The Predictive Value of The Core-Muscle Index Regarding Type II Endoleaks After Endovascular Repair of Abdominal Aortic Aneurysm (EVAR)
Gottfried Mommertz
DOI10.21767/2573-4482.100013
1Department of Anaesthesiology and operative intensive care Medicine, Marienhospital Aachen, Germany
2Department of Vascular and Endovascular Surgery, Marienhospital Aachen, Germany
- *Corresponding Author:
- Gottfried Mommertz
Gottfried Mommertz, Department of Vascular and Endovascular Surgery, Zeise 4, 52066 Aachen, Germany
Tel: 00492411301
E-mail: Gottfried.Mommertz@marienhospital. de
Received date: June 20, 2016; Accepted date: June 23, 2016; Published date: June 28, 2016
Citation: Goldacker K, Hansen J, Möllhoff T, et al. The Predictive Value of The Core-Muscle Index Regarding Type II Endoleaks After Endovascular Repair of Abdominal Aortic Aneurysm (EVAR). Journal of Vascular & Endo Surgery. 2016, 1:3. doi: 10.21767/2573-4482.100013
Abstract
Objective: The presently favoured technique of endovascular repair of abdominal aortic aneurysms (EVAR) can fail to fully eliminate the aneurysm when an endoleak occurs. The most common endoleak, type II, is caused by retrograde perfusion of the aneurysmal sac through mesenteric or lumbar arteries. Our hypothesis is that the patency and number of lumbar arteries and thus, the formation of type II endoleaks, can be predicted preoperatively by morphometrically measuring the total psoas area or core muscle index.
Methods: The medical records of all EVAR patients treated at the Marienhospital Aachen between July 2013 und August 2015 were reviewed retrospectively with a special focus on the postoperative formation of endoleaks. In the preoperative CT-scans of the population we morphometrically measured the total psoas area and density. The effect of total psoas area on occurance of endoleaks was assessed using Wilcoxon-signed-rank-test.
Results: 63 patients with a mean age of 72.5 years were treated with EVAR for AAA. There was an endoleak type II occurrence rate of 21.9%. The mean total psoas area was 2412.30 mm². The Wilcoxon-signed-rank-test showed no significant association between the mean total psoas area or density and the occurrence of endoleaks.
Conclusions: In the end we could not demonstrate that core muscle index could be a predictor for endoleak type II. One of the reasons we failed is perhaps the small size of the cohort. We are planning to continue pursuing our hypothesis by appending our data with that of other centers to include a larger number of individuals.
Introduction
Abdominal aortic aneurysm is a threat steadily gaining importance as our population ages. Approximately 5 % of males aged 65 years and older are affected. Aside from open abdominal aneurysm repair, which has been performed since the 1950s, an endovascular procedure has also been successfully implemented since 1990. EVAR, first described by Parodi et al. [1], is now steadily becoming the favoured operative method, with lower mortality and complication rates in both elective and emergent cases [2,3].
Endoleaks are a common complication following EVARprocedures. Persistant bloodflow into the space between the stentgraft and the aneurysm sac causes a further growth of the aneurysm. Endoleaks are categorized according to localization of the leak and their threat of rupture – type I: leak at graft attachment site (Ia: proximal, Ib: distal, Ic: iliac occluder); type II: aneurysm sac filling via branch vessel (most common) (IIa: single vessel, IIb: two vessels or more); type III: leak through defect in graft (IIIa: junctional separation of the modular components, IIIb: fractures or holes involving the endograft); type IV: leak through graft fabric as a result of graft porosity and type V: continued expansion of aneurysm sac without demonstrable leak on imaging [4].
Whilst type I and III endoleaks, largely origining in failure of device, measurement or technique are generally treated immediately, type II endoleaks are often treated more conservatively [5]. Some authors even advocate against early treatment, since spontaneous sealing of type II endoleaks has been reported to occur within the first 6 months in as many as 53% of all endoleaks [6-9]. In an extensive retrospective study in 2013, Löwenthal ets al. analysed potential predictive CT-angiographic parameters in the development of high-risk type 2 endoleaks after endovascular aneurysm repair. They identified the number and diameter of lumbar arteries perfusing the AAA to be the most important predictive factor [10].
Core muscle size, or total psoas area (TPA), is an objective means used mainly to assess patient frailty by morphometrically determining psoas muscle mass by the cross-sectional area in CT scans.
Our hypothesis is that patients with a larger core muscle size, whilst less “frail” and thus less at risk regarding perioperative complications, are more likely to develop type 2 endoleaks due to larger lumbar arteries perfusing the psoas muscles. A measurement of TPA in a pre-operative CT scan could thus be a readily available means of predicting possible candidates at risk for type 2 endoleaks, and allow for pre-interventional embolization of aortic side branches to counteract the development of endoleaks.
The measurement of core muscle index is furthermore well suited for our study cohort as morphometric measures of muscle size and density were readily obtainable from the pre-operative CT angiographies used to assess anatomy and pathology in planning the endovascular aortic repair.
Methods
In a single center retrospective study, the medical records of all adult patients suffering from AAA who underwent elective EVAR in our center between July 2013 und August 2015 were reviewed. Patients lacking pre- or postoperative CT-scans were excluded. Amongst these, 63 had a preoperative abdominal CT scan of suitable quality for morphometrical analysis. This population comprised our study cohort.
Patient demographics, comorbidities and postoperative outcome, especially regarding occurance of endoleaks, were reviewed.
A single observer morphometrically measured cross-sectional areas and densities of left and right psoas muscle at the level of the forth lumbar (L4) vertebra by selecting the CT imaging slice at the superior aspect of L4 and outlining both psoas muscle borders. The areas thus enclosed were then summed to render the TPA. Within the outlined reagions, average muscle density in Houndsfield units was also measured.
Results
Table 1 shows the basic descriptive data of our population – in 63 total patients, 55 were male, 8 female, the mean age at intervention was 72.5 ± 8.6 years. The mean BMI was 27.4 kg/ cm2 ± 4.2 kg/cm2.
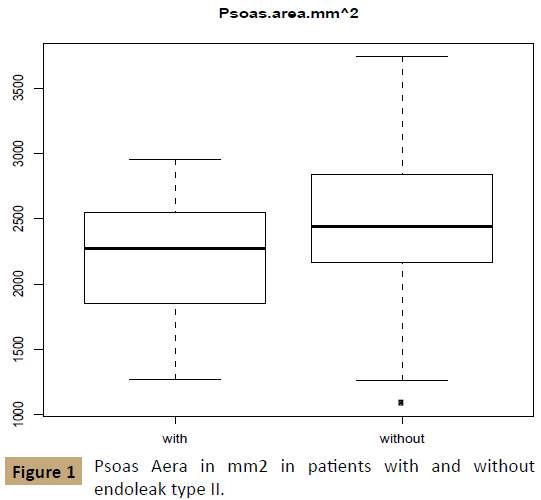
Mean TPA, defined as the sum of right side and left side psoas area at L4-level, was 2412.3 ± 556.4 mm2.
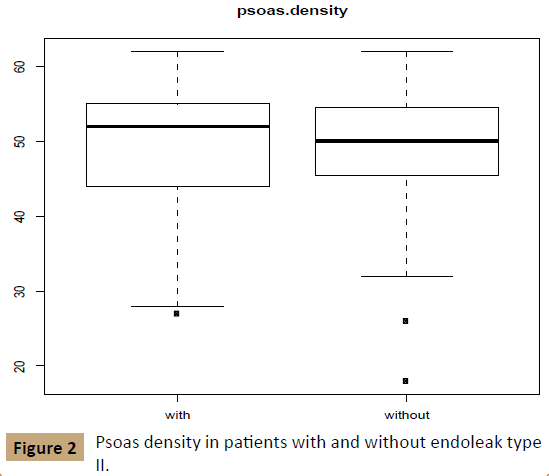
Mean average psoas density (APD), measured in Hounsfield units, was 48.2 ± 9.2.
Of all patients, 14 developed endoleaks type II. This equals a percentage of 21.9% for type II endoleaks occurrence.
In those patients that developed endoleaks following the EVARprocedure, the mean age at intervention was 74.6 ± 8.0 years. The mean BMI was 25.8 kg/cm2 ± 3.6 kg/cm2
Mean TPA in endoleak patients was 2250.8 ± 562.2 mm2, mean APD, measured in Hounsfield units, was 47.5 ± 10.9 (Table 1).
| number of Patients | 63,00 |
|---|---|
| number of type II endoleaks | 14,00 |
| Median psoas area | 2412,30 |
| SD for total psoas area | 556,37 |
| median psoas density | 48,17 |
| SD for psoas density | 9,23 |
| psoas median in endoleak patients | 2250,80 |
| SD for total psoas area in endoleak patients | 562,19 |
| Psoas density median in endoleak patients | 47,53 |
| SD for psoas density in endoleak patients | 10,91 |
Table 1: Data of patients with and without endoleak type II.
We used the Wilcoxon-signed-rank test to determine whether either TPA or APD significantly correlated with the occurrence of type 2 endoleaks setting the significance level at p=0,05. We found the correlation between neither TPA (p=0,319) nor APD (p=0,62) to be statistically significant, therefore negating our hypothesis (Figures 1 and 2).
Conclusion
There is no significant correlation between TPA or APD and the occurrence of type 2 endoleaks in our study cohort. Thus, core muscle index could not be proven to be a suitable predictor for the formation of endoleaks.
One of the reasons we failed is perhaps is the small size of the cohort, therefore we are planning to continue pursuing our hypothesis by appending our data with that of other centers to include a larger number of individuals.
Should we succeed to prove TPA or APD to indeed serve as a predictive factor for endoleak occurrence, this would provide us with a readily obtainable prognostic tool to allow for preoperative measures such as embolization of lumbar arteries to be taken in order to prevent endoleaks.
References
- Parodi JC, Palmaz JC, Barone HD (1991) Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg 5:491-499.
- Thomas DM, Hulten EA, Ellis ST(2014) Open versus Endovascular Repair of Abdominal Aortic Aneurysm in the Elective and Emergent Setting in a Pooled Population of 37,781 Patients: A Systematic Review and Meta-Analysis. ISRN Cardiology.
- Schermerhorn ML, O'Malley AJ, Jhaveri A, Cotterill P, Pomposelli F (2008) Landon BE. Endovascular vs. Open Repair of Abdominal Aortic Aneurysms in the Medicare Population. N Engl J Med 358:464-474.
- Bashir MR, Ferral H, Jacobs C, McCarthy W, Goldin M (2009) Endoleaks After Endovascular Abdominal Aortic Aneurysm Repair: Management Strategies According to CT Findings. American Journal of Roentgenology 192: W178-W186.
- White SB, Stavropoulos SW (2009) Management of Endoleaks Following Endovascular Repair. SeminIntervent Radiol 26:33-38.
- Tuerff SN, Rockman CB, Lamparello PJ, Adelman MA, Jacobowitz GR, et al. (2002) Are type II (branch vessel) endoleaks really benign? Ann Vasc Surg 16:50-54.
- Maldonado TS, Gagne PJ (2003) Controversies in the management of type II “branch” endoleaks following endovascular abdominal aortic aneurysm repair. Vasc Endovasc Surg 37:1-12.
- Moore WS, Rutherford RB (1996) Transfemoral endovascular repair of abdominal aortic aneurysm: results of the North American EVT phase 1 trial. Jvasc Surg 23:543-553.
- Silverberg D, Baril DT, Ellozy SH, (2006)An 8-year experience with type II endoleaks: natural history suggests selective intervention is a safe aproach. J Vasc Surg 44:453-459.
- Löwenthal D, Herzog L, Rogits B (2015) Identification of Predictive CT Angiographic Factors in the Development of High-Risk Type 2 Endoleaks after Endovascular Aneurysm Repair in Patients with Infrarenal Aortic Aneurysms. Fortschr Röntgenstr 187: 49-55.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences