Endovascular Management of Ruptured Traumatic Middle Meningeal Artery Pseudo aneurysm and Arteriovenous Fistula
UMohamad Abdalkader, Artem Kaliaev and Thanh Nguyen
DOI10.21767/2573-4482.19.04.12
Department of Neurosurgery, Boston University School of Medicine, Boston, Massachusetts, USA
- *Corresponding Author:
- Abdalkader M
Department of Neurosurgery Boston University School of Medicine Boston, Massachusetts, USA
Tel: 18572008308
E-mail: mohamad.abdalkader@bmc.org
Received date: April 28, 2019; Accepted date: May 22, 2019; Published date: May 29, 2019
Citation: Abdalkader M, Kaliaev A, Nguyen T. Endovascular Management of Ruptured Traumatic Middle Meningeal Artery Pseudo aneurysm and Arteriovenous Fistula. J Vasc Endovasc Therapy 2019, Vol.4 No.2:12.
Abstract
Pseudoaneurysm and arteriovenous fistula are the most common traumatic vascular injuries of the Middle Meningeal Artery (MMA). Although considered as a protection mechanism against epidural hematoma formation, these lesions carry a high risk of secondary rupture leading to delayed intracranial bleeding with high morbidity and mortality. The concomitant presence of both conditions is rarely reported. We report a case of post traumatic pseudoaneurysm and fistula of the MMA complicated by acute rupture and intracranial bleeding successfully treated by endovascular coiling and Onyx® embolization. We provide a literature review on both conditions and their endovascular management.
Keywords
Middle meningeal artery; Pseudoaneurysm; Arteriovenous fistula; Embolization
Introduction
Traumatic vascular injuries of the head and the neck are rare but serious complications of head and neck trauma [1]. Middle Meningeal Artery (MMA) injury usually results in extravasation of the blood in the epidural space forming an epidural hematoma. Pseudoaneurysm and arteriovenous fistula may limit the acute epidural hematoma formation by diverting the blood into the aneurysmal pouch or into the venous system. Although considered protective from the epidural hematoma, these lesions are considered high-risk vascular lesions because of the high risk of secondary rupture and intracranial bleeding [2-4]. A high index of suspicion of those lesions should be maintained especially in case of skull fracture or delayed neurological deterioration after head trauma and treatment should be considered to prevent serious complications [3,5]. Herein, we present a patient who exhibited both rare manifestations of traumatic injury to the middle meningeal artery.
Case Presentation
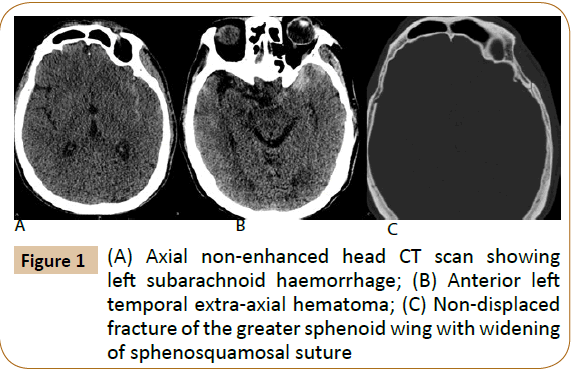
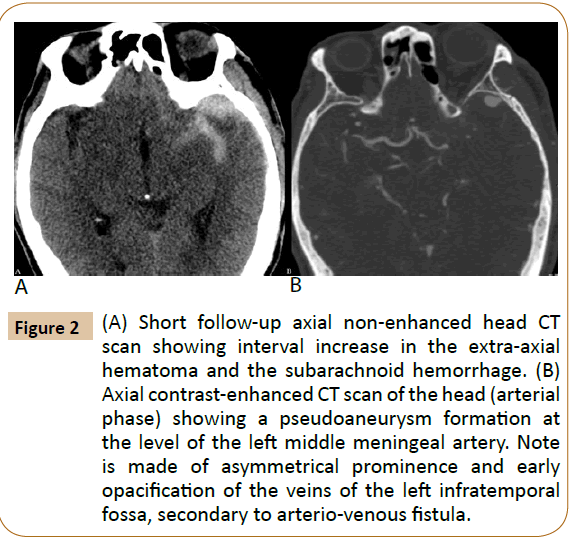
A 75-year-old man suffered a bicycle accident when he was riding his bike without a helmet. Head CT showed a nondisplaced fracture of the left parietal and sphenoid bones associated with left small anterior temporal epidural hematoma, thin right frontoparietal subdural hematoma and bilateral subarachnoid hemorrhage (Figure 1). The epidural hematoma was small with no significant mass effect. Follow-up CT brain and CTA were done after 6-hour showed interval increase in the size of the left anterior temporal epidural hematoma with 1.2 cm pseudoaneurysm of the left middle meningeal artery adjacent to the skull fracture (Figure 2). The agreement was to proceed with embolization of the MMA pseudoaneurysm to prevent secondary rupture.
Figure 2: (A) Short follow-up axial non-enhanced head CT scan showing interval increase in the extra-axial hematoma and the subarachnoid hemorrhage. (B) Axial contrast-enhanced CT scan of the head (arterial phase) showing a pseudoaneurysm formation at the level of the left middle meningeal artery. Note is made of asymmetrical prominence and early opacification of the veins of the left infratemporal fossa, secondary to arterio-venous fistula.
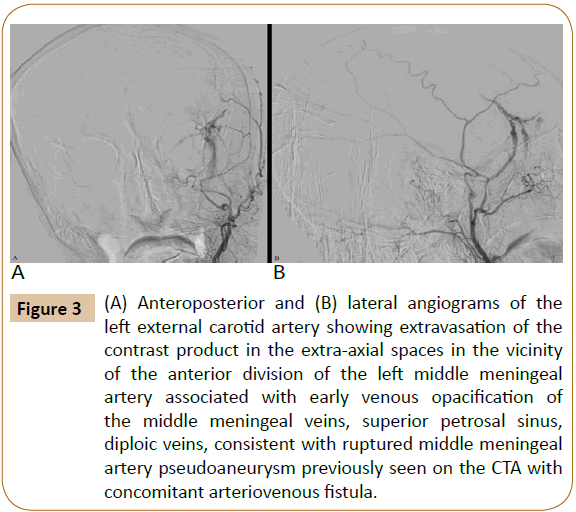
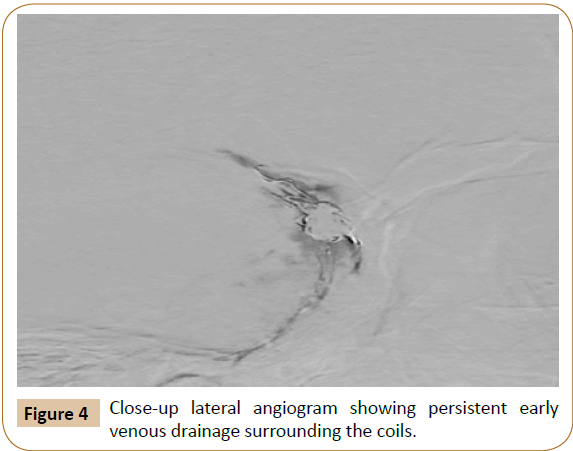
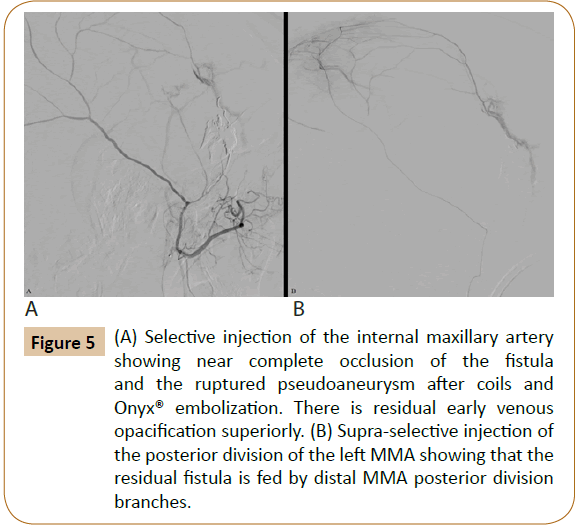
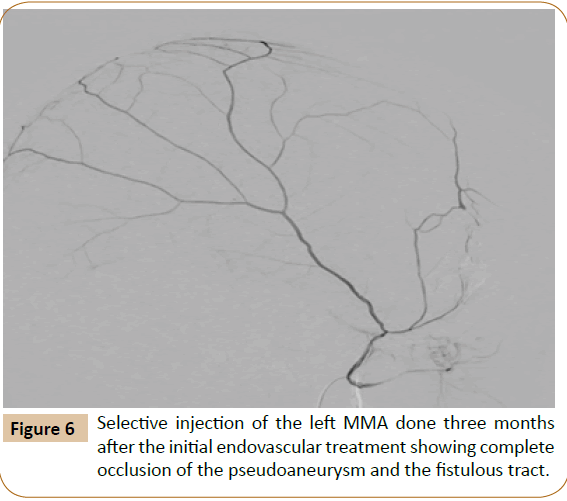
Angiogram of the left external carotid artery through a 6 French guiding catheter showed interval rupture of the middle meningeal artery pseudoaneurysm previously seen on the CTA with extravasation of the contrast product into the adjacent extraaxial spaces. In addition, there was early venous drainage in the accompanying middle meningeal veins, superior petrosal sinus, and diploic veins consistent with concomitant arteriovenous fistula of the MMA (Figure 3). There was no evidence of cortical Catheterization of the anterior division of the left middle meningeal artery and then the pseudoaneurysm was performed using 0.012-inch microwire and Echelon TM 10 Microcatheter (ev3, Irvine, California, USA). Coiling of the pseudoaneurysm, as well as the parent artery proximal and distal to the aneurysm, was performed using Micrus coils (Codman Neuro, Micrus Endovascular Microcoil System, Raynham, MA), with a total coil length of 186 cm. Control angiogram showed persistent early venous drainage (Figure 4). After priming the microcatheter with DMSO, 1.5 ml of Onyx® (Ethylene vinyl alcohol copolymer- EV3, Irvine-CA) was slowly injected over 15 minutes into the coil meshwork until Onyx® cast was seen into the foot of the draining veins of the fistula. Control angiogram showed near complete occlusion of the aneurysm and the fistula with persistent small fistulous component fed by small distal feeders coming from the posterior division of the MMA (Figure 5). This residual shunting was not present on the follow angiogram done 12 weeks later (likely spontaneously thrombosed) (Figure 6). The patient's neurological condition improved over the course of his hospitalization. He was discharged to a rehabilitation center with no focal neurological deficit.
Figure 3: (A) Anteroposterior and (B) lateral angiograms of the left external carotid artery showing extravasation of the contrast product in the extra-axial spaces in the vicinity of the anterior division of the left middle meningeal artery associated with early venous opacification of the middle meningeal veins, superior petrosal sinus, diploic veins, consistent with ruptured middle meningeal artery pseudoaneurysm previously seen on the CTA with concomitant arteriovenous fistula.
Figure 5: (A) Selective injection of the internal maxillary artery showing near complete occlusion of the fistula and the ruptured pseudoaneurysm after coils and Onyx® embolization. There is residual early venous opacification superiorly. (B) Supra-selective injection of the posterior division of the left MMA showing that the residual fistula is fed by distal MMA posterior division branches.
Discussion
The Middle Meningeal Artery (MMA) runs along a bone groove in the inner surface of the skull, making it vulnerable to injury in the setting of head trauma and skull fractures [6]. MMA injury occurred in 4% of cases in a study involving 446 angiograms of patients with head trauma [1]. MMA injury usually results in extravasation of blood in the epidural space forming an epidural hematoma. However, early clotting, pseudoaneurysm formation or diversion of blood into the adjacent veins through an arteriovenous fistula, may delay or restrict the epidural hematoma formation [2].
MMA pseudoaneurysms are false aneurysms containing none of the normal arterial wall structures [4,6]. They are formed when a full thickness tear of the MMA wall does not result in free hemorrhage but by a surrounding hematoma that ultimately organizes, becomes walled off and maintains some communication with the parent arterial lumen [2]. Traumatic pseudoaneurysms of the MMA are associated with a skull fracture that crosses the MMA groove in up to 90% of the cases [5,7,8]. They are usually present at the anterior branch of the MMA, distant from a branching point. They characteristically lack a neck and show slow filling on the arterial phase and delayed washout on the venous phase on angiogram [5,9].
MMA Arteriovenous Fistula (AVF) occurs when there is a concomitant injury of the middle meningeal artery or its branches and the adjacent veins or dural sinuses. The venous drainage may be through the accompanying middle meningeal veins, the petrosal sinuses, the sphenoparietal sinuses, superior sagittal sinus, cavernous sinus, the diploic veins or even cerebral cortical drainage [1,3,10]. MMA AVF is a rare injury; it was found in 8 out of 446 patients (1.8%) who underwent cerebral angiograms for head trauma [1].
Although traumatic pseudoaneurysms and arteriovenous fistula of the middle meningeal artery share the same etiological mechanism, which is a tearing of the middle meningeal artery, their coexistence is very rarely reported. To the best of our knowledge, only a handful of case reports are present in the English-speaking literature [11-14]. The natural history of these lesions is not well known. Although there are some cases of MMA fistula or pseudoaneurysms that remain asymptomatic or resolved spontaneously, these lesions have generally poor prognosis and should be regarded as high-risk vascular lesions because of the risk of rupture [3,7,10,15-17]. Pseudoaneurysms are especially considered unstable because of the poor support of the aneurysmal wall. They tend to progressively increase in size and ultimately rupture leading to delayed intracranial bleeding [12,5,18-22]. Rupture of the MMA aneurysms may result in intra-axial and/or extra-axial bleeding depending if there is a breach of the sub-adjacent meningeal layers. Epidural, subdural, subarachnoid, intra-cerebral, or intra-ventricular hemorrhages were all reported as a result of pseudoaneurysm rupture [1,23,24].
The interval between trauma and aneurysmal rupture can range from days to months. Most of the ruptures occurred within the first 4 weeks of reported cases [5,8,24]. In our case, the rupture occurred between the CT angiography and the cerebral angiography (in less than 10 hours), which is to our knowledge the shortest reported secondary MMA pseudoaneurysm rupture.
The fast growth rate and high risk of re-bleeding associated with pseudoaneurysms and less commonly with arteriovenous fistula have led to recommendations for aggressive treatment. Endovascular treatment is considered the first line treatment of both pseudoaneurysms and arteriovenous fistula in the absence of significant intracranial bleeding and mass effect. Embolization of the aneurysm using coils, N-Butylcyanoacrylate (NBCA), Onyx®, gelatin sponge plugs, and Polyvinyl Alcohol Particles (PVA) has been described with successful results [13,25-29]. However, there is no general agreement on the specific embolic agent to use because of the rarity of these lesions [28]. However, embolic materials should be selected carefully depending on the type and size of the lesions to prevent complications and recanalization. In our case, coil embolization was performed first to reduce the shunting flow of the AVF and to occlude the pseudoaneurysm, followed by liquid embolic to occlude the fistulous tract.
Surgical treatment of the pseudoaneurysm is another treatment option especially if there is associated epidural hematoma and mass effect [7]. It may include clipping, ligation or trapping of the pseudoaneurysm and/or the artery. Surgery is associated with higher mortality and morbidity and may not be possible in all cases [7,14]. In addition, in the setting of arteriovenous fistula, ligation of the feeding arteries may not be complete with potential development of other collaterals and the subsequent recanalization of the fistula [28].
Conclusion
Middle meningeal artery pseudoaneurysms and arteriovenous fistula are critical traumatic vascular injuries because of the high risk of secondary rupture and intracranial bleeding. A high index of suspicion should be maintained in the setting of head trauma with a skull fracture, intracranial hematoma or in case of delayed neurological deterioration after a lucid interval. Endovascular therapy provides minimally invasive and definitive treatment of both conditions and should be considered for patients having either or both conditions.
References
- Freckmann N, Sartor K, Hermann HD (1981) Traumatic arteriovenous fistulae of the middle meningeal artery and the neighbouring veins or dural sinuses. Acta Neurochir 55: 273-281.
- Handa J, Shimizu Y, Handa H (1970) Traumatic aneurysm and arteriovenous fistula of the middle meningeal artery. Clin Radiol 21: 39-41.
- Almefty M, Yashar S, Kalani YS, Ducruet AF, Crowley RW, et al. (2016) Middle meningeal arteriovenous fistulas: A rare and potentially high-risk dural arteriovenous fistula. Surg Neurol Int 7: S219-S222.
- Holmes B, Harbaugh RE (1993) Traumatic intracranial aneurysms: A contemporary review. J Trauma 35: 855-860.
- Bruneau M, Gustin T, Zekhnini K, Gilliard C (2002) Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage: Case report and literature review. Surg Neurol 57: 174-178.
- Yu J, Guo Y, Xu B, Xu K (2016) Clinical importance of the middle meningeal artery: A review of the literature. Int J Med Sci 3:790-799.
- Parkinson D, West M (1980) Traumatic intracranial aneurysms. J Neurosurg 52: 11-20.
- Wang CH, Lee HC, Cho DY (2007) Traumatic pseudoaneurysm of the middle meningeal artery: Possible indicators for early diagnosis in the computed tomography era. Surg Neurol 68: 676-681.
- Higazi I, El-Banhawy A, El-Nady F (1969) Importance of angiography in identifying false aneurysm of the middle meningeal artery as a cause of extradural hematoma: Case report. J Neurosurg 30: 172-176.
- Chandrashekar HS, Nagarajan K, Srikanth S, Jayakumar P, Vasudev M (2007) Middle meningeal arteriovenous fistula and its spontaneous closure: A case report and review of the literature. Intervent Radiol 13: 173-178.
- Sicat LC, Brinker RA, Abad RM, Rovit RL (1975) Traumatic pseudoaneurysm and arteriovenous fistula involving the middle meningeal artery. Surgical Neurology 3: 97-103.
- Ko JH, Kim YJ (2014) Traumatic pseudoaneurysm of the middle meningeal artery with an arteriovenous fistula on a non-fractured site. Intervent Neuroradiol 20: 352-356.
- Roski RA, Owen M, White RJ, Takaoka Y, Bellon EM (1982) Middle meningeal artery trauma. Surg Neurol 17: 200-203.
- Tsutsumi M, Kazekawa K, Tanaka A, Ueno Y, Nomoto Y, et al. (2002) Traumatic middle meningeal artery pseudoaneurysm and subsequent fistula formation with the cavernous sinus: Case report. Surg Neurol 58: 325-328.
- Chedid MK, Vender JR, Harrison SJ, McDonnell DE (2001) Delayedappearance of a traumatic intracranial aneurysm. Case report and review of the literature. J Neurosurg 94: 637-641.
- Luciani A, Houdart E, Mounayer C, Saint Maurice JP, Merland JJ (2007) Spontaneous closure of dural arteriovenous fistulas: Report of three cases and review of the literature. J Neurosurg 22: 992-996.
- Moriya M, Itokawa H, Fujimoto M, Noda M, Nagashima G, et al. (2007) Spontaneous closure of dural arteriovenous fistula after performing diagnostic angiography. Neurol surg 35: 65-70.
- Okumura H, Tenjin H, Ueda S (1998) A case of traumatic pseudoaneurysm of the middle meningeal artery treated with endovascular surgery. Neurol surg 26: 929-933.
- Lim DH, Kim TS, Joo SP, Kim SH (2007) Intracerebral hematoma caused by ruptured traumatic pseudoaneurysm of the middle meningeal artery: A case report. J Korean Neurosurg 42: 416-418.
- Lee JY, Lee CY, Kim HW (2014) Angiographically progressive change of traumatic pseudoaneurysm arising from the middle meningeal artery. J Korean Neurosurg 56: 423-427.
- Aoki N, Sakai T, Kaneko M (1992) Traumatic aneurysm of the middle meningeal artery presenting as delayed onset of acute subdural hematoma. Surg Neurol 37: 59-62.
- Jussen D, Wiener E, Vajkoczy P, Horn P (2012) Traumatic middle meningeal artery pseudoaneurysms: diagnosis and endovascular treatment of two cases and review of the literature. Neuroradiol 54: 1133-1136.
- Albert FK, Oldenkott P, Sigmund E (1989) Subarachnoid hemorrhage and intracerebral hematoma in injury of the middle meningeal artery. Zentralbl Neurochir 50: 153-156.
- Buckingham M, Crone K, Ball W, Tomsick T, Berger T, et al. (1988) Traumatic intracranial aneurysms in childhood: two cases and a review of the literature. Neurosurg 22: 398-408.
- Khattar NK, White AC, Fortuny EM, Hruska RT, James RF (2017) Management of unruptured traumatic middle meningeal artery pseudoaneurysms through onyx embolization. Cureus 9: e1794.
- Lesley WS, Thomas MR, Abdulrauf SI (2004) N-butyl cyano acrylate embolization of a middle meningeal artery aneurysm in a patient with neurofibromatosis type 2. Am J Neuroradiol 25: 1414-1416.
- Lama M, Mottolese C (2000) Middle meningeal artery aneurysm associated with meningioma. J Neurosurg 44: 39-41.
- Meder JF (1992) Traumatic aneurysms of the internal and external carotid arteries. One case and a review of the literature. J Neuroradiol 19: 248-255.
- Touho H, Furuoka N, Ohnishi H, Komatsu T, Karasawa J (1995) Traumatic arteriovenous fistula treated by superselective embolisation with microcoils: Case report. Neuroradiol 37: 65-67.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences