Retrograde Endovascular Revascularization of Anterior Tibial Artery via the Dorsal and Plantar Arches
Yoshida RdA
DOI10.21767/2573-4482.100020
Botucatu School of Medicine, Paulista State University (UNESP), Campus de Botucatu, São Paulo, Brazil
- *Corresponding Author:
- Yoshida RdA
Department of Surgery and Orthopedics
Botucatu School of Medicine, Paulista State University (UNESP)
Campus de Botucatu, São Paulo, Brazil, CEP 18618-970
Tel: +5512997450977
E-mail: ricardoyoshida@gmail.com
Received Date: August 10, 2016; Accepted Date: August 31, 2016; Published Date: September 07, 2016
Citation: Yoshida RdA. Retrograde Endovascular Revascularization of Anterior Tibial Artery via the Dorsal and Plantar Arches. J Vasc Endovasc Surg. 2016, 1:3. doi: 10.21767/2573-4482.100020
Abstract
Background: Endovascular techniques through anterograde approaches are routinely used in infragenicular endovascular procedures, but sometimes total chronicle occlusions transposition are not possible. Puncture of the distal arteries and retrograde approach have been reported to improve the chances of successful artery occlusion transposition.
Case report: Patient female, presenting with necrosis of right foot toes and infragenicular arteries occlusions.
Results: We report a successful case using anterograde approach via posterior tibial artery, crossing the dorsal or plantar arches and retrograde endovascular revascularization of anterior tibial artery.
Conclusion: The combined anterograde-retrograde access crossing the dorsal and pedal arches is feasible and could avoid complications related to direct artery puncture.
Keywords
Angioplasty; Stent; Endovascular procedure; Peripheral blood
Introduction
Critical limb ischemia is described by rest pain and/or tissue loss, and occurs in about 25% of cases of peripheral atherosclerotic occlusive disease (PAOD), which could suffer some kind of limb amputation [1,2].
Patients with Diabetes, especially, often develop critical limb ischemia with arterial lesions in multiple segments, mainly in infragenicular [3]. Typical angiographic findings in those cases are extensive occlusive lesions of the tibial arteries and preservation of fibular artery, dorsalis pedis, and malleolar arteries [4,5].
Bellow-the-knee (BTK) revascularizations using venous grafts decrease the risk of major amputations [3,6]. With the improvement of endovascular techniques and its devices, the endovascular approach has become the preferred strategy for the treatment of lesions in infragenicular arteries [4,7,8]. However, the traditional anterograde approach may fail in 20% of cases in BTK endovascular revascularization, especially in long chronic total occlusions (CTO), with significant calcification and diffuse disease in the distal arteries, which also impairs the distal foot blood run-off, even after successful recanalization [9,10]. Retrograde approaches through pedal-plantar puncture or by combined techniques of anterograde-retrograde accesses- SAFARI [11] have been reported to improve the success rates [4,9,12-14]. The alternative to direct puncture of the tibial arteries would be crossing pedal-plantar arteries starting from anterograde approach of one tibial artery aiming in a retrograde fashion at the other tibial artery; this has been demonstrated in only one previous case report [2], and the technical success obtained motivated a small modification presented in this report, with retrograde percutaneous revascularization of the anterior tibial artery by crossing the plantar and the pedal arches, after previous anterograde revascularization of the posterior tibial artery.
Case Report
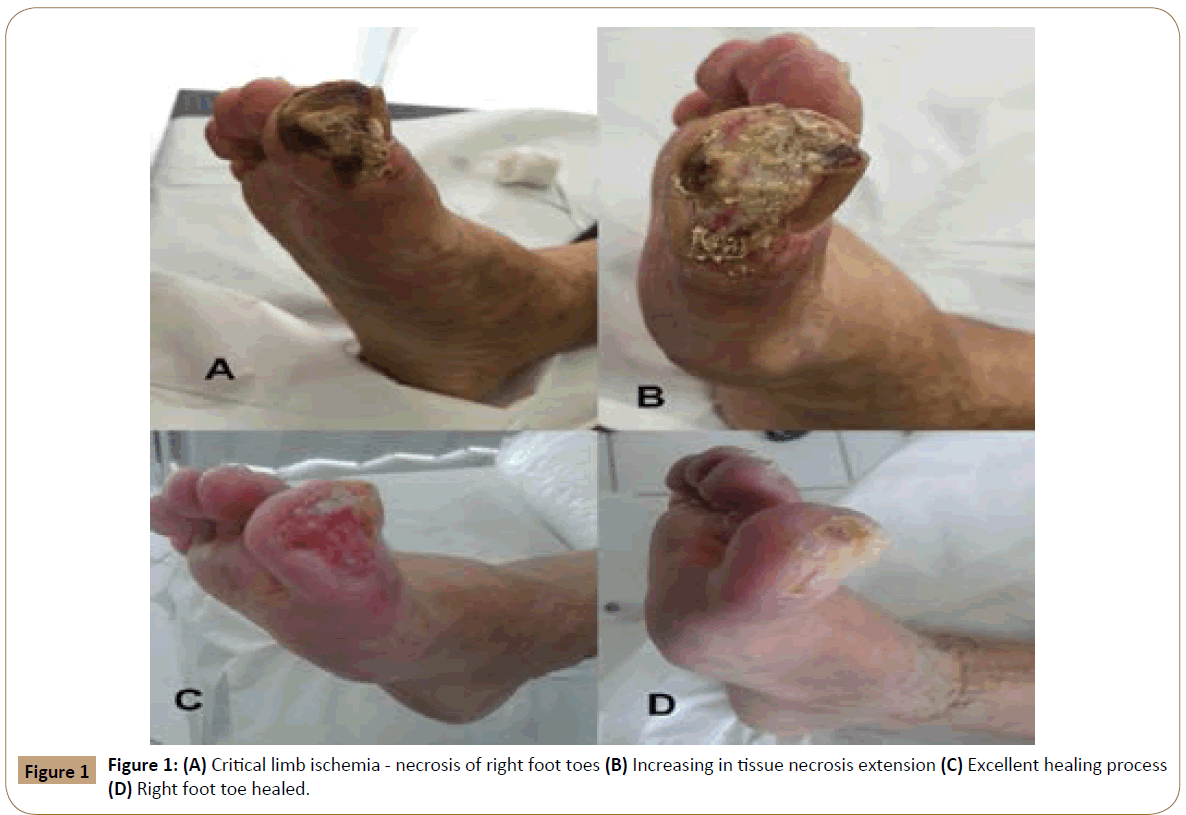
A 77-year old female patient, arterial hypertension, Diabetes mellitus, and coronary heart disease (previous AMI, postoperative period of coronary angioplasty), and non-dialysis chronic renal failure (creatinine clearance=25 mL/min), PAOD, symptoms of heart failure, presenting necrosis of right foot toes, for the last 3 months (Figure 1A).
Two months ago she underwent a successful angioplasty of right fibular and posterior tibial arteries. At the time, there was an unsuccessful attempt of anterograde recanalization of the anterior tibial artery. Since no dorsalis pedis run-off, retrograde recanalization was not considered. The procedure was completed with popliteal and posterior tibial pulses, as well as clinical improvement. Nonetheless, in the following month the rest pain returned and there was increase in tissue necrosis extension (Figure 1B).
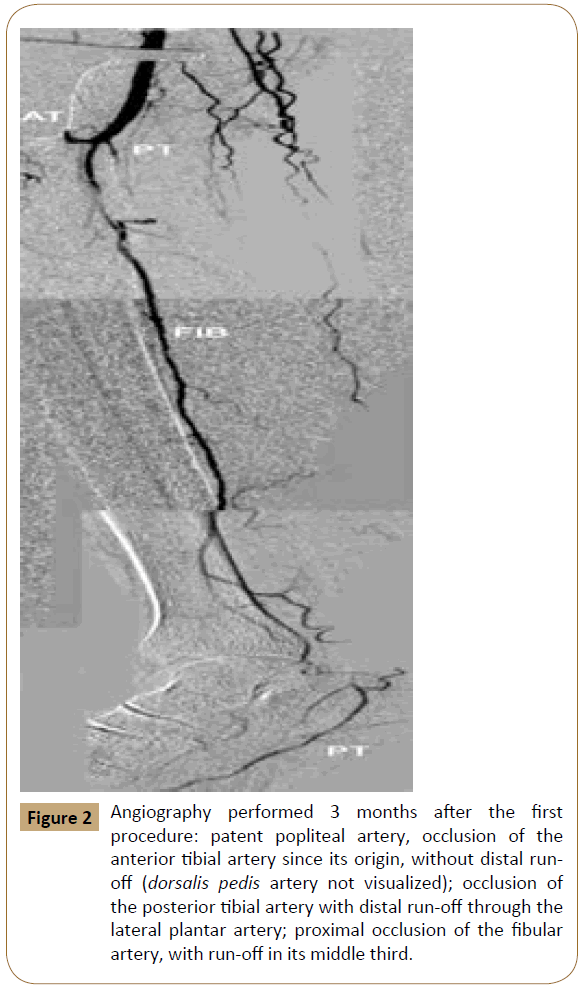
A new angiography was performed, revealing: patent popliteal artery, occlusion of the anterior tibial artery since its origin without distal run-off (dorsalis pedis artery not visualized); occlusion of the posterior tibial artery with distal run-off through the lateral plantar artery; proximal occlusion of the fibular artery, with run-off in its middle third (Figure 2).
Figure 2: Angiography performed 3 months after the first procedure: patent popliteal artery, occlusion of the anterior tibial artery since its origin, without distal runoff (dorsalis pedis artery not visualized); occlusion of the posterior tibial artery with distal run-off through the lateral plantar artery; proximal occlusion of the fibular artery, with run-off in its middle third.
A new attempt of angioplasty was decided in order to limb salvage. The saphenous vein was mapped and it was inappropriate to be used as bypass. In addition, the patient had high clinical risk for open surgery.
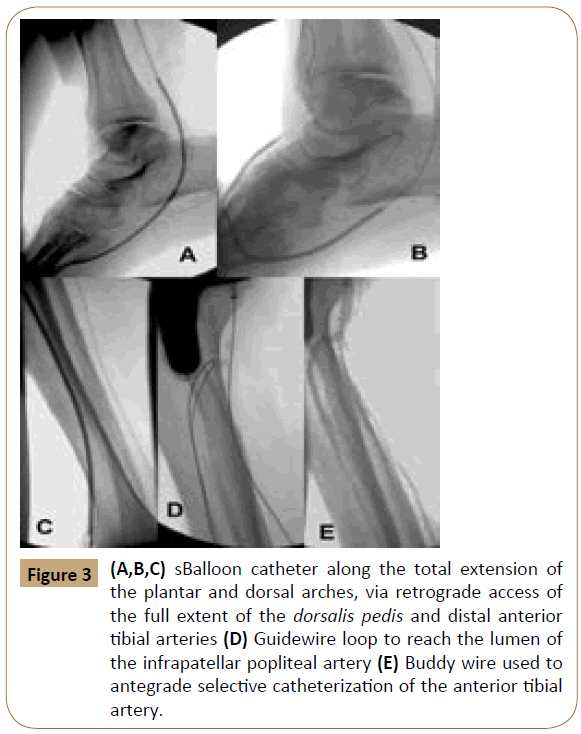
By anterograde ipsilateral femoral puncture and placement of long 55 cm sheath, the fibular artery was selectively catheterized with a 0.018 guidewire and a balloon angioplasty was performed with a 3.0 x 220 balloon catheter with excellent angiographic result. After selective catheterization of the posterior tibial artery origin, a CommandR (Abbott Vascular, Illinois-USA) 0.014 guidewire was progressed distally, guided by a Quick CrossR (Spectranetics, Colorado Springs-USA) supporting catheter crossing the occlusive lesion reaching the true lumen in the plantar artery. Control angiography showed, interestingly, patent dorsal arch, despite having numerous severe segmental stenosis. Then a 0.014 CommandR guidewire was distally progressed through dorsal and plantar arches and reached the distal third of the anterior tibial artery. Via retrograde fashion a balloon angioplasty was performed with 2.5 x 200 mm Armada 14 balloon catheter (Abbott Vascular, Illinois-USA) along total extension of the plantar and dorsal arches, followed by sequential angioplasties of the full extension of the dorsalis pedis and distal anterior tibial arteries, with great difficulty, but nevertheless with success (Figure 3A-C). In sequence it was possible to perform the retrograde revascularization of the anterior tibial artery until close to its origin, as far as the length of the shaft device could reach. In order to cross the extremely calcified occlusive lesion of the anterior tibial artery arch, the 0.014 guidewire was replaced by a 0.035 hydrophilic stiff guidewire, supported by a Quick Cross supporting catheter. A loop was performed with the guidewire in order to cross this occlusive lesion and, after several maneuvers it was possible to reach the lumen of the popliteal artery. The 0.035 hydrophilic stiff guidewire was used to guide (buddy wire) the anterograde selective catheterization of the anterior tibial artery with a 0.018 Connect guidewire (Abbott Vascular, Illinois-USA) (Figure 3D and E). After removing the retrograde hydrophilic guidewire, the anterograde angioplasty of the anterior tibial artery was successfully performed with a 3.0x220 balloon catheter.
Figure 3: (A,B,C) sBalloon catheter along the total extension of the plantar and dorsal arches, via retrograde access of the full extent of the dorsalis pedis and distal anterior tibial arteries (D) Guidewire loop to reach the lumen of the infrapatellar popliteal artery (E) Buddy wire used to antegrade selective catheterization of the anterior tibial artery.
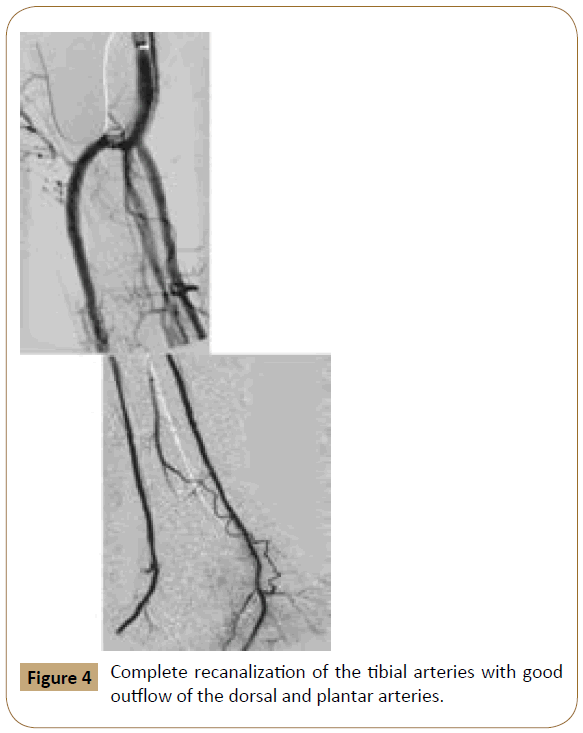
The final angiogram showed the fibular artery totally revascularized as well the anterior and posterior tibial arteries. Although fully revascularized, the tibial arteries presented with hemodynamically significant dissections in their proximal segments; after numerous unsuccessful attempts of correction by angioplasty, two 3.5x60 self-expanding stents were deployed in the anterior and posterior tibial arteries, respectively, providing complete revascularization and reestablishment of blood flow, with good outflow of the dorsal and plantar arteries (Figure 4).
The patient received dual antiplatelet therapy (ASA 100 mg+Clopidogrel 75 mg). There was no change in renal function after the procedure due to parenteral hydration and contrast saving.
After 2 months of treatment the patient was in excellent healing process (Figure 1C) of the ischemic lesions with maintenance of the AT and PT pulses with ABI 1.0 in AT, PT and Fib). After 6 months the healing process was complete with maintenance of the AT and PT pulses with ABI 1.0 in AT, PT and Fib (Figure 1D).
Discussion
Critical limb ischemia secondary to infragenicular PAOD is associated with high amputation and low survival rates [1,13]. BTK region, the re-establishment of pulsatile flow to the pedal and plantar arches is key to foot and limb salvage [4,15]. According to "angiosome" theory the blood supply to the toes depends on the anastomoses between the medial plantar, lateral plantar and first dorsal metatarsal, and of its supply from the tibial arteries [13,16,17]. The restoration of both in the case described definitely had a significant impact on the wound healing on toes.
With the increasing technological sophistication of the endovascular devices, the strategy of "endovascular first " for limb salvage in infragenicular PAOD has been increasingly used [4,6,8]. This strategy has at least two advantages: (1) it is less invasive than the distal bypasses, with less risk of infection; (2) early or late redo possibility, preserving the target vessels for future grafts. BTK angioplasties have technical success rates that range from 79% for occlusions to 99% for stenosis, and 75% limb salvage for occlusions to 92% for stenosis in one year, as long as technically successful [14,15,18]. The technical challenge in endovascular revascularization is CTO transposition. Anterograde revascularization of CTO with subintimal or intraluminal techniques is safe and feasible [3,4,19]. In this case reported, the anterograde revascularization of the posterior tibial and fibular arteries using this technique was successfully done.
In the failure of revascularization through isolated anterograde approach, techniques of anterograde and retrograde accesses (SAFARI technique) can be performed simultaneously, often through the subintimal space, in order to achieve technical success [11,13]. According to the literature, the retrograde access by puncture of the dorsalis pedis, the metatarsals or the distal anterior tibial arteries allows the treatment of CTO that cannot be done by isolated anterograde approach [4,9,10,13]. An adjuvant retrograde approach improves the technical success rate around to 87% and is a viable option when: (1) isolated anterograde recanalization failed; (2) anterograde revascularization has low technical success-the occlusion is located at the origin of an artery or trifurcation of a large collateral artery, preventing the selective catheterization of the target vessel; (3) when there is difficulty in establishing an anterograde subintimal path due to the presence of excessive calcification; (4) when there is a reentry failure in the true lumen distal to the occlusion [13].
However, the puncture of these small arteries has some limitations: (1) requires a long learning curve; (2) requires an adequate access site, which sometimes is very restricted due to ulcers and infections; (3) may be complicated by stenotic or occlusive lesions in distal branches or even injured vessels due to multiple punctures or as a consequence of access devices (sheaths); (4) may be the cause for the target vessel occlusion due to intimal lesions or dissections; (5) distal arteries are more likely to have spasms [4,9,10,12]. To avoid these problems of the distal punctures, Kawarada et al., [4] presented an alternative of performing retrograde angioplasty crossing the pedal-plantar artery anastomoses. In this report, a slight modification of this technique was done with anterograde approach of the posterior tibial artery, followed by the crossing of the arteries of the dorsal arch, then plantar arch crossing and retrograde angioplasty of the anterior tibial artery, followed by Buddy-wire maneuver to complete the anterior tibial artery arch angioplasty.
There is no consensus as yet of how many and which distal arteries should be treated, especially when faced with CTO. In addition, in patients with Diabetes, where there is a predominance of BTK lesions, it is not known whether the isolated treatment of one artery, usually fibular artery, would be enough to heal wounds and reduce amputation rates, or if there would be the need for revascularization of at least one tibial artery to obtain better results [3,8,15,20], in 221 cases showed that some patients ( ± 4%) which had initial technical success did not heal the ischemic lesions as expected. In that study, the authors concluded that the isolated treatment of the fibular artery (commonly the most preserved in diabetic patients) could not prevent major amputation, and revascularization of at least one tibial artery reduced the rate of major amputations [3,8,15].
The use of stents in the infragenicular segment is another controversial issue. In a recent systematic review, their use is recommended in cases of failed angioplasty, salvaging the target vessel revascularizated [21]. In this case reported, the stents deployments in the proximal segments of the anterior and posterior tibial arteries were due to failure the angioplasty, with persistent significant residual stenosis and hemodynamically significant dissection.
In conclusion, in this case reported, after the failure of the attempted anterograde revascularization of the anterior tibial artery, the combined anterograde-retrograde access crossing the dorsal and pedal arches, performed without puncture of the dorsalis pedis or anterior or posterior tibial arteries, allowed the anterior tibial artery angioplasty, avoiding thereby the complications described related to direct puncture of these vessels [4].
References
- Norgren L, Hiatt WR, Dormandy JA (2007) Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J VascEndovascSurg 33:S1-S75.
- Yoshida RA, Matida CK, Sobreira ML (2008) Comparative study of evolution and survival of patients with intermittent claudication, with or without limitation for exercises, followed in a specific outpatient setting. Jornal Vascular Brasileiro 7:112-122.
- Yoshida RA, Silva CECd, Sobreira ML (2008)Infrapopliteal angioplasty: the more arteries are treated the better.Jornal Vascular Brasileiro 7:176-182.
- Kawarada O, Yokoi Y, Sekii H (2008) Retrograde crossing through the pedal arch for totally occluded tibial artery. J IntervCardiol 21:342-346.
- Santos VPD, Alves CAS, Fidelis C (2013)Arteriographic findings in diabetic and non-diabetic with critical limb ischemia. Revista da AssociaçãoMédicaBrasileira 59:557-562.
- Adam DJ, Beard JD, Cleveland T (2005) Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366:1925-1934.
- Adam DJ, Bradbury AW (2007) TASC II document on the management of peripheral arterial disease. Eur J VascEndovascSurg 33:1-2.
- Faglia E, Dalla PL, Clerici G (2005) Peripheral angioplasty as the first-choice revascularization procedure in diabetic patients with critical limb ischemia: prospective study of 993 consecutive patients hospitalized and followed between 1999 and 2003. Eur J VascEndovascSurg 29:620-627.
- MonteroBM, Schmidt A, Braunlich S (2008)Retrograde approach for complex popliteal and tibioperoneal occlusions. J EndovascTher 15:594-604.
- Palena LM, Brocco E, Manzi M (2014)The clinical utility of below-the-ankle angioplasty using "transmetatarsal artery access" in complex cases of CLI. Catheter CardiovascInterv 83:123-129.
- Spinosa DJ, Harthun NL, Bissonette EA (2005)Subintimal arterial flossing with antegrade-retrograde intervention (SAFARI) for subintimal recanalization to treat chronic critical limb ischemia. J VascIntervRadiol 16:37-44.
- Ruzsa Z, Nemes B, Bansaghi Z (2014)Transpedal access after failed anterograde recanalization of complex below-the-knee and femoropoliteal occlusions in critical limb ischemia. Catheter CardiovascInterv 83:997-1007.
- Sabri SS, Hendricks N, Stone J (2015) Retrograde pedal access technique for revascularization of infrainguinal arterial occlusive disease. J VascIntervRadiol 26:29-38.
- Singh GD, Armstrong EJ, Yeo KK (2014) Endovascular recanalization of infrapopliteal occlusions in patients with critical limb ischemia. J VascSurg 59:1300-1307.
- Faglia E, Mantero M, Caminiti M (2002) Extensive use of peripheral angioplasty, particularly infrapopliteal, in the treatment of ischaemic diabetic foot ulcers: clinical results of a multicentric study of 221 consecutive diabetic subjects. J Intern Med 252:225-232.
- Attinger CE, Evans KK, Bulan E (2006) Angiosomes of the foot and ankle and clinical implications for limb salvage: reconstruction, incisions, and revascularization. PlastReconstrSurg 117:S261-S293.
- Biancari F, Juvonen T (2014)Angiosome-targeted lower limb revascularization for ischemic foot wounds: systematic review and meta-analysis. Eur J VascEndovascSurg 47:517-522.
- Romiti M, Albers M, Brochado-Neto FC (2008) Meta-analysis of infrapopliteal angioplasty for chronic critical limb ischemia. J VascSurg 47:975-981.
- Nydahl S, London NJ, Bolia A (1996) Technical report: Recanalisation of all three infrapopliteal arteries by subintimal angioplasty. ClinRadiol 51:366-367.
- Faglia E, Clerici G, Clerissi J (2007) When is a technically successful peripheral angioplasty effective in preventing above-the-ankle amputation in diabetic patients with critical limb ischaemia. Diabet Med 24:823-829.
- Jens S, Conijn AP, Koelemay MJ, (2014) Randomized trials for endovascular treatment of infrainguinal arterial disease: systematic review and meta-analysis (Part 2: Below the knee). Eur J VascEndovascSurg47:536-44.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences