The Impact of Post-Implantation Syndrome
Benyakorn T
DOI10.21767/2573-4482.18.03.16
1Division of Vascular Surgery, Department of Surgery, Thammasat University Hospital, Pathum Thani, Thailand
2Department of Vascular Surgery, UW Medicine, University of Washington, Seattle, Washington, USA
- *Corresponding Author:
- Thoetphum Benyakorn
Division of Vascular Surgery
Department of Surgery
Faculty of Medicine
Thammasat University
Pathum Thani, Thailand
Tel: +66 2-926-9523
E-mail: tbenya@uw.edu
Received Date: September 20, 2018; Accepted Date: September 21, 2018; Published Date: September 28, 2018
Citation: Benyakorn T (2018). The Impact of Post-implantation Syndrome. J Vasc Endovasc Therapy. 3:16.
Editorial
For more than forty years, starting in 1951, open repair of the abdominal aortic aneurysm (AAA) was the gold standard treatment. In 1990, the renowned Juan Parodi-Vascular surgeon from Buenos Aires, Argentina- introduced a minimally invasive operation called endovascular aneurysm repair (EVAR) [1]. Currently, EVAR is the new gold standard for AAA treatment. EVAR has provided advantages over open repair such as: Less operative blood loss; shortened operative time; shortened hospital stay; and reduced recovery time.
Three large randomized controlled trials showed the early survival advantages of EVAR [2-4]. Presently there is an exponential increase of the EVAR procedure all over the world. However, many recent publications suggest that EVAR has a decrease in long-term benefits [5,6]. Even though the evolution of general healthcare has greatly improved, the five-year survival of EVAR patients remain poor [7]. When compared to open repair long term survival of EVAR has worsened in older patients and in cases of large aneurysm diameter [8,9].
Does the Inflammatory Response Play a Role in Long-Term Survival?
Interleukin-6 (IL-6) is known as a key cytokine of the inflammatory process. IL-6 is secreted from inflammatory tissue and also directly from aneurysms [10]. IL-6 was detected immediately after vascular injury and reached a peak level at 24-h post-operatively. One study demonstrated that the higher concentration of IL-6 in the post-operative period results in leukocytosis and a longer hospital stay [11]. In addition, high levels of IL-6 can affect 30-day mortality and long term survival rate. Dawson and colleagues also found there was a correlation between a high level of IL-6 in the post-operative period and long-term cardiovascular risk [12]. The rapid increase of inflammatory mediators in the circulation is known as post-implantation syndrome (PIS).
PIS can occur immediately after stent graft placement with the incidence of PIS varying between 14% to 60% [13-18]. In most cases, PIS is well tolerated, but in some particular cases it may contribute to severe complications, including renal function impairment, cardiovascular events, and multiple organ failure during the post-operative period [19].
The combination of leukocytosis, fever and an elevation in high-sensitivity C-reactive protein (hs-CRP) has been widely used for diagnosis of PIS [14,15], there is no evidence to clearly define the etiology of PIS [20,21]. Many factors have been suspected and proposed, such as, stent graft component, contrast medium-induced neutrophil degradation, bacteria translocation from transient sigmoid ischemia, endothelium injury in the implantation process, reaction of mural thrombus, thrombosis on the previous aneurysm sac, and volume of new-onset thrombus [17,22-27].
Can Any Device Minimize the PIS Effect?
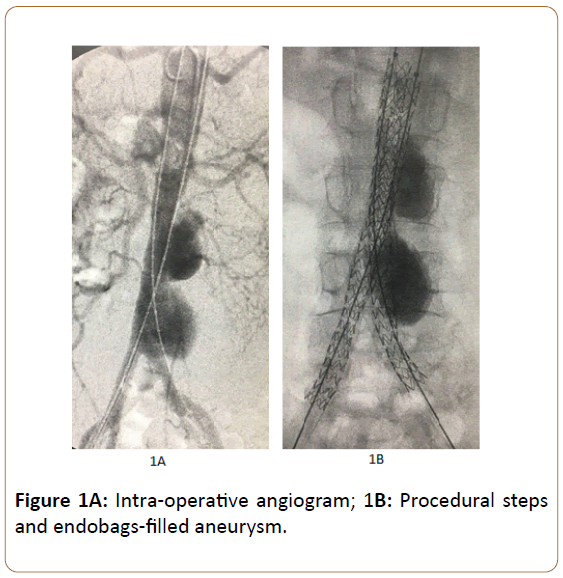
Endovascular aneurysm sealing system (EVAS), the unique design for sealing the entire aneurysm sac in the active sac management, is completely different from traditional endovascular devices. The Nellix device (Endologix Inc., Irvine, Calif) consists of a 10 mm ballon-expandable stent graft covered by double layer polymer-filled endobag. The expanding endobags completely seal the entire aneurysm and separate the aneurysm sac from the systemic circulation (Figures 1A and 1B). This mechanism may prevent or decrease biochemical reaction within the aneurysm sac. This results in a reduced release of inflammatory mediators compared with omnipresent endovascular devices. A recent study showed that the incidence of PIS is lower in EVAS compared to EVAR (5.1% vs 20.5%, p=0.07). In addition, mean leukocyte count (p=0.003), mean body temperature (p=0.05), and mean hs-CRP (p<0.001) were relatively lower within the EVAS cohort. This evidence suggests that EVAS is associated with a blunted systematic inflammatory response when compared to EVAR [28].
In conclusion, PIS is not a rare clinical entity and may contribute to severe complications. Although the etiology of PIS is not clearly defined, a preventive effort to reduce any inflammation should be attempted. EVAS, as a new innovative device is now clinically proven to decrease the incidence of PIS. Future research in reducing PIS is crucial.
Acknowledgement
The author kindly thanks Marina S. Ferguson-Department of Radiology, University of Washington-for adjusting the language to this article.
References
- Parodi JC, Palmaz JC, Barone HD (1991) Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 5: 491-499.
- Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG (2004) The EVAR trial participants. Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (EVAR trial 1), 30-day operative mortality results: randomised controlled trial. Lancet 364: 843-848.
- Prinssen M, Verhoeven EL, Buth J, Cuypers PW, Balm R, et al. (2004) A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med 351: 1607-1618.
- Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Kohler TR, et al. (2009) Outcomes following endovascular vs open repair of abdominal aortic aneurysm: a randomized trial. JAMA 302: 1535-1542.
- Patel R, Sweeting MJ, Powell JT, Greenhalgh RM, the EVAR trial investigators (2016) Endovascular versus open repair of abdominal aortic aneurysm in 15-years’ follow-up of the UK endovascular aneurysm repair trial 1 (EVAR trial 1): a randomised controlled trial, Lancet 388: 2366-2374.
- Schermerhorn ML, Buck DB, O’Malley AJ, Curran T, Darling J, et al. (2015) Long-term outcomes of abdominal aortic aneurysm in the medicare population. N Engl J Med 373: 328-338.
- Bahia SS, Holt PJ, Jackson D, Patterson BO, Thompson MM, et al. (2015) Systematic review and meta-analysis of long-term survival after elective infrarenal abdominal aortic aneurysm repair 1969-2011: 5 Year survival remains poor despite advances in medical care and treatment strategies. Eur J Vasc Endovasc Surg 50: 320-330.
- Khashram M, Hider PN, Williman JA, Jones GT, Roake JA (2016) Does the diameter of abdominal aortic aneurysm influence late survival following abdominal aortic aneurysm repair? A systematic review and meta-analysis.Vascular 24: 658-667.
- Huang Y, Gloviczki P, Duncan AA, Kalra M, Fleming MD, et al. (2017) Maximal aortic diameter affects outcome after endovascular repair of abdominal aortic aneurysms. J vasc Surg 65: 1313-1322.
- Dawson JA, Cockerill GW, Choke E, Belli AM, Loftus I, et al. (2007) Aortic aneurysms secrete interleukin-6 into the circulation. J Vasc Surg 45: 350-356.
- Dela Motte L, Kehlet H, Vogt K, Nielsen CH, Groenvall JB, et al. (2014) Preoperative methylprednisolone enhances recovery after endovascular aortic repair a randomized, double-blind, placebo-controlled clinical trial. Ann Surg 260: 540-549.
- Dawson JA, Choke E, Cockerill GW, Loftus IM, Thompson MM (2009) The long-term effects of open and endovascular aneurysm repair on circulating interleukin-6. Eur J Vasc Endovasc Surg 37: 43-45.
- Arnaoutoglou E, Kouvelos G, Milionis H, Mavridis A, Kolaitis N, et al. (2011) Post- implantation syndrome following endovascular abdominal aortic aneurysm repair: Preliminary data. Interact Cardiovasc Thorac Surg 12: 609-614.
- De La Motte L, Vogt K, Panduro Jensen L, Groenvall J, Kehlet H, et al. (2011) Incidence of systemic inflammatory response syndrome after endovascular aortic repair. J Cardiovasc Surg (Torino) 52: 73-79.
- Voute MT, Bastos Goncalves FM, Klein Nulent CG, Hoeks SE, et al. (2012) Stent graft composition plays a material role in the post- implantation syndrome. J Vasc Surg; 56: 1503-1509.
- Moulakakis KG, Alepaki M, Sfyroeras GS, Koulouras V, Milionis H, et al. (2013) The impact of endograft type on inflammatory response after endovascular treatment of abdominal aortic aneurysm. J Vasc Surg. 57: 668-677.
- Sartipy F, Lindstrom D, Gillgren P, Ternhag A (2015) The impact of stent graft material on the inflammatory response after EVAR. Vasc Endovascular Surg 49: 79-83.
- Arnaoutoglou E, Kouvelos G, Papa N, Kallinteri A, Milionis H, et al. (2015) Prospective evaluation of post-implantation inflammatory response after EVAR for AAA: influence on patients’ 30 day outcome. Eur J Vasc Endovasc Surg 49:175-183.
- Arnaoutoglou E, Papas N, Milionis H, Kouvelos G, Koulouras V, et al. (2010) Post-implantation syndrome after endovascular repair of aortic aneurysms: need for post discharge surveillance. Interact Cardiovasc Thorac Surg 11: 449-454.
- Blum U, Voshage G, Lammer J, Beyersdorf F, Töllner D, et al. (1997) Endoluminal stent-grafts for infrarenal abdominal aortic aneurysms. N Engl J Med 336: 13-20.
- Görich J, Rilinger N, Söldner J, Krämer S, Orend KH, et al. (1999) Endovascular repair of aortic aneurysms: treatment of complications. J Endovasc Surg 6: 136-146.
- Storck M, Scharrer-Pamler R, Kapfer X, Gallmeier U, Görich J, et al. (2001) Does a postimplantation syndrome following endovascular treatment of aortic aneurysms exist? Vasc Surg 35: 23-29.
- Galle C, Motte S, Zhou L, Stordeur P, Delville JP, et al. (2000) Early inflammatory response after elective abdominal aortic aneurysm repair: a comparison between endovascular procedure and conventional surgery. J Vasc Surg 32: 234-246.
- Chang CK, Chuter TA, Niemann CU, Shlipak MG, Cohen MJ, et al. (2009) Systemic inflammation, coagulopathy, and acute renal insufficiency following endovascular thoracoabdominal aortic aneurysm repair. J Vasc Surg 49: 1140-1146.
- Akin I, Nienaber CA, Kische S, Rehders TC, Ortak J, et al. (2009) Effect of antibiotic treatment in patients with postimplantation syndrome after aortic stent placement. Rev Esp Cardiol 62: 1365-1372.
- John DK, Konstantinos GM, Constantine NA, Spyridon NM, Triantafillos GG, et al. (2014) Volume of new-onset thrombus is associated with the development of postimplantation syndrome after endovascular aneurysm repair. J Vasc Surg 60: 1140-1145.
- Lee JH, Choi JH, Kim EJ (2018) Volume of mural thrombus plays a role in the elevation of inflammatory markers after endovascular aortic repair. J Cardiothorac Surg 13: 27.
- Berg P, Stroetges RA, Miller LE, Schoefferle J (2017) A propensity score–matched analysis of inflammatory response with endovascular aneurysm sealing vs endovascular aneurysm repair. J Endovasc Ther 24: 670-674.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences