limb hyper abducted. Small incision in axilla about 4 cm parallel to the axillary vein, (Figure 2) we excised about 2-3 cm of the axillary vein with visible axillary valve cusp, the level of axillary segment can be shifted upper or lower to match the size of popliteal vein, finally we ligated the proximal and distal segments of the axillary vein with VICRYL (2/0). Closure of the fascia and skin with prolene 3/0 interrupted suture.
Then with the patient in prone position, exposure of popliteal vein, meticulous ligation and division of tributaries of the popliteal vein and immediate hepranization of the patient by unfractionated heparin 5.000 unit; after clamping the popliteal vein.
The valve bearing segment should be inserted under optimal tension with no hint of torsion or angulation the upper suture line is performed first and the valve was tested by removing the clamp and if possible stripping the blood in the segment above against the valve (positive strip test).
When anastomosis between transferred valve and popliteal vein was completed, intraoperative duplex probe was used for assurance of competency, closure with drain which was removed by the second day postoperative.
Postoperative care
Patients received postoperative broad spectrum oral antibiotic 5 days, anticoagulanted (enoxaparin sodium according to body weight 150 iu/kg) for 5 days with start of oral anticoagulant (warfarin sodium) 24 hours after surgery for 6 months monitored by INR. Compression stocking immediately after removal of the drains with early ambulation.
Patients were discharged one week after reaching a target of international normalized ratio (INR) (2-2.5).
Outcome assessment and follow up
Ulcer criteria (length, width, depth), healthy granulation, infection.
Ulcers that never healed after the procedure were counted as recurrences at the follow up visit after the grace period for calculation of accurate data.
Swelling graded- o absent, 1 pitting not gross, 2 visible ankle edema 3 massive entire the leg.
Pain patient were asked to indicate their level of pain on visual analogue ranging from 0 to 10 [11].
All patients were followed up clinically and by duplex scanning weekly in first month, and at 3,6,12,18 and 24 months postoperative to show valve competency.
Patients also examined for presence of DVT, and ulcer healing.
Statistical analysis
Data was analyzed using SPSS (Statistical Package for Social Sciences) version 15. Qualitative data was presented as number and percent. Comparison between groups was done by Chi- Square test. Quantitative data was presented as mean ± SD. Student t-test was used to compare between two groups. Survival curves were calculated using the Kaplan-Meier product limit method and their difference/comparisons assessed by logrank test. P<0.05 was considered to be statistically significant.
Results
Our study was conducted on 20 patients with CVI with 19 males (95%) and one female (5%) The age of our patients ranged from 20 to 45 years old with mean age of 31 years old.
All patients who performed Axillary vein valve transferee (n=10) had history of DVT (100%). Pain and ulcer were found in all cases. On examination, edema was present in 5 cases (50%). Pigmentations& dermatitis were present in all cases. All patients’s had previous attack for superficial and incompetent perforators.
All patients who performed External banding (n=10) were presented with history of superficial venous system surgery. Three limbs stripped GSV (30%) and seven limbs underwent surgery for perforators and stripped GSV (70%), pain in 4 cases (40%) and ulcer was presented in 7 cases CEAP 6 (70%) and the other 3 cases were CEAP 5. On examination, edema was present in 9 cases (90%). Pigmentations were present in 8 cases (80%), dermatitis in 2 cases (20%).
On CEAP classifications 17 cases were grade 6 (85%) and 3 cases were grade 5 (15%).
Femoral vein valves were competent in 17 cases (85%) and incompetent in 3 cases (15%), all cases by duplex US showed incompetent popliteal vein valves, 17 cases were with sever reflux (85%) and other 3 cases with moderate reflux (15%).
Valve bearing segment used for replacing the deformed popliteal vein valve was harvested from the left axillary vein in 6 patients and from the right side in 4 patients, all was preoperatively mapped by duplex scan and they were all (10 patients) the first valve after the venous angle, all could be taken from axillary incision.
Follow Up: Patient included in the study was subjected to follow up ranged from 3 months to 24 months.
Group 1 (valve transferee)
On 3 months follow up: 3 cases (30%) show no healing and 7 cases (70%) showed complete healing of ulcer. Postoperative valve patency showed 8 cases with patent competent valves (80%).
On 6 months follow up: 2 cases (20%) show no healing, 1 case (10%) showed incomplete healing and 7 cases (7%) showed complete healing of ulcer. Postoperative valve patency showed 4 cases with patent competent valves (40%).
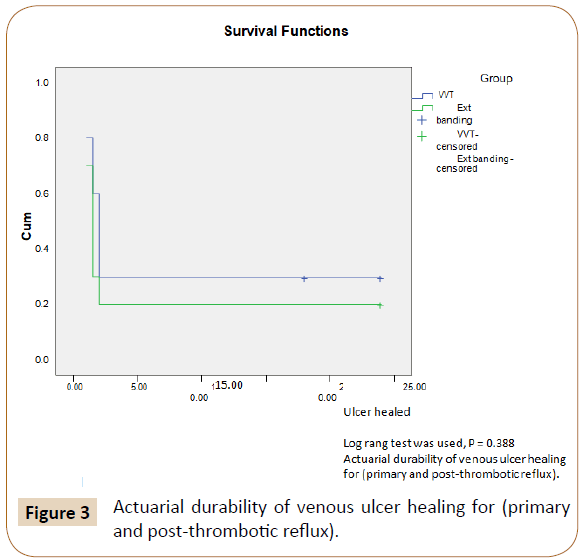
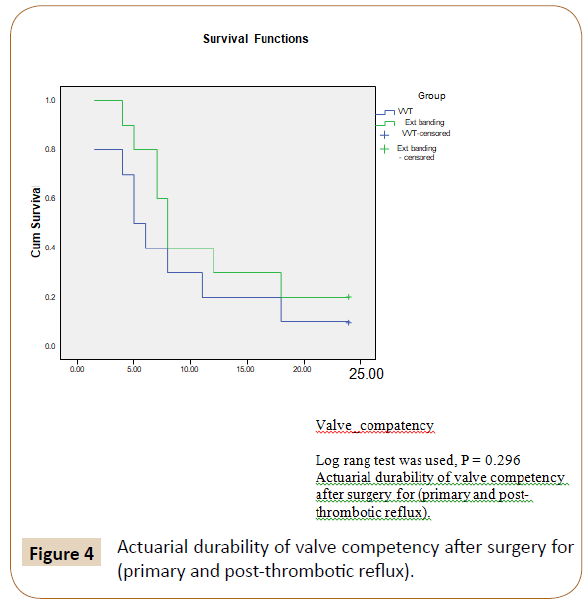
On 12 months follow up: 2 cases (20%) show no healing, 1 case (10%) showed incomplete healing and 7 cases (7%) showed complete healing of ulcer (Figure 3). Postoperative valve patency showed 2 cases with patent competent valves (20%) (Figure 4).
Group 2 (external banding)
On 3 and 6 months follow up: All 10 cases (100%) showed complete healing of ulcer. Postoperative valve patency showed 10 cases with patent competent valves by the third month but 8 at the six month (80%).
On 12 months follow up: 2 cases (20%) showed recurrent ulcer and 8 cases (80%) showed complete healing of ulcer.
Postoperative valve patency showed 3 cases with patent competent valves 30%.
On 24 months follow up: Only 1 case with competent valve with axillary vein valve transplant group and no valves were competent with external banding group.
Morbidity and Mortality
On post-operative follow up quality of life has been assessed based on absence or presence of the following criteria (Hematoma, DVT, Superficial thrombophlebitis and pain).
Patients with external Banding had no either superficial thrombophlebitis nor DVT. 2 cases suffered from postoperative pain (20%) and 3 cases had Hematoma (30%).
Patients with axillary vein valve transplantation had DVT (20%) 2 cases, Superficial thrombophlebitis (20%). 2 cases and 3 cases had Hematoma on upper limb (30%), and 3 cases suffered from pain on 3 months follow up but only 2 cases had pain by 6 months and one case by 9 month follow up.
There was no mortality in our studied patients.
Discussion
Volume of reflux is one of the most important determinants of severity of chronic venous insufficiency. Stasis-induced symptoms and signs of chronic venous hypertension in deep vein reflexive disease are more than likely due to large-volume reflux, the compensatory mechanisms such as calf-pump action and perforator valve function gradually deteriorate with increased deep vein reflux [12]. In chronic venous insufficiency, deep vein reflux occurs in the majority of patients, either alone or in combination with superficial or perforator vein incompetence.
Surgery of the insufficient superficial or perforator venous systems, in the presence of deep venous reflux, leads to poor healing of venous ulcers in majority of patients [13].
Hence, this group, in whom recurrence of leg ulceration is significant even after superficial and perforator vein surgery, and the group that has deep venous reflux without superficial vein involvement, constitute a significant number of venous leg ulceration patients in whom deep venous valve reconstruction surgery becomes a last option [2]. Venous Color duplex ultrasound scanning which is becoming the de facto standard for evaluation of venous obstruction is also used to assess the location and extent of reflux in venous ulcers [14].
Corrective surgery in deep-venous reflux is not practiced often for reasons not quite known, though many consider it risky, others think it pointless, and still others judge it insufficiently validated in time. In actual fact, this type of surgery is generally non-aggressive and entails a low rate of complication. The results achieved partly fade in time due to the evolving nature of the disease, but the benefits occurring to over half the patients for a period of over 5 years are by no means negligible [15].
Results of deep venous reconstructive surgery (DVRS) for reflux are satisfactory despite the fact that patients are usually treated by surgery usually in the advanced phases of chronic venous insufficiency [16].
Our study presents results expressed at 2 years in a continuing short-term follow up of all patients with venous leg ulcerations (CEAP C6) (CEAP 5) due to deep venous reflux. These patients had non-healing venous ulceration despite superficial and perforator vein surgery and trial of conservative management for more than 3 months on venotropic drugs and compression therapy.
Although the CEAP classification has proven to be a useful descriptive instrument in classifying venous conditions, more information is needed regarding disease severity and longitudinal changes in patient conditions during treatment [17]. In response to this need for a disease severity measurement, the American Venous Forum in 2000 derived the Venous Severity Scoring (VCSS) system from elements of the CEAP classification [18]. In our study we used CEAP classification as our patients were in advanced stage and our main target was focused on ulcer healing. 20 patients with chronic venous insufficiency with CEAP classifications 17 cases were grade 6 (85%) and 3 cases were grade 5 (15%).
The ideal site for repair of valve is still debated. Sottiurai and others believe that the popliteal vein is the gatekeeper of the leg veins and we recommend popliteal level repair, and in a study by Sottiurai et al. they showed 80% ulcer healing in primary valvular reflux patients who underwent Valvuloplasty and superficial venous surgery.
He further showed 75% ulcer healing in secondary reflux patients who underwent vein valve and transplant in combination with superficial venous surgery [13].
While Perrin et al. 2000 worked on 32 diseased valves they transplant into femoral vein only. Thirty-one patient from thirty-two (96%) had postphelebitic leg with non-healed ulcer 41% with competent valves 25% at the end of study [15]. Lane et al. Conducted study on 42 limbs with repair of 125 diseased valves; they worked on femoral and popliteal veins external banding 36 limbs from 42 had primary reflux 85% with mean follow up 93 months; they demonstrated healing of ulcer in 80% with competent valve about 90% [19]. Rameshtripathi, et al. demonstrated ulcer healing in 63.5% of limbs in the primary reflexive disease who underwent external Valvuloplasty and 47% in secondary reflexive disease who underwent axillary valve transplantation, Tripathi, 2004 worked on 35 limb all of them had postphelebitic leg. He transplanted the valve into femoral and popliteal vein with mean follow up 24 months. He had non healing ulcer into 45% with competent valve 41% [20].
Maleti and Perrin, Showed Successful outcome can be put between 33%-82% ulcer healing with follow up 1 year with valve competency 16%-87% in transplanted result [16].
In our study we demonstrated ulcer healing of 80% of limbs in the primary reflexive disease who underwent external banding and 70% in secondary reflexive disease who underwent axillary valve transplantation.
These comparative data suggest that when deep vein reflux is associated with superficial venous incompetence, superficial venous surgery alone for these patients will result in non-healing or recurrence of a majority of these leg ulcers.
In our study a curious phenomenon was observed on duplex scan follow up, most of valves lost their competency by first year follow up only (20%) of the valves were competent in secondary reflux group who underwent axillary vein valve transplantation and only (30%) of the valves were competent in primary reflux group who underwent external banding and patients who developed loss of competence following valve transplan showed complete absence of valves or ‘valve resorption’. This may be due to collagenolysis following trauma to valve leaflets or due to persistent distal reflux [21].
In our study we observed postoperative thrombosis in 20% in secondary reflux patient who underwent axillary valve transplantation and no patients who underwent external banding had DVT. While, Tripathi et al. observed 6.7% limbs in the primary reflux group and in 25.4% limbs in the secondary reflux group, had DVT; all axillary transferee patients experienced postoperative mild to moderate oedema of the upper limb that was managed with elevation and compression bandages and resolved completely after 2 weeks postoperatively.
Our experience is therefore more in concordance reported in the present study. These thrombotic events occurred despite adequate anticoagulation.
For secondary valvular reflux, valve transplants we have used valve graft from axillary vein, however Tripathi et al. used brachial venous segments or from the opposite great saphenous vein. An attempt was made to harvest a segment of vein with at least two competent valve stations, wherever possible [20]. But we used one valve segment from the axillary vein that matches well with the diameter of popliteal vein.
The early results of the present series indicate that valvular reconstruction is more durable when performed for primary reflexive disease and valve transplantation useful for healing of postphlebetic ulcer.
Conclusion
In our study we recommend surgical correction in treatment of severe popliteal vein reflux patients that provide healing of venous ulcer in about 70% of patients who had secondary reflux, 80% in primary reflux patients at 2 years following operation in spite of loss of most of the valves competence at the end of our study. Also, all complications after surgery were minimal and reversible.
However, these parameters of assessment need more evaluation and analysis guided by large number of patients, long term follow up and multicentric randomized study to reach a final decision in this critical and debatable point.
References
- Kahle B, Hermanns HI, Gallenkemper G (2011) Evidence based treatment of chronic leg ulcers. Dtsch Arztebl Int 108: 231-237.
- O’Meara S, Al-Kurdi D, Ovington LG (2014) Antibiotics and antiseptics for venous leg ulcers. Cochrane Database Syst Rev CD003557.
- Cheatle TR, Coleridge Smith PD, Scurr JH (2007) Skin microcirculatory responses in chronic venous insufÃÆïÃâìÃâÃÂciency: The effect of short-term venous hypertension. Vasa 20: 63-69.
- Kalra M, Gloviczki P (2003) Surgical treatment of venous ulcers: role of subfascial endoscopic perforator vein ligation. Surg Clin North Am 83: 671-705.
- Raju S, Berry MA, Neglén P (2000) Transcommissural valvuloplasty: Technique and results. J Vasc Surg 32: 969-976.
- Danielsson G, Arfvidsson B, Eklof B, Kistner RL, Masuda EM, et al. (2004) Reflux from thigh to calf, the major pathology in chronic venous ulcer disease: Surgery indicated in the majority of patients. Vasc Endovasc Surg 38: 209-219.
- O’Donnell TF (1988) Chronic venous insufficiency: An overview of epidemiology, classification, and anatomic considerations. Semin Vasc Surg 1: 60-65.
- Neglén P, Thrasher TL, Raju S (2003) Venous outflow obstruction: An underestimated contributor to chronic venous disease. J Vasc Surg 38: 879-885.
- Eklöf B1, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, et al. (2004) Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg 40: 1248-1252.
- van Bemmelen PS, Bedford G, Beach K, Strandness DE (1989) Quantitative segmental evaluation of venous valvular reflux with duplex ultrasound scanning. J Vasc Surg;10: 0425-0431.
- Hockenberry-Eaton M, Wilson, D. Wong’s. 2009: Essentials of Pediatric Nursing, 8th edn. St. Louis: Mosby
- Neglén P, Raju S (1993) A rational approach to detection of significant reflux with duplex Doppler scanning and air plethysmography. J Vasc Surg 17: 590-595.
- Sottiurai, VS (1996) Current surgical approaches to venous hypertension and valvular reflux. Int J Angiol 5: 49-54.
- Collins L and Seraj S (2010) Diagnosis and treatment of venous ulcers. Am Fam Physician 81: 989- 996.
- Perrin M (2000) Reconstructive surgery for deep venous reflux: A report on 144 cases. Cardiovasc Surg 8: 246-255.
- Maleti O, Perrin M (2011) Reconstructive surgery for Deep Vein Reflux in the Lower Limbs: Techniques, Results and Indications. Eur J Vasc Endovasc Surg 41: 837-848
- Meissner MH, Moneta G, Burnand K, Gloviczki P, Lohr JM, et al. (2007) The haemodynamics and diagnosis of venous disease. J Vasc Surg 46: S4-S24.
- Vasquez MA and Munschauer CE (2008) Venous clinical severity score and quality-of-life assessment tools: Application to vein practice. Phlebology 23: 259-275.
- Lane RJ, Cuzilla ML, McMahon CG (2003) Intermediate to long-term results of repairing incompetent multiple deep venous valves using external stenting. ANZ J Surg 73: 267-274.
- Tripathi R., Sieunarine K, Abbas M, Durrani N (2004) Deep venous valve reconstruction for non-healing leg ulcers: Techniques and results. ANZ J Surg, 74: 34-39
- Kistner KP, Steven M (1996) Die Leistungserstellung. Physica-Lehrbuch. Springer Science + Business Media pp. 53-130.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences