Surgical Treatment Strategies of Iatrogenic Giant Femoral Artery Pseudoaneurysms
Ahmed Mousa, Abdul Rahman S Al-Mulhim, Ahmed Audeh, Bayan Al-Ghadeer and Faisal Al-Khaldi
DOI10.21767/2573-4482.100037
Ahmed Mousa1,*, Abdul Rahman S Al-Mulhim2, Ahmed Audeh2, Bayan Al-Ghadeer3 and Faisal Al-Khaldi3
1Department of Vascular and Endovascular Surgery, Al-Azhar University School of Medicine, Al-Hussein University Hospital, Cairo, Egypt
2Department of General Surgery, King Faisal University, King Fahad Hospital Hofuf, Saudi Arabia
3College of Medicine, King Faisal University, Saudi Arabia
- *Corresponding Author:
- Ahmed Mousa
Department of Vascular and Endovascular Surgery College of Medicine
Al-Azhar University Al-Hussein University Hospital Cairo, Egypt
Tel:+966559904848
E-mail: isvascular@yahoo.com
Received date: January 15, 2017; Accepted date: February 02, 2017; Published date:February 02, 2017
Citation: Mousa A, Al-Mulhim ARS, Audeh A, et al. Surgical Treatment Strategies of Iatrogenic Giant Femoral Artery Pseudoaneurysms. J Vasc Endovasc Surg. 2017, 2:1. doi: 10.21767/2573-4482.100037
Abstract
Background: The aim of this study was to evaluate the technical and clinical results, following surgical treatment of iatrogenic giant femoral artery pseudoaneurysms.
Methods and findings: Among 1850 patients 60 (3.25%) of them diagnosed with an iatrogenic giant femoral artery pseudoaneurysms. All patients underwent surgical repair and were followed up for one month, three month and six month respectively using Duplex ultrasound sound and/or CT angiography. There were 40 male and 20 female, aged 30-70 years (Mean age 49.06 years ± 11.03). There were 66.7% n=40 patients presented with groin pain, pulsatile mass associated with lower extremity ischemia, infected pseudoaneurysm in 16.7% (n=10), pending ruptured pseudoaneurysm in 8.3% (n=5), and large wide pseudoaneurysm neck confirmed by Doppler ultrasound (8.3%) n=5. Primary repair was done for 30 patients; repair with vein batch angioplasty for 15 patients, interposition reversed saphenous vein graft for 10 patients, and interposition synthetic Dacron graft for 5 patients. Technical success was achieved in 100% of cases. There is neither limb loss nor intra-operative or postoperative mortality. Distal extremity ischemia was completely resolved after surgical repair. Postoperative complications included one groin wound infection, which was controlled by antibiotic treatment and debridement.
Conclusion: Open surgical repair of femoral pseudoaneurysms is technically feasible, first-line treatment for iatrogenic giant femoral artery pseudoaneurysmsassociated complications.
Keywords
Giant femoral artery; Pseudoaneurysm; Iatrogenic pseudoaneurysm; Surgical repair; Femoral pseudoaneurysms; Vein batch angioplasty; Interposition graft
Introduction
Femoral Artery Pseudoaneurysm (FAP) is one of the troublesome groin complications related to the femoral arterial access site used for invasive cardiovascular procedures [1]. Due to the increased number and complexity of endovascular interventions, the incidence of iatrogenic pseudoaneurysm formation has increased [2]. The femoral artery has been the initial access site of choice nearly for all intra-arterial procedures. However, access site complications of percutaneous procedures, such as bleeding, vessel thrombosis, emboli, dissection, and arteriovenous fistula, present significant clinical problems after catheterization procedures. FAP constitutes the most common of these complications, with a reported incidence of 0.2% to 2% [3]. The FAP form when an arterial puncture fails to close, allowing arterial blood to ooze into the surrounding tissue and create a pulsating hematoma [4]. Also it can present as a new thrill or bruit, or marked pain or tenderness. Complications of pseudoaneurysms include rupture, distal embolization, local pain, neuropathy and local skin ischemia [5]. Small asymptomatic pseudoaneurysms can be managed conservatively [6]. Management of femoral artery pseudoaneurysm has changed from surgical intervention to radiological intervention by transcatheter embolization using thrombin, direct percutaneous injection of thrombin, transcatheter fibrin adhesives and coils. Surgical interventions include aneurysmectomy and arterial repair. Surgical management is the only option left in failed radiological interventions or very large pseudoaneurysms [7].
Purpose
The aim of this study was to evaluate the technical and clinical results, following surgical treatment of iatrogenic giant femoral artery pseudoaneurysms.
Methods
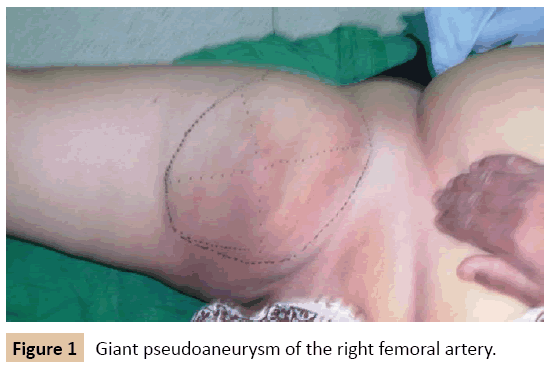
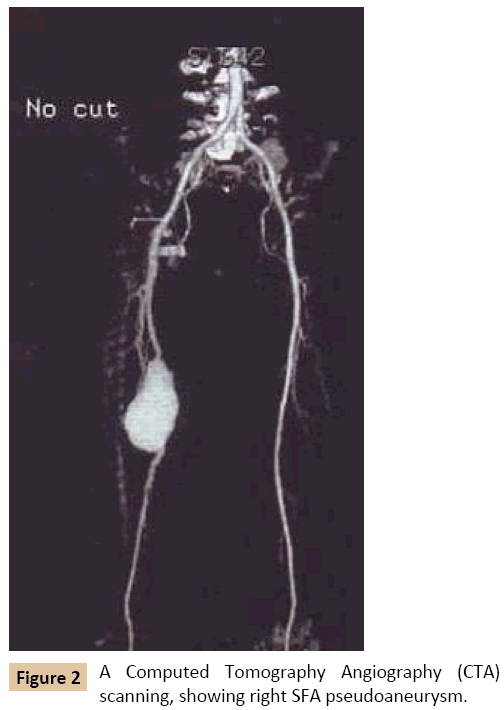
During the period from June 2006 to June 2016, data of 1850 patients, mapped for femoral artery puncture, underwent both percutaneous cardiac catheterization and peripheral vascular interventions were collected retrospectively from medical records. There were 60 patients who diagnosed with a giant FAP (Figure 1) that required surgical repair (n=60), 40 (66.7%) male and 20 (33.3%) female, aged 30-70 years (Mean age 49.06 years ± 11.03). Patients with FAP ≤ 12 cm and anastomotic site pseudoaneurysms were excluded from the study. All patients underwent surgical treatment and were followed up for one month, three month and six month respectively. The diagnosis of FAP was based on clinical examination as well as color flow duplex ultrasonography scanning and/or computed tomography angiography (CTA) scanning (Figure 2).
Technique of surgical repair
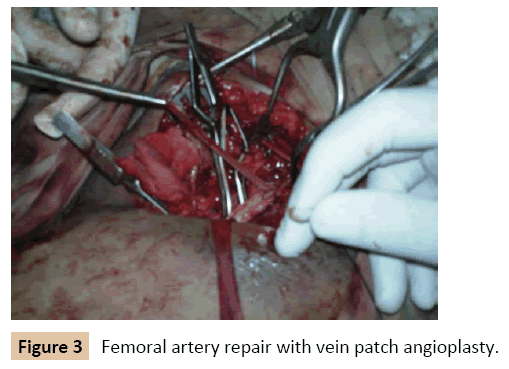
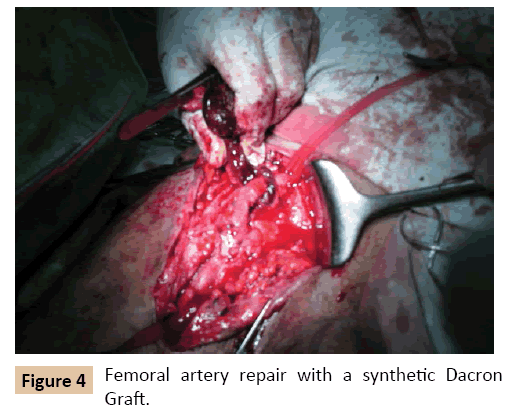
The patients were placed in the supine position. The character of the dorsalis pedis and posterior tibial pulses were documented prior to, during, and after the surgical procedure. A vertical incision was made along the whole length of the aneurysm which extended proximally and distally to provide proper exposure and control of the CFA, the SFA, and the PFA. The entire pseudoaneurysm pouch was accessed and huge haematoma was evacuated until reaching the arterial defect. The proximal part of the CFA and the distal part of the SFA and the PFA were freed with careful dissection, and nylon tapes were placed around them for vascular control after evacuation of the haematoma. After proper distal and proximal vascular control repair was done using 5-6/0 polypropylene suture. Primary repair was performed for 50% (n=30) in whom there was a small defect located in the anterior aspect of the femoral artery, repair with vein batch angioplasty (Figure 3) for 16.7% (n=10) patients, repair with interposition reversed saphenous vein graft for 16.7% n=10 patients, and repair with interposition synthetic Dacron graft for 16.7% n=10 patients (Figure 4). The indications for vein patch angioplasty and graft repair were arterial lacerations that are not suitable for primary repair. After the operation, all patients were given oral aspirin (antiplatelet agent) at a dose of 150 mg/day for 3 months. Clinical follow-up examinations were conducted at one month, three months and six month postoperatively, together with color flow Duplex ultrasonography scanning and/or CTA. Statistical analysis was performed using SPSS 16.0 for Windows program (SPSS Inc., Chicago, IL, USA).
Results
Among 1850 patients who underwent both percutaneous coronary intervention and peripheral vascular intervention through femoral access during a 10-year period at Al-Azhar University Hospitals, an iatrogenic giant femoral artery pseudoaneurysms were developed on 3.25% (n=60) patients. The time interval between the insult and diagnosis ranged from 1-4 weeks (Mean 16.20 ± 7.84 days). There were 40 (66.7%) male and 20 (33.3%) female, aged 30-70 years (Mean age 49.06 ± 11.03 years). There were 66.7% (n=40) patients presented with groin pain and pulsatile mass associated with manifestations of distal ischemia, infected pseudoaneurysm in 16.7% (n=10), pending ruptured pseudoaneurysm in 8.3% (n=5), and large wide pseudoaneurysm neck confirmed by Doppler ultrasound (8.3%) n=5. The pseudoaneurysm size ranged from 12-25 cm (Mean 17.60 ± 4.12 cm). Open surgical treatment was performed for all patients. Among the operated patients there were 50% (n=30) patients with SFA pseudoaneurysm, 41.7% (n=25) patients with CFA pseudoaneurysm, and 8.3% (n=5) patients with PFA pseudoaneurysm. The pseudoaneurysm size ranged from 12- 25 cm (Mean 17.60 ± 4.12 cm), and the duration of the clinical manifestations of the pseudoaneurysm until the time of surgery ranged from 1-4 weeks (Mean 16.20 ± 7.84 days), at the time of surgical intervention. Primary repair was performed for 50% (n=30) in whom there was a small defect located in the anterior aspect of the artery, repair with vein batch angioplasty for 16.7% (n=10) patients, repair with interposition reversed saphenous vein graft for 16.7% (n=10) patients, and repair with interposition synthetic Dacron graft for 16.7% (n=10) patients. Technical success was achieved in 100% (n=60) of cases without technical difficulties and without any complications. There is no limb loss occurred. There is no intra-operative or postoperative mortality. Distal extremity ischemia was completely resolved after surgical repair. Postoperative complications included one groin wound infection, which was controlled by systemic antibiotic treatment and early drainage. Follow-up after one month, three months and, six month revealed successful surgical repair with no clinical, sonographic or CTA complications and there were no changes in the postoperative distal pulses and color flow Duplex ultrasonography confirmed that the interposition grafts were patent.
Discussion
Femoral Artery Pseudoaneurysms (FAPs) occur in approximately 2% of cases following percutaneous-based procedures. Pseudoaneurysms result from insufficient sealing of the arterial puncture site, resulting in bleeding into the groin, resulting in the formation of haematoma [8], and it’s being surrounded by a pseudo capsule [9]. Various studies have reported the frequency of pseudoaneurysms following diagnostic or therapeutic percutaneous interventions to be between 0.2% and 6% [9]; the incidence has increased dramatically in recent years and is estimated at 0.9% for diagnostic procedures; it may increase to 9% or more for therapeutic procedures [3]. Among 1850 femoral interventions the incidence for development of femoral artery pseudoaneurysm was 3.25%. There is a good technical success without any complications and there is no reported case of amputation. Pseudoaneurysms mostly occur in the superficial femoral artery, they may also be encountered in the deep femoral artery, at the junction points of deep and superficial femoral arteries, and in the common femoral artery. Since the femoral artery is the most commonly used location for intervention, pseudoaneurysms of the femoral artery are more frequently encountered than pseudoaneurysms of the brachial and radial arteries [9]. Stable pseudoaneurysms are considered benign and can resolve spontaneously. Despites conservative treatment, up to 14% of pseudoaneurysms may require open repair [10]. As a result many surgeons treat small postcatheterization pseudoaneurysms (PCPAs conservatively as it undergoes spontaneous thrombosis over time. However, this may involve a prolonged hospital stay, delayed ambulation, and repeated sonographic monitoring to assess for thrombosis. However Toursarkissian et al. [11] monitored 82 patients with PCPAs less than 3 cm in diameter with duplex US and found that 72 of the lesions (87%) spontaneously thrombosed at a mean of 23 days (range, 1-125 d). Kent et al. [12] found spontaneous thrombosis unusual in PCPAs larger than 6 mL or 1.8 cm in diameter. The role of surgery has diminished since the development of lessinvasive methods of treatment of PCPAs. Despite this, there are still recognized indications for surgical repair including [11] large haematoma requiring surgical evacuation or suspected infected pseudoaneurysms [8] distal ischemia caused by local pressure by the pseudoaneurysm on the femoral artery, neuropathy caused by local pressure on the femoral nerve, failure of percutaneous treatment, ischemic soft tissue and skin caused by local pressure [11]. The most recent report by Garcia et al. [13] in 79 patients exemplified why surgical repair is discouraged unless absolutely necessary. A groin incision is generally safe and effective [14]. In Fellmeth et al. [15] described the successful non-surgical closure of 35 iatrogenic femoral pseudoaneurysm with ultrasound-guided compression repair in patients undergoing catheterization [16]. Another method of treating FAP was percutaneous thrombin injection which was first described by Cope and Zeit [17]. Current practice typically involves percutaneous thrombin injection with ultrasound visualization of the needle tip within the FAP [18,19]. Less invasive treatment option such as Duplex ultrasound-guided compression is available; however, evidence of its efficacy is limited. Patients with a pseudoaneurysm with a wide “neck” should be treated surgically. Surgery has traditionally been considered the 'gold standard' treatment, although it is not without risk in patients with severe cardiovascular disease. Surgical closure is needed in those patients whose pseudoaneurysm is enlarging, painful or remain patent. Our study demonstrates the efficacy of different types of surgical treatment of giant FAP complicating femoral cannulation. Our results in conjunction with the literature suggest a number of benefits of surgical treatment as a primary treatment option. The technical success was achieved in 100% of cases, there were very low complication rates as there is only a single case with groin infection which was treated properly and there were no intra-operative or postoperative mortality. So open surgical repair with different surgical vascular procedures was considered the first line approach in patients requiring active treatment, and is still preferred in many centers.
References
- Kassem HH, Elmahdy MF, Ewis EB, Mahdy SG (2015) Incidence and predictors of post-catheterization femoral artery pseudoaneurysms. The Egyptian Heart Journal 65:213-221.
- Lonn L, Olmarker A, Geterud K, Klingenstierna H, Delle M, et al. (2002) Treatment of femoral pseudoaneurysms. Percutaneous US-guided thrombin injection versus US-guided compression. ActaRadiologica 43: 396-400.
- Ates M, Sahin S, Konuralp C, Gullu U, Cimen S, et al. (2006) Evaluation of risk factors associated with femoral pseudoaneurysms after cardiac catheterization. J VascSurg 43:520-524.
- Marc-Alexander O, Maria-Anna S, Hubertus VK, Reginald W, Bernward L (2008) Percutaneous thrombin injection for treatment of iatrogenic femoral artery pseudoaneurysms: A case for caution. Angiology 59:372-375.
- Asgary S, Rafieian-KopaeiM, AdelniaA, KazemiS, ShamsiF (2010) Iatrogenic femoral artery pseudoaneurysm. ARAY Atheroscler J 6:74-77.
- ElMahdy MF, Kassem HH, Ewis EB, Mahdy SG (2014) Comparison between ultrasound-guided compression and paraaneurysmal saline injection in the treatment of postcatheterization femoral artery pseudoaneurysms. Am J Cardiol 113:871-876.
- Tiwary SK, Kumar S, Rahul K, Khanna AK (2007) Iatrogenic femoral artery aneurysms in orthopaedic practice. ANZ J Surg 77:899-901.
- Patrick AS, Campbell JE (2012) Complications related to femoral artery access for transcatheter procedures. VascEndovascSurg 46:617-623.
- Huseyin S, Yuksel V, Sivri N, Gur O, Gurkan S, et al. (2013) Surgical management of iatrogenic femoral artery pseudoaneurysms: A 10-year experience. Hippokratia17:332-336.
- Robert M, Anna-Maria B (2003) Current treatment method for postcatheterizationpseudoaneurysms. J VascIntervRadiol 14:697-710.
- Toursarkissian B, Allen BT, Petrinec DT (1997) Spontaneous closure of selected iatrogenic pseudoaneurysms and arteriovenous fistulae. J VascSurg 25:803-808.
- Kent KC, McArdle CR, Kenndy B(1993) A prospective study of the clinical outcome of femoral pseudoaneurysm and arteriovenous fistulas induced by arterial puncture. J VascSurg 17:125-133.
- Garcia San Norberto EM, Gonzalez-Fajardo JA, Gutierrez V, Carrera S, Vaquero C (2009) Femoralpseudoaneurysms post-cardiac catheterization surgically treated: evolution in progress. InteractCardiovascThoracSurg 8:353-357.
- Patrick AS, Campbell JE, AbuRahma AF (2014) Femoralpseudoaneurysms after percutaneous access. J VascSurg 60:1359-1366.
- Fellmeth BD, Roberts AC, Bookstein JJ(1910) Postangiographic femoral artery injuries: non-surgical repair with US-guided compression. Radiology 178:671-675.
- Chatterjee T, Do DD, Mahler F, Meier B (1998) Pseudoaneurysm of femoral artery after catheterization: treatment by a mechanical compression device guided by colour Doppler ultrasound. Heart 79:502-504.
- Cope C, Zeit R (1986) Coagulation of aneurysms by direct percutaneous thrombin injection. AJR 147: 383-387.
- Mittleider D, Cicuto K, Dykes T (2008) Percutaneous thrombin injection of a femoral artery pseudoaneurysm with simultaneous venous balloon occlusion of a communicating arteriovenous fistula. CardiovascInterventRadiol 31: S115-S119.
- Yetkin U, Ozelci A, Akyuz M, Goktogan T, Yurekli I, et al. (2009) Surgical Approach To A Giant Post Cardiac Catheterization Pseudoaneurysm After Unsuccessful Duplex Ultrasound-Guided Compression. Int J Cardiol 8:1-6.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences