Carotid Stenting of a Near Total Occlusion in a High Risk Patient Using Proximal and Distal Cerebral Embolic Protection
William L Bennett, Atul Singla, Robert Attaran, Nidal Abi-Rafeh and Carlos Mena-Hurtado
DOI10.21767/2573-4482.100061
William L Bennett1, Atul Singla1*, Robert Attaran1, Nidal Abi-Rafeh2 and Carlos Mena-Hurtado1
1Department of Medicine, Section of Cardiovascular Disease, Yale University, New Haven, Connecticut, USA
2Department of Medicine, Section of Cardiology, Tulane University School of Medicine, New Orleans Louisiana, USA
- *Corresponding Author:
- Atul Singla
Department of Medicine, Section of Cardiology
Yale University, 15 York Street, New Haven
Connecticut, 06520-8017, USA.
Tel: 2037377673
Fax: 2036886117
E-mail: atulsingla14@gmail.com
Received date: July 26, 2017; Accepted date: October 16, 2017; Published date: October 23, 2017
Citation: Bennett WL, Singla A, Attaran R, Abi-Rafeh N, Mena-Hurtado C (2017) Carotid Stenting of a Near Total Occlusion in a High Risk Patient Using Proximal and Distal Cerebral Embolic Protection. J Vasc Endovasc Surg. 2:28 doi: 10.21767/2573-4482.100061
Case Report
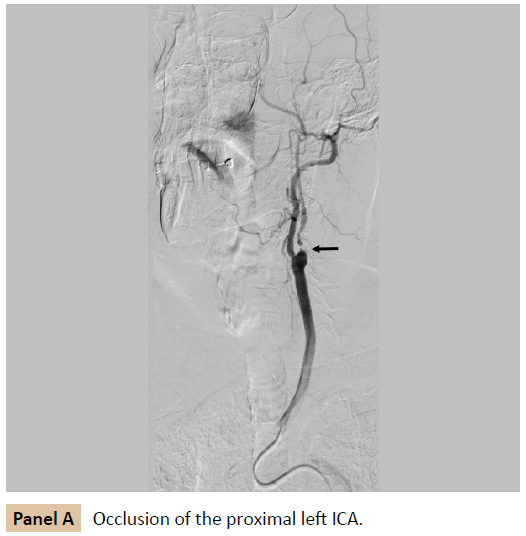
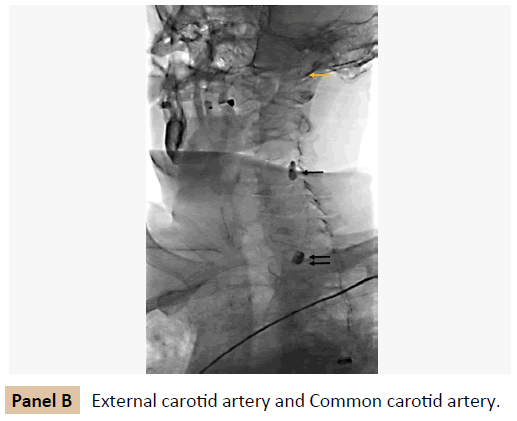
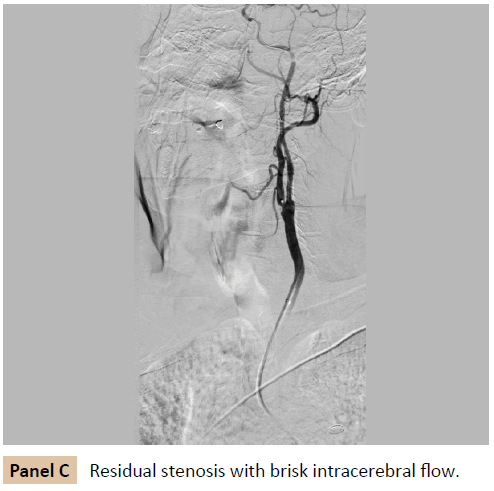
A 65 year old man with past medical history of hypertension, hyperlipidemia, diabetes mellitus, and smoking presented with right sided weakness and elevated troponin. MRI brain revealed acute bilateral cerebral hemisphere infarcts. Carotid ultrasound duplex demonstrated 99% stenosis of the left internal carotid artery (ICA). Additional workup revealed three vessel coronary artery diseases with ejection fraction of 25%. He was referred for revascularization of carotid artery disease prior to coronary artery bypass surgery. After extensive discussion of risks versus benefits of endarterectomy and stenting, he opted for carotid stenting. Carotid angiography confirmed near total occlusion of the proximal left ICA (Panel A, arrow). A proximal embolic protection device (MoMa Ultra, Medtronic, Minneapolis, MN) was advanced into the external carotid artery (Panel B, black single arrow) and common carotid artery (Panel B, double arrows) and both occlusion balloons were sequentially inflated to occlude antegrade flow in the ICA. A distal embolic protection device (Emboshield Nav 6, Abbott, Santa Clara, CA) was advanced beyond the stenosis and filter deployed (Panel B, yellow arrow). The lesion was predilated with a 3.0 x 20 mm balloon (Emerge MR, Boston Scientific, Malborough, MA), followed by deployment of a 8.0 x 21 mm self-expanding stent (Wallstent, Boston Scientific, Malborough, MA). The system was carefully aspirated several times to ensure all embolic particles were removed, and occlusion balloons were deflated, restoring flow to the internal carotid artery. The distal filter was retrieved. Postprocedure angiograms demonstrate minimal residual stenosis with brisk intracerebral flow (Panel C). Following the procedure, the patient had no neurological deficits.
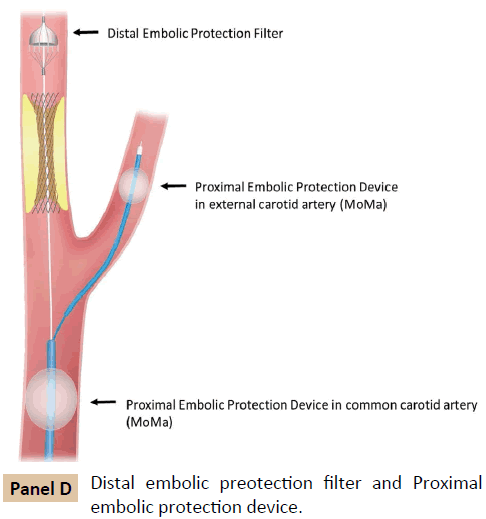
Internal carotid artery disease accounts for up to 20% of ischemic strokes [1]. The risk of stroke increases with the degree of stenosis, and in the presence of symptoms. Stroke risk decreases with near total occlusion (95-99% stenosis), yet remains significant [1]. Although carotid endarterectomy (CEA) has been the gold standard for treating symptomatic carotid disease, carotid artery stenting (CAS) has emerged as a viable alternative in selected patients. The use of CAS has been limited by the potential of embolization of plaque debris to the brain and resultant neurological sequelae. The use of single proximal or distal embolic protection devices has been shown to reduce embolic events, and is currently the standard of practice [2] (Panal D). It is therefore intuitive that combining proximal and distal embolic protection devices would further reduce the risk of distal embolization during CAS (panel D). A recent study by Varbella et al., suggests the use of dual embolic protection to be feasible in patients with high-risk lesions [3]. Although dual protection increases the complexity and the duration of the procedure, it is likely to be successful in the hands of experienced operators. In the case presented here, this proved to be a safe and highly effective strategy for successful revascularization of a carotid artery near total occlusion.
References
- Inzitari D, Eliasziw M (2000) The Causes and Risk of Stroke in Patients with Asymptomatic Internal-Carotid-Artery Stenosis. New England J Medicine 342: 1693-1700.
- Bersin RM, Stabile E (2012) A Meta-Analysis of Proximal Occlusion Device Outcomes in Carotid Artery Stenting. Catherization and Cardiovascular Interventions 80: 1072-1078.
- Varbella F, Gagnor A, Tomassini F (2016) Feasibility of Carotid Artery Stenting With Double Cerebral Embolic Protection in High-Risk Patients. Catherization and Cardiovascular Interventions 87: 432-437.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences