Endovascular Management of Acute Pulmonary Embolus
Reis PEO*, Roever L and Reis IFO
DOI10.21767/2573-4482.100011
1Fluminense Federal University, Rio de Janeiro, Brazil
2Federal University of Uberlândia, Brazil
3Vascular Clinic Ocke Reis, Rio de Janeiro, Brazil
- *Corresponding Author:
- Reis PEO
Department of Specialized and General Surgery Fluminese Federal University, Rio de Janeiro, Brazil
Tel: +55 21 2629 5000
E-mail: vascular@pauloocke.com.br
Received date: May 09, 2016; Accepted date: May 11, 2016; Published date: May 13, 2016
Citation: Reis PEO, Roever L, Reis IFO. Endovascular Management of Acute Pulmonary Embolus. Journal of Vascular & Endo Surgery. 2016, 1:2. doi: 10.21767/2573-4482.100011
Keywords
Embolims; Treatment; Endovascular
Introduction
The first pulmonary embolectomy was done by Friedrich Trendelenburg in 1908 with no survivor and the first successful pulmonary embolectomy was in 1924 [1-3]. Now approximately 630 000 pulmonary embolisms (PE) occur yearly in the United States, resulting in 300 000 deaths [4-8].
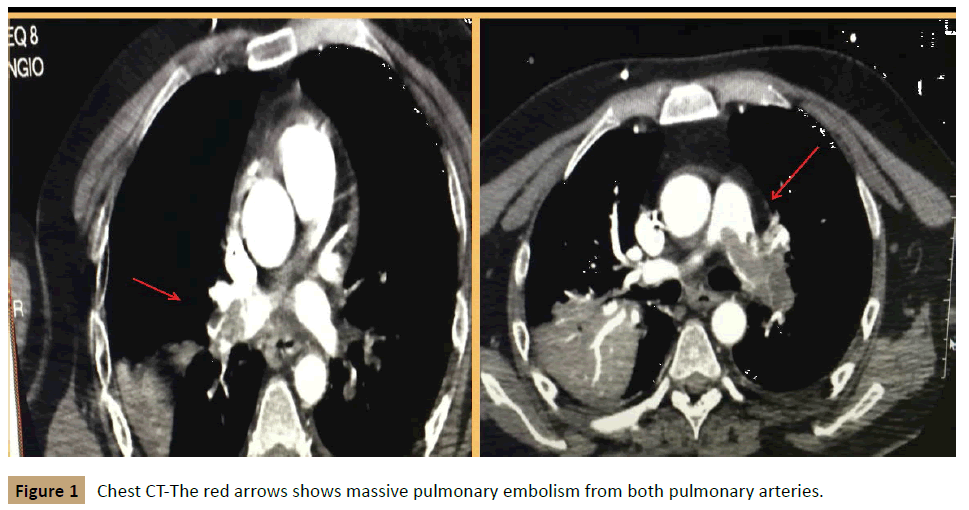
The symptoms most often found in patients with PTE are: dyspnea, chest pain, pleuritic chest pain, cough, swelling of the legs, pain in legs, hemoptysis, palpitations, wheezing, chest pain type angina, syncope, hemodynamic instability, acute right ventricular failure, cardiogenic shock and the main imaging methods used in the diagnosis are ventilation-perfusion scintigraphy, pulmonary angiography and computed tomography (CT) (Figure 1).
The guidelines for the management of TEP addresses the risk factors for major and minor, as the relative risk requiring the occurrence of TEP (Table 1). Deep vein thrombosis (DVT) in the lower limbs is mainly responsible for pulmonary thromboembolism (PTE) [9].
| Major (relative risk between 5 and 20) | Lower (relative risk between 2 and 4) |
| • Surgeries Major abdominal surgery or pelvic/Hip prosthesis or knee/Post-operative ICU • Obstetrical Events End of pregnancy/Cesarean/Puerperium • Lower members Fractures/Varicose Veins • Neoplasms Abdominals/Pelvic/Metastatic • Immobilization Hospitalization/Nursing Homes • Others TVP confirmed prior |
• Cardiovascular Congenital heart disease/Heart failure Congestive/Hypertension/vein thrombosis Superficial/Central venous catheter • Estrogen therapy Contraceptive/Hormone replacement • Others COPD/Neurological Diseases/Hidden Neoplasms/Thrombotic disorders/Prolonged Travel/Obesity/Inflammatory disease intestinal/Nephrotic syndrome/Chronic Dialysis/Myeloproliferative disorders/Hemoglobinuria/Behcet's Disease |
Table 1: Risk factors for pulmonary embolism.
With the advancement of new endovascular technologies we have available various catheters for thrombectomy and thrombolysis to treat patients with massive or submassive PE [10-12]. Tajima et al. [10] described a modified rotating pigtail catheter to treat critical pulmonary emboli. Pulmonary embolectomy for massive PE could have good results [13,14]. However with endovascular procedures PE can be treated quickly and efficiently without a thoracotomy [15-18].
CHEST Guideline and Expert Panel Report published in 2016 suggest the use of catheter-removing thrombus or mechanical interventions in patients with acute pulmonary embolism associated with hypotension, and have a high risk of bleeding or failed systemic thrombolysis, or shock presence that it can progress to death before systemic thrombolysis [19].
In conclusion we agree that probably some patients PE should be treated to remove the embolus and if the PE does not affect right ventricular function the patient will generally do well with anticoagulation.
References
- Jamielson SW (2006) Historicalperspective: surgery for chronic thromboembolic disease. Semin Thorac Cardiovasc Surg 2006 Fall 18: 218-222.
- Thistlethwaite PA, Jamielson SW (2007) Surgery for pulmonary embolism Sabiston & Spencer surgery of the Chest. Philadelphia: Elsevier Saunders 1723-1739.
- Madani MM, Jamielson SW (2003) Pulmonary Thromboendarterectomy In: Cohn LH Edmunds LH Jr (Eds) Cardiac surgery in the adult. New York: McGraw-Hill 1205-1228.
- Fedullo P, Auger W, Kerr K, Rubin L (2001) Chronic thromboembolic pulmonary hypertension. N Engl J Med 345: 1465-1472.
- Fedullo P, Tapson V (2003) Clinical practice. The evaluation of suspected pulmonary embolism. N Engl J Med 349: 1247-1256.
- Kucher N, Goldhaber S (2005) Management of massive pulmonary embolism. Circulation 112: 28-32.
- Hamilton Craig CR, McNeil K, Dunning J, Walters DL, Slaughter R, et al. (2008) Treatment options and strategies for acute severe pulmonary embolism. Intern Med J 38: 657-667.
- Zamanian RT, Gould MK (2008) Effectiveness and cost effectiveness of thrombolysis in patients with acute pulmonary embolism. Curr Opin Pulm Med 14: 422-426.
- Tarbox AK, Swaroop M (2013) Pulmonary embolism. Int J Crit Illn Inj Sci 2013 3: 69-72.
- Tajima H, Murata S, Kumazaki T (2004) Hybrid treatment of acute massive pulmonary thromboembolism: mechanical fragmentation with a modified rotating pigtail catheter, local fibrinolytic therapy and clot aspiration followed by systemic fibrinolytic therapy. AJR Am J Roentgenol 183: 589-595.
- Peter HL, Huiting C, Carlos FB, Panagiotis K (2010) Endovascular interventions for acute pulmonary embolism. Perspectives in Vascular Surgery and Endovascular Therapy 22: 171-182.
- Garcia MJ (2015) Endovascular management of acute PE using the Ultrasound-Enhanced EkoSonic System. Semin Intervent Radiol 32: 384-387.
- Aklog L, Williams CS, Byrne JG (2002) Acute pulmonary embolectomy: A contemporary approach. Circulation 105: 1416-1419.
- Yalamanchili K, Fleisher AG, Lehrman SG (2004) Open pulmonary embolectomy for treatment of major pulmonary embolism. Ann Thorac Surg 77: 819-823.
- Tajima H, Murata S, Kumazaki T (2004) Manual aspiration thrombectomy with a standard PTCA guiding catheter for treatment of acute massive pulmonary thromboembolism. Radiat Med 22: 168-172.
- De Gregorio MA, Gimeno MJ, Mainar A (2002) Mechanical and enzymatic thrombolysis for massive pulmonary embolism. J Vasc Interv Radiol 13: 163-169.
- Uflacker R, Strange C, Vujic I (1996) Massive pulmonary embolism: preliminary results of treatment with the Amplatz thrombectomy device. J Vasc Interv Radiol 7: 519-528.
- Wakefield TW, Caprini Comerota AJ (45) Thrombectomy catheters j, for pulmonary embolism from thromboembolic diseases. Curr Probl Surg 45: 833-900.
- Clive Kearon, Elie AA, Joseph Ornelas (2016) Antithrombotic therapy for VTE disease CHEST Guideline and Expert Panel Report. CHEST 149: 315-352.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences