Transarterial Embolization of a Pelvic Arteriovenous Malformation Using Squid-12
Guilherme de Palma Abrão, DaniloAlves de Araujo, Matheus Miranda Barbosa and Paulo Eduardo Ocke Reis
DOI10.36648/2634-7156.21.6.12
Guilherme de Palma Abrão1*, DaniloAlves de Araujo1, Matheus Miranda Barbosa1 and Paulo Eduardo Ocke Reis2
1Department of Radiology, Fluminense Federal University, Rio de Janeiro, Brazil
2Department of Specialized and General Surgery, Fluminense Federal University, Rio de Janeiro, Brazil
- *Corresponding Author:
- Guilherme de Palma Abrão
Department of Radiology, Fluminense Federal University, Rio de Janeiro, Brazil
Tel: +982679898
E-mail: guiabrao@yahoo.com.br
Received Date: February 21, 2021; Accepted Date: March 23, 2021; Published Date: March 30, 2021
Citation: Guilherme PA, Danilo AA, Matheus MB, Ocke Reis PE (2021) Transarterial Embolization of a Pelvic Arteriovenous Malformation Using Squid-12. J Vasc Endovasc Ther. 6 No. 3: 12.
Abstract
We describe a complex congenital pelvic arteriovenous malformation (AVM) with multiple feeding arteries arising from branches sides of the right internal iliac artery and a dominant draining vein in a male patient. Transarterial embolization was performed in a patient with a congenital pelvic AVM, using Squid® 12 (Balt Extrusion, Montmorency, France) composed of ethylene vinyl alcohol (EVOH) copolymer dissolved in dimethyl sulfoxide (DMSO) and micronized tantalum powder for radiopacity. The patient showed prompt resolution of the symptoms and complete occlusion of the AVM which was observed on the CT and angiography control exams.
Keywords
Pelvic arteriovenous malformation; Transarterial embolization; Liquid agents
Introduction
Pelvic AVM is a rare but extremely distressing condition representing only 1.8% of the major abdominal AVM localizations. Congenital pelvic arteriovenous malformation (AVM) is presumed to be a focal persistence of primitive and vascular channels [1-4]. Most pelvic lesions seem to have a particular angioarchitecture consisting of multiple small arteries and a single draining fistula [2,3]. Treatment, either open or endovascular, is challenging because of the anatomic characteristics, the deep location, and the high hemorrhagic and ischemic risks [1].
No guidelines are available for the endovascular treatment of pelvic AVM and previous reports have described many cases of embolization for feeding arteries. To embolise the nidus sufficiently, blood flow to the AVM should be controlled [2-5]. The use of liquid agents in the treatment of AVMs is increasing every day. There non-adhesive properties allow more effective treatments compared to cyanoacrylate [6].
Case Report
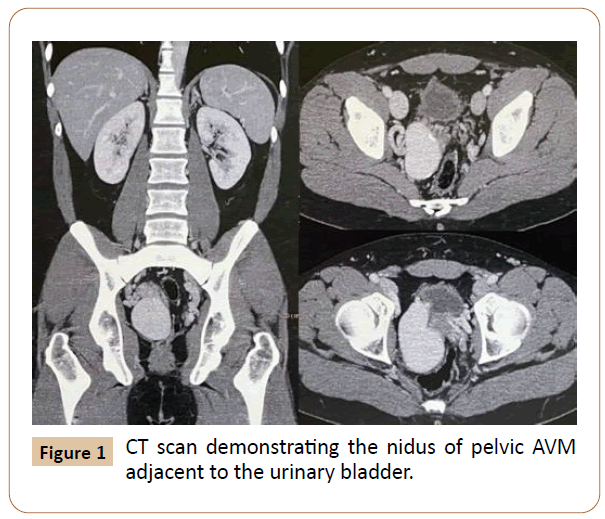
A 30-year-old man with no significant medical history presented with progressively increasing pelvic pain for 6 months. Computed tomography angiography (CTA) demonstrated a large pelvic AVM with multiple feeding arteries arising from the side branches of the right internal iliac artery especially from the anterior trunk, which were draining, into right internal iliac vein through a large venous pouch, which involved the wall of the urinary bladder (Figure 1). Because he had no history of pelvic trauma, neoplasm, or surgery we considered the AVM to be congenital anomaly.
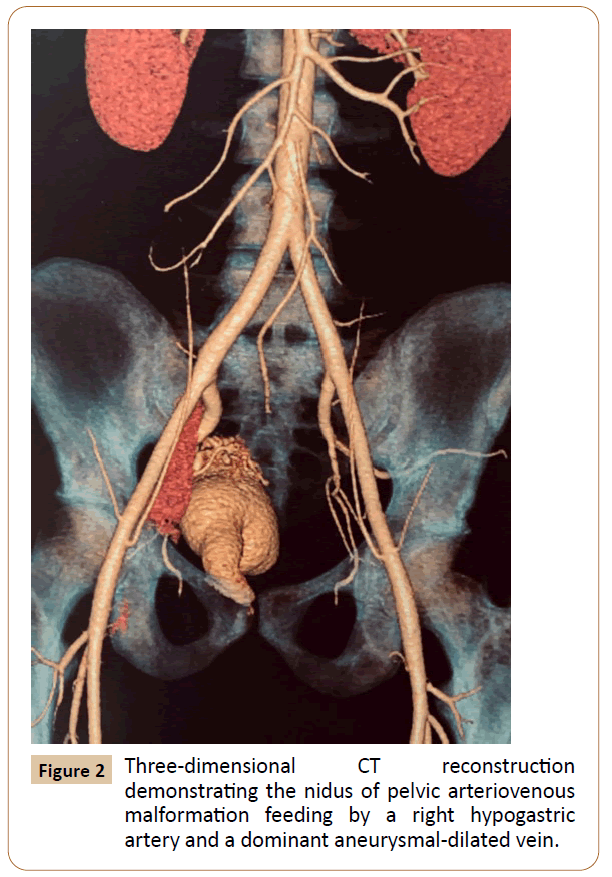
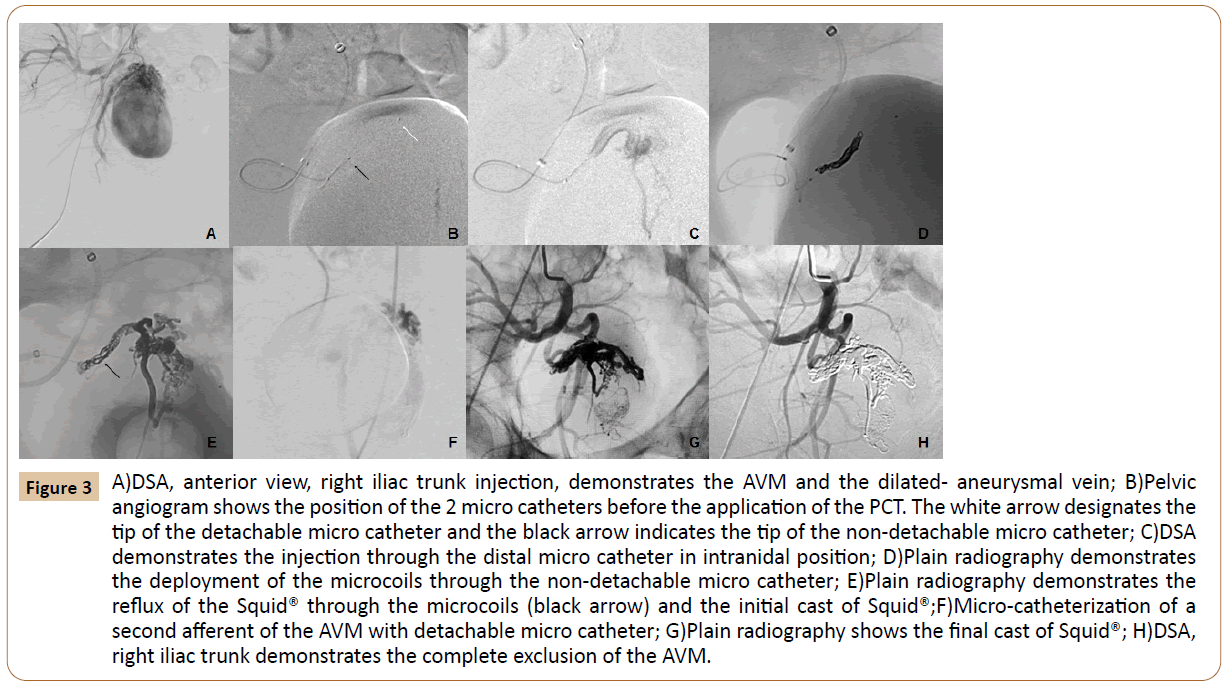
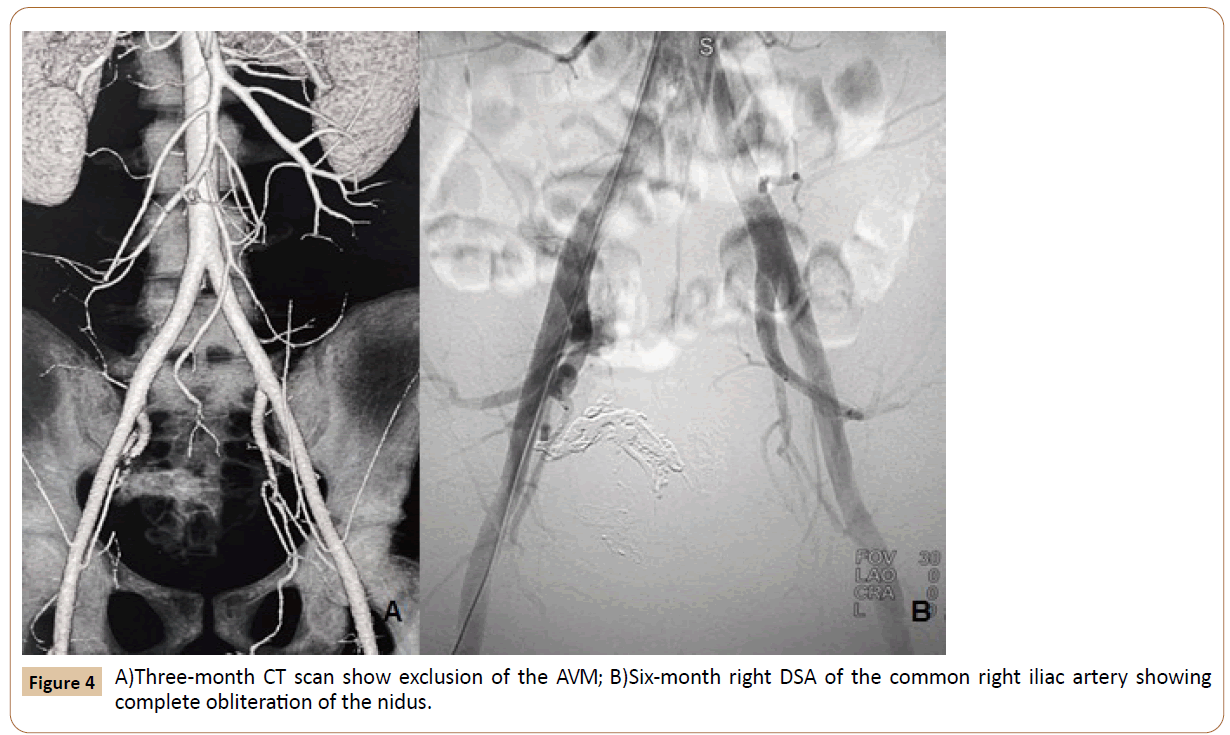
Under general anesthesia baseline pelvic arteriography demonstrated a large nidus with multiple feeding arteries originating from the anterior division branches of the right hypogastric which drained into a varicose venous channel before drainage into the right internal iliac vein (Figure 2). Left common femoral artery was punctured simultaneously using the Seldinger technique and a 6F long introducer sheath® (Balking, Cook, Indiana, USA) was positioned in the right hypogastricartery. Co-axially a DAC® 0,070” catheter (Stryker, Michigan, USA) was positioned in the anterior trunk. The strategy was to occlude the main feeder using the principle of pressure cooker technique (PCT) [7] to avoid reflux and enable a more comprehensive, forceful and continuous injection of Squid® 12. Intranidal position was achieved with Apollo® 1.5 F detachable tip micro catheter (Medtronic, Irvine, CA, USA) over a Syncro® 0.010" microguidewire (Stryker, Michigan, USA). Navigation of a second micro catheter (Headway Duo, Microvention, CA, USA), in the same feeder was then achieved with its distal tip positioned between the detachment zone and the distal marker of the Apollo®. Next, 5 Target® microcoils (Stryker, Michigan, USA) were then positioned through the Headway Duo micro catheter (Figure 3), creating a plug around the detachable micro catheter. After removing the Headway® Duo we proceeded with the injection of Squid® 12 through the detachable tip micro catheter until angiographic exclusion of that compartment of the AVM (Figure 4). Apollo®microcatheterwassuccessfullyremov ed.Therestoftheniduswasstillperfusedthrough other two smaller feeding arteries that were occluded with selective micro catheter is musing Squid® 12. Finally, right common iliac arteriography showed almost total obliteration of the nidus and the aneurysmal dilated vein. Six month after, complete occlusion of the AVM was observed on the CT and angiography control.
Figure 3 A)DSA, anterior view, right iliac trunk injection, demonstrates the AVM and the dilated- aneurysmal vein; B)Pelvic angiogram shows the position of the 2 micro catheters before the application of the PCT. The white arrow designates the tip of the detachable micro catheter and the black arrow indicates the tip of the non-detachable micro catheter; C)DSA demonstrates the injection through the distal micro catheter in intranidal position; D)Plain radiography demonstrates the deployment of the microcoils through the non-detachable micro catheter; E)Plain radiography demonstrates the reflux of the Squid® through the microcoils (black arrow) and the initial cast of Squid®;F)Micro-catheterization of a second afferent of the AVM with detachable micro catheter; G)Plain radiography shows the final cast of Squid®; H)DSA, right iliac trunk demonstrates the complete exclusion of the AVM.
Discussion
Pelvic AVM has different causes (idiopathic, post-traumatic, neoplastic, and congenital) and can be life-threatening during delivery or rupture (spontaneous or post-traumatic) [2-4]. An arteriovenous malformation is an abnormal communication between arteries and veins with a nidus, which infrequently occurs in the pelvis, representing only 1.8% of the major abdominal AVM localizations [2-4].
Surgical resection for congenital pelvic AVMs is often more complicated due to the typically complex network of arteriovenous communications and intimate association of the abnormal vessels to critical structures within the pelvis. For these reasons, surgery is not performed as frequently for pelvic AVMs. Transcatheter embolization has emerged as the preferred treatment for AVMs [4]. Given these high clinical success rates, endovascular therapy (ET) is often the recommended initial therapy for pelvic AVMs requiring treatment.
Various embolic agents have been successfully used in ET, including PVA and other particulate embolic agents, liquid embolic agents including n-butyl-cyanoacrylate glue, Gelfoam, and coils they are often used in combination (Divya Sridhar) Venturiniet al. [8] described the embolization of the target artery and the nidus of AVMs using PVA particles, coils or amplatzer plug with Squid.
EVOH polymers have been used widely in embolization procedures with considerable success since their first introduction by Terada et al. [6]. Squid® is an EVOH copolymer that has become available recently. It also has a less viscous formulation (Squid 12) for improved vascular penetration and as a lower density formulation (Squid LD) compared to Onyx®. The Squid was more slowly injected (60-90 s) to minimize DMSO toxicity and to ensure its tolerability also in case of endovascular treatment of small vessels.
For embolization of an arteriovenous malformation (AVM) with multiple feeding arteries and a single draining vein, control of blood flow to the nidus is critical. Generally, blood flow through then idusis equal between the draining vein and feeding arteries. When arterial flow to the indus decreases, draining venous flow also decreases, draining venous flow also decreases, draining venous flow also decreases, and vice versa. In this sense, Murakami et al. [9], described a pelvic AVM treated by transarterial embolization combining proximal balloon occlusion to decrease the arterial flow and control the intranidal injection of glue.
Perhaps the most important technical characteristic of the EVOH polymers injection is the control of reflux. After the plug formation and solidification along the microcatheter, the embolic agent penetrates the target region. The control of this reflux is essential throughout the entire procedure and may limit the final result [2]. For permanent control of reflux PCT was designed to create an anti- reflux plug by trapping the detachable part of an EVOH polymer-compatible microcatheter with coils and glue in order to obtain wedge-flow conditions, thereby enabling a better understanding of macro fistulous AVMs and a more comprehensive, forceful and controlled liquid embolization. Certainly, it can be used with others EVOH polymers to treat different diseases.
In conclusion, the present transarterial technique variations associated with lower viscosity formulation of the Squid® 12 enabled better nidus penetration and make reflux control easier.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Nakad G, AbiChedid G, Osman R (2014) Endovascular treatment of major abdominal arteriovenous fistulas: a systematic review. Vasc Endovascular Surg 48: 388-395.
- Gandini R, Angelopoulos G, Konda D, Messina M, Chiocchi M, et al. (2008) Transcatheter embolization of a large symptomatic pelvic arteriovenous malformation with Glubran 2 acrylic glue. Cardiovasc Intervent Radiol 31: 1030-1033.
- Do YS, Kim YW, Park KB, Kim DI, Park HS, et al. (2012) Endovascular treatment combined with embolosclerotherapy for pelvic arteriovenous malformations. J Vasc Surg 55: 465-471.
- Calligaro KD, Sedlacek TV, Savarese RP, Carneval P, De Laurentis DA (1992) Congenital pelvic arteriovenous malformations: long-term follow-up in two cases and a review of the literature. J Vasc Surg 16:100-108.
- Cho SK, Do YS, Shin SW, Kim DI, Kim YW, et al. (2006) Arteriovenous malformations of the body and extremities: analysis of therapeutic outcomes and approaches according to a modified angiographic classification. J EndovascTher13:527-538.
- T Terada, Y Nakamura, K Nakai, M Tsuura, T Nishiguchi, et al. (1991) Embolization of arteriovenous malformations with peripheral aneurysms using ethylene vinyl alcohol Copolymer. Report of three cases. J Neurosurg 75: 655-660.
- Chapot R, Stracke P, Velasco A, Nordmeyer H, Heddier M, et al. (2014)The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol 41:87-91.
- Venturini M, Lanza C, Marra P, Colarieti A, Panzeri M, et al. (2019) Transcatheter embolization with Squid, combined with otherembolic agents or alone, in different abdominal diseases: a single-center experience in 30 patients. CVIR Endovasc 2: 8.
- Murakami K, Yamada T, Kumano R, Nakajima Y (2014) Pelvic arteriovenous malformation treated by transarterial glue embolisation combining proximal balloon occlusion and devascularisation of multiple feeding arteries. BMJ Case Rep.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences