Total Abdominal Aortic Stent Graft Occlusion
Paulo Eduardo Ocke Reis, Marcello Rotolo, Alessandra Viz Veiga, Jean Moura Netto, Vitor Nascimento Maia, Lys Nunes dos Santos, Irlandia Figueira Ocke Reis, Fernando Azambuja Fontes, Thadeu Mozella, Gustavo Solano, Daniel Paixao, Luciana Cristina Ximenes, Amanda Barata Reis and Pietro de Almeida Sandri
DOI10.21767/2573-4482.100070
1Department of Specialized and General Surgery, Fluminense Federal University, Rio de Janeiro, Brazil
2Vascular Clinic Ocke Reis, Rio de Janeiro, Brazil
- *Corresponding Author:
- Paulo Eduardo Ocke Reis
Department of Specialized and General Surgery
Fluminense Federal University
Rio de Janeiro, Brazil.
Tel: +55 21 2629-5000
E-mail: vascular@pauloocke.com.br
Received date: December 24, 2017; Accepted date: December 29, 2017; Published date: December 30, 2017
Citation: Reis PEO, Rotolo M, Veiga AV, Netto JM, Maia VN, et al. (2017) Total Abdominal Aortic Stent Graft Occlusion. J Vasc Endovasc Surg. 2:37. doi: 10.21767/2573-4482.100070
Abstract
We report a case involving an acute chronic endovascular abdominal aortic stent graft occlusion in which percutaneous angioplasty was performed via bilateral trans femoral approach. This case emphasized that endograft occlusion treatment after endovascular aortic aneurysm repair (EVAR) is feasible.
Keywords
Endovascular aneurysm repair; Abdominal aortic aneurysm; Endograft; Thrombosis
Introduction
The endovascular treatment of abdominal aortic aneurysm when compared to conventional treatment is less invasive and presenting lower morbidity, mortality, especially in patients with high anesthetic-surgical risk [1-3]. Among the complications described in the medium and long term after the treatment are the thromboembolic events associated with the stent graft occlusion, generally graft limb occlusion [3,4]. Furthermore, follow-up after surgery is necessary to decrease the risk of death or associated comorbidities [3]. We present a case of total occlusion of the endograft after long-term aortic aneurism repair.
Case Report
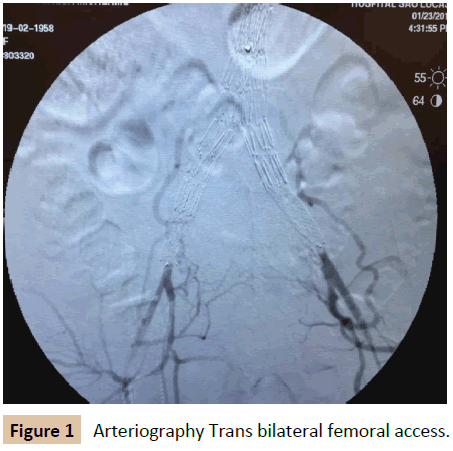
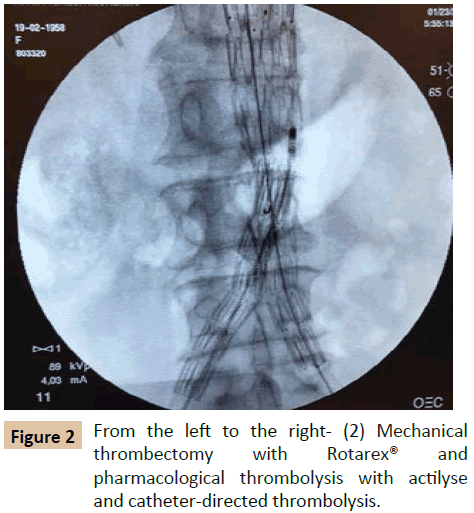
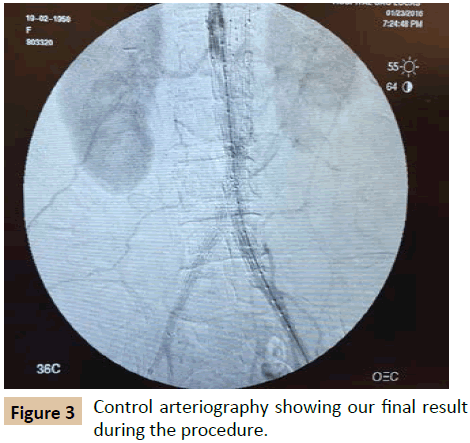
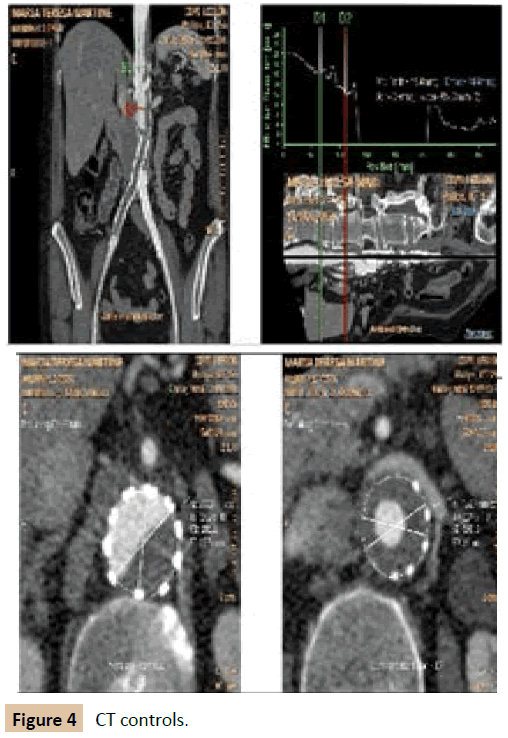
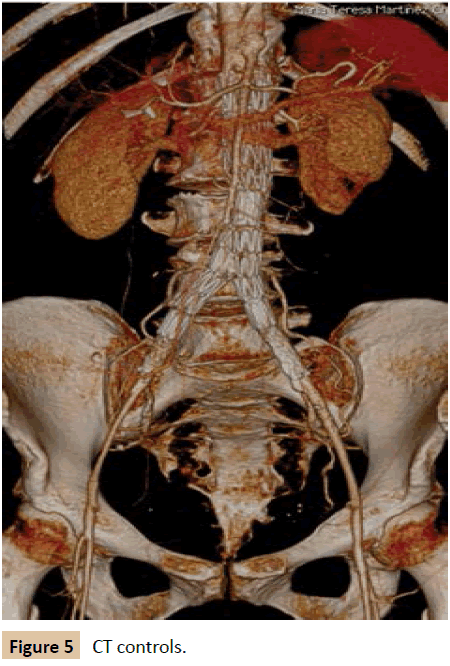
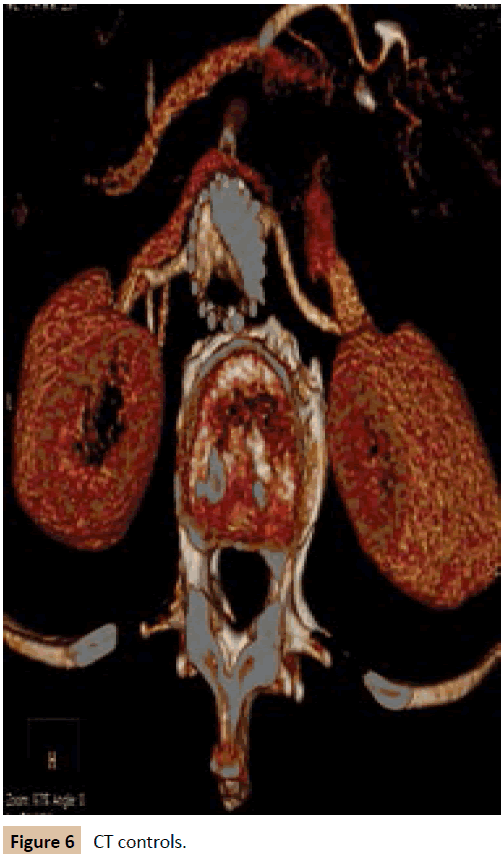
A 59-year-old female patient smoker and with systemic hypertension was admitted in the emergency room with pain and paraesthesia in both legs, absence of pulses in the lower limbs, with a history of aortic aneurysm repair of the abdominal aorta by endovascular technique in 2009 with another team. In the suspicion of aorto-iliac occlusion we requested a computerized angio tomography and it was identified an aortic stent graft occlusion. We performed arteriography trans bilateral femoral access (Figure 1) and after mechanical thrombectomy with Rotarex® and pharmacological thrombolysis with actilyse, 30 mcg, all long the procedure, diluted, during three hours with catheter-directed thrombolysis followed by prolonged balloon inflation (Figure 2), the final arteriography revealed a better final image but not as we would wish (Figure 3). The patient was taken to the ICU and was discharged on the fourth postoperative day. Since then, she maintains clinical follow-up with improvement of paraesthesia, pain relief and presence of pulses in lower limbs and claudication for half distances. Angio TC control results (Figures 4-6) shows partial recanalization of Aortoilac segment. Although with clinical improving since than indication of intervention, in our opinion, neither the patient nor the family wants to perform another interventional procedure.
Discussion
Long-term surveillance indicates that approximately 20% of patients require additional procedures, most of by endovascular procedures [5-7]. Limb thrombosis after EVAR is a complication in which the incidence rates have been reported to be 2% to 25% [3-8]. Placement of a large limb in a shorter vessel, kinking [3] or the presence of angulation or calcifications of the iliac arteries appear to be predictors of endograft limb occlusion after EVAR [6]. And didn`t find statistical significance for occlusion rate between different endograft [5]. The mechanism of late limb occlusion should be related to migration or dislocation of an endograft and eventual endograft occlusion [5,9]. Mehta et al. reported that 7.4% of patients developed stent graft limb thrombosis, in 1768 cases, during a mean follow-up of 34 months [7]. Thrombosis in aortic Endoprosthesis seems to be a multifactorial process, especially local hemodynamic factors, which lead to a disturbance of the endothelial function, with repercussion on cell adhesiveness and increased viscosity. The increase blood viscosity in turn modifies the shear stress on the of the endograft wall, favoring formation of thrombus, however, the pathophysiology of these events has not yet been fully elucidated. Such findings are consistent with the case of the patient reported, since there was a history of significant smoking burden and irregular use of antiplatelet agents. In this way, the endovascular technique has established its bases, proving to be feasible and effective for the treatment of surgical vascular diseases, capable of offering safety and comfort with a minimally invasive approach, which is fundamentally important for patients with comorbidities and high surgical risk, however we need more randomized controlled trials to evaluate percutaneous angioplasty to treat an occluded endograft, if is a well-accepted tool. Endograft limb occlusion may be related to reduce outflow. Occlusion of the internal iliac artery or unrecognized distal dissection may increase the risk of limb thrombosis [10,11]. Acute endograft limb occlusion is manifested with claudication rather than with critical ischemia, provided the limb has been deployed proximal to the internal iliac artery, which facilitates collateral perfusion to the lower extremity.
Conclusion
In this way, endovascular procedures has established its bases, proving to be feasible and effective for the treatment of aortic endoprotesis occlusion, capable of offering safety and comfort with a minimally invasive approach, even as the treatment of its complications, which is fundamentally important for patients with critical comorbidities and high surgical risk.
References
- Greenhalgh RM, Brown LC, Kwong GP, Powell JT, Thompson SG (2004) Comparison of endovascular aneurysm repair with open repair in patients with abdominal aortic aneurysm (Evar trial 1), 30-day operative mortality results: randomized controlled trial. Lancet 364: 843-848.
- Prinssen M, Verhoeven EL, Buth J, Cuypers PW, van Sambeek MR, et al. (2004) A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med 351: 1607-1618.
- Chaikof EL, Dalman RL, Eskandari MK, Jackson BM, Lee A, et al. (2018) The Society for Vascular Surgery practice guidelines on the care of patients with an abdominal aortic aneurysm. J Vasc Sur 67: 2-77.
- Sampram ES, Karafa MT, Mascha EJ, Clair DG, Greenberg RK, et al. (2003) Nature, frequency, and predictors of secondary procedures after endovascular repair of abdominal aortic aneurysm. J Vasc Surg 37: 930-937.
- Tatli E, Tokatli A, Vatan MB, Aksoy M, Can Y, et al. (2016) Percutaneous approach to the treatment of a totally occluded abdominal aortic stent graft. Perfusion 31: 521-524.
- MantasGK, Antonopoulos CN, Sfyroeras GS, Moulakakis KG, Kakisis JD, et al. Factors Predisposing to Endograft Limb Occlusion after Endovascular Aortic Repair. Eur J Vasc Endovasc Surg 49: 39-44.
- Mehta M, Sternbach Y, Taggert JB, Kreienberg PB, Roddy SP, et al. (2010) Long-term outcomes of secondary procedures after endovascular aneurysm repair. J Vasc Surg 52: 1442-1449.
- Solonynko B, Galazka Z, Jakimowicz T, Szmidt J (2012) Influence of atheromatous lesions in the ilio-femoral segment on the occurrence of stent graft thrombosis after endovascular treatment of an abdominal aortic aneurysm. Pol Przegl Chir 84: 551-559.
- Maleux G, Koolen M, Heye S, Nevelsteen A (2008) Limb occlusion after endovascular repair of abdominal aortic aneurysms with supported endograft. J Vasc Interv Radiol 19: 1409-1412.
- Conway AM, Modarai B, Taylor PR, Carrell TW, Waltham M (2012) Stent-graft limb deployment in the external iliac artery increases the risk of limb occlusion following endovascular AAA repair. J Endovasc Ther 19: 79-85.
- Daoudal A, Cardon A, Verhoye JP, Clochard E, Lucas A, et al. (2016) Sealing zones have a greater influence than iliac anatomy on the occurrence of limb occlusion following endovascular aortic aneurysm repair. Vascular 24: 279-286.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences