The Impact of Peripheral Artery Disease on Health Related Quality of Life: Comparison with the Impact of Coronary Artery Disease
Anthos Koureas, Mamas Theodorou and Alexis A Samoutis
DOI10.21767/2573-4482.100060
Anthos Koureas1,2*, Mamas Theodorou2 and Alexis A Samoutis3
1Vascular Surgery Department, Nicosia General Hospital, Cyprus
2Faculty of Economics and Management, Open University of Cyprus, Cyprus
3Frederick University of Cyprus, Cyprus
- *Corresponding Author:
- Anthos Koureas
Vascular Surgery Department
Nicosia General Hospital
Nicosia – Limassol Old Road, No. 215
2029 Strovolos, Cyprus
Tel: +35799371271
E-mail: akourea@cablenet.com.cy
Received Date: August 26, 2017; Accepted Date: Septembre 26, 2017; Published Date: Septembre 30, 2017
Citation: Koureas A, Theodorou M, Samoutis AA (2017) The Impact of Peripheral Artery Disease on Health Related Quality of Life: Comparison with the Impact of Coronary Artery Disease. J Vasc Endovasc Surg. 2:27. doi: 10.21767/2573-4482.100060
Abstract
Introduction: Peripheral artery disease is a common cardiovascular disease with high morbidity and mortality. The traditional objective parameters used to assess and guide the therapeutic interventions, poorly reflect the real effects from patients’ perspectives and their experience of living with peripheral artery disease. The importance of evaluating and improving quality of life has been recognized in several studies. Coronary artery disease is a more life-threatening cardiovascular disease. However, comparing coronary and peripheral artery disease, as to their impact on health related quality of life, has been controversial. The aim of this study was the assessment of health related quality of life in patients with peripheral artery disease and the investigation of relations and correlations with the objective criteria of illness. Moreover, the group of patients with peripheral arterial disease who were scheduled for surgical intervention was compared with the corresponding group of patients with coronary artery disease, as for the quality of life.
Methods: Symptomatic patients with peripheral artery disease (n=125) referred to the Vascular surgery service during a six month period were enrolled in this observational study of health related quality of life. Patients completed the short form-36 (SF-36) questionnaire and ankle-brachial index was measured at presentation. During the same period, patients with coronary artery disease who were scheduled for bypass surgery (n=43) were also enrolled in the study and health related quality of life was assessed using the same questionnaire.
Results: Patients with peripheral artery disease had significantly impaired health related quality of life, reporting low scores in all SF-36 domains. Markedly low they scored on the domain’s physical functioning, bodily pain, role limitations by physical problems and role limitations by emotional problems. The mean anklebrachial index was 0.57 (range, 0.30-0.90) exhibiting modest correlation with SF- 36 scores. Patients with peripheral artery disease who were scheduled for bypass surgery scored significantly (p<0.001) lower than relevant patients with coronary artery disease on the domains physical functioning, bodily pain and vitality.
Conclusions: Peripheral artery disease has negative impact on health related quality of life. Objective measures, as the ankle-brachial index, only partially reflect the quality of life of these patients. Compared with patients with coronary artery disease who are scheduled for surgery, patients with peripheral artery disease have similar or even greater negative impact on health related quality of life.
Keywords
Quality of life; SF-36; Ankle-brachial index; Peripheral artery disease; Coronary artery disease
Introduction
Peripheral artery disease (PAD) is a common chronic disease with a high morbidity and mortality rate. Like all cardiovascular diseases, PAD is owed to atherosclerosis systemic process and characterized by the presence of risk factors, such as smoking, hyperlipidemia, diabetes and hypertension. Clinical severity ranges from asymptomatic disease to intermittent claudication to critical limb ischaemia with potential tissue loss [1].
Traditionally, as definite cure is not possible, management of PAD patients aims to reduce cardiovascular events, prevent limb loss and improve functional status [2]. However, the increasing numbers of patients, the improvement of prognosis with long-term treatments and the use of modern therapeutic measures, reveal the insufficiency of clinical, anatomic and physiological criteria, to attribute the real effect of illness and the potential benefit to the patient [3]. Objective parameters, such as Fontaine classification and ankle-brachial index (ABI) measurements, poorly reflect the patient’s experience of living with PAD and often cannot be correlated with subjective illness feelings [4]. An extreme but common example in clinical practice is the improvement of some patients’ quality of life after amputation, in spite of their functional disability [5]. Thus, the evaluation of PAD effects from patients’ perspectives and the assessment of quality of life in order to understand the physical, psychosocial and emotional consequences of PAD, constitutes a modern challenge for health professionals. The importance of improvement in quality of life has been recognized in several studies and the TransAtlantic Inter-Society Consensus (TASC) suggested that accurate quality of life assessments should become an indispensable implement to guide and evaluate therapeutic options in patients with PAD [6].
Coronary artery disease (CAD) is also a common cardiovascular disease and the leading cause of death worldwide. Common risk factors, pathogenesis and treatment options of PAD and CAD confer a particular interest in comparing these two patient groups, with regard to health-related quality of life.
The aim of this study was to measure health-related quality of life (HRQOL) in patients suffering from PAD and investigates the correlation with objective disease criteria. The use of a validated and reliable generic questionnaire (SF-36), allowed comparison of the results with those of patients with CAD, which is generally regarded to be more life-threatening and have more impact on HRQOL. Especially for the two diseases comparison, they were selected patients with PAD and CAD who were scheduled for surgical intervention.
Short summary
Peripheral artery disease has a major negative impact on health related quality of life. The burden of disease is greater than that of coronary artery disease in patients scheduled for bypass surgery.
Methods
Patient selection and study design
All patients referred to the Vascular Laboratory and the Outpatients Department of Vascular Surgery Clinic of Nicosia General Hospital, Cyprus, between January and June 2015, with the diagnosis of chronic symptomatic peripheral artery disease (PAD), was considered for this observational study. During the same period, patients with the diagnosis of coronary artery disease (CAD) referred to Cardiothoracic Surgery Clinic of Nicosia General Hospital for surgical intervention (CABG), were enrolled in the study. Patients with recent acute cardiovascular events were excluded from the study, so that the answers for their chronic disease are not influenced by the emergency character of an acute event. Greek was the first language of all patients involved in this study, in order to ensure that they could read, write and clearly understand the questionnaires. Written informed consent was obtained from each patient participating in this study.
Data sources
Data sources consisted of medical records and patient questionnaires. Information on demographic and socioeconomic characteristics, such as age, marital status, educational level, occupational status and income was registered for all patients. Data also included clinical characteristics, risk factors, comorbid conditions, previous operations and treatment plans.
Patients with PAD were classified in stages according to the Fontaine scale (Fontaine stage II-IV). Resting ABIs were obtained in all PAD patients. ABI was calculated for each symptomatic extremity, with the highest Doppler-derived systolic pressure at the ankle (dorsalis pedis or posterior tibial artery), indexed to the highest Doppler- derived brachial artery pressure. The index of the most diseased leg of each patient was used for statistical analysis.
Patients with CAD were classified according to the Canadian Cardiovascular Society Angina Grading Scale (CCS I-IV).
Quality of life measurement
Health related quality of life was measured with the Short Form 36 (SF-36) Health Status Survey, a validated, reliable and relatively simple generic tool. The SF-36 is the most widely used questionnaire and has been suggested as the standard instrument in vascular studies [7,8]. As a generic survey, it allows comparisons across many patient populations and different disease entities [9]. This 36-item questionnaire, measures eight domains of health related quality of life: Physical Function, Role Limited by Physical Health, Bodily Pain, General Health, Vitality, Social Function, Role Limited by Emotional Health and Mental Health [10]. The Greek translation of SF-36 health survey has been validated and the results supported the use of the instrument in studies involving Greek samples [11-13].
The standard SF-36 questionnaires (Greek version 1.0) were completed via face to face interview in order to enhance patients’ understanding and minimize missing values. Scores for each subscale item were recorded, summed and transformed, using the original 0-100 algorithms, into a scale from 0 to 100, with higher scores indicating a better quality of life.
Data analysis
Statistical analysis was performed using SPSS 16.0 for Windows software. Descriptive statistics including frequencies and means and correlation analysis were conducted. The Student’s t-test was used to compare our scores against published norms and between different patient groups (PAD vs. CAD). Correlation between ABI and PAD patients’ quality of life was determined by calculation of Pearson’s correlation coefficient. ANOVA and Post Hoc tests were applied to compare the course of quality of life between patient groups. A p-value of <0.05 was considered statistically significant.
Results
A total of 125 patients with PAD participated during the 6-month study period. Average age was 68.2 years (range 48-85) and 88% of patients were male. Demographic data of the PAD group are shown in Table 1. Eighty two patients (65.6%) had retired from work, 67.2% were married, whilst 47.2% had secondary education.
| Characteristic | No. (%) |
|---|---|
| Age (years) | |
| Under 50 | 3 (2.4) |
| 50-59 | 18 (14.4) |
| 60-69 | 47 (37.6) |
| 70-79 | 43 (34.4) |
| 80-89 | 14 (11.2) |
| Sex | |
| Male | 110 (88) |
| Female | 15 (12) |
| Marital Status | |
| Married | 84 (67.2) |
| Widowed | 27 (21.6) |
| Divorced | 12 (9.6) |
| Single | 2 (1.6) |
| Educational Level | |
| No education-Primary | 53 (42.4) |
| Secondary | 59 (47.2) |
| Tertiary | 13 (10.4) |
| Occupational Status | |
| Retired | 82 (65.6) |
| Unable to work | 12 (9.6) |
| Full-time | 23 (18.4) |
| Family Income (Monthly) | |
| < €1000 | 69 (55.2) |
| €1001-2000 | 38 (30.4) |
| €2001-3000 | 3 (2.4) |
| >€3000 | 15 (12) |
Table 1: Demographic Data of 125 patients with Peripheral Arterial Disease.
The clinical characteristics of all PAD patients are presented in Table 2. Most patients had hypertension and hyperlipidemia. Fifty four percent were diabetic and nearly 82% were current or former smokers. The mean ABI was 0.57 (range 0.3-0.9).
| Characteristic | No. (%) |
|---|---|
| Risk Factors | |
| Hypertension | 109 (87.2) |
| Hyperlipidemia | 106 (84.5) |
| Diabetes mellitus | 68 (54.4) |
| Smoking Status | |
| Never | 23 (18.4) |
| Former | 69 (55.2) |
| Current | 33 (26.4) |
| Comorbid Diseases | |
| Coronary Artery Disease (CAD) | 52 (41.6) |
| KidneyDisease | 17 (13.6) |
| History of myocardial infarction | 32 (25.6) |
| History of stroke | 4 (3.2) |
| Clinical PAD stage (Fontaine) | |
| IIa | 45 (36) |
| IIb | 28 (22.4) |
| III | 24 (19.2) |
| IV | 28 (22.4) |
| Treatment Plan | |
| Peripheral bypass | 41 (32.8) |
| Conservative | 22 (17.6) |
| Angioplasty | 21 (16.8) |
| Angiography | 41 (32.8) |
Table 2: Clinical characteristics of 125 patients with Peripheral Artery Disease.
All patients with PAD in this study reported low SF-36 scores. Markedly low they scored on the domain’s physical functioning, bodily pain, role limitations by physical problems and role limitations by emotional problems. The mean scores of the eight SF-36 dimensions are shown in Table 3. The results were compared with the normative data of Greek general population due to lack of available data for Cypriot population. PAD patients’ results were significantly lower in every domain of health related quality of life (all p<0.001, Student’s t-test).
| SF-36 subscales | score (%) | standard deviation (SD) |
|---|---|---|
| Physical Functioning (PF) | 32.68 | 24.73 |
| Role Physical (RP) | 22.2 | 32.41 |
| Bodily Pain (BP) | 31.53 | 25.44 |
| General Health (GH) | 43.22 | 20.17 |
| Vitality (VT) | 40.92 | 23.48 |
| Social Functioning (SF) | 47.1 | 31.11 |
| Role Emotional (RE) | 34.13 | 42.21 |
| Mental Health (MH) | 50.62 | 25.33 |
Table 3: Scores by domains of SF-36 in 125 PAD patients.
The relation between ankle-brachial index (ABI) and quality of life was investigated with the use of correlation coefficients. The correlation between each SF-36 subscale and ABI, reached statistical significance (p-value< 0.05). Pearson correlation coefficient was moderate with values ranges from 0.29 in the subscale of Emotional Role, to 0.69 in the subscale of Physical Functioning. Generally, higher values were recorded in the subscales related to physical health, namely Physical Function (r=0.69), Physical Role (r=0.48) and Bodily Pain (r=0.64), while lower correlations were recorded in the subscales of Social Functioning (r=0.38) and Emotional Role (r=0.29).
During the same study period, 43 patients with the diagnosis of CAD were referred for CABG at the Cardiothoracic Clinic of the same hospital and they were enrolled in the study. This group was numerically similar to the subgroup of patients with PAD who were also scheduled for surgical revascularization. The same demographic data and clinical characteristics were registered for all CAD patients who were classified according to the Canadian Cardiovascular Society Angina Grading Scale (CCS I-IV).
Average age of the CAD group was 59.1 years (range 38-79) and 80.5% of patients were male. As in the PAD group, most CAD patients had hypertension (93%) and hyperlipidemia (83.7%). All the clinical characteristics and CCS classification are presented in Table 4. Scores for all SF-36 subscales were low, indicating the disease burden of coronary artery disease in patients scheduled for CABG. Markedly low scores were shown for role limitations by physical problems (34.14%) and for role limitations by emotional problems (28.45%).
| Characteristic | No. (%) |
|---|---|
| Risk Factors | |
| Hypertension | 40 (93) |
| Hyperlipidemia | 36 (83.7) |
| Diabetes mellitus | 27 (62.7) |
| Current Smoker | 19 (44.1) |
| Comorbid Diseases | |
| Peripheral Artery Disease (PAD) | 5 (11.6) |
| KidneyDisease | 7 (16.2) |
| History of myocardial infarction | 22 (51.6) |
| History of stroke | 3 (6.9) |
| CCS Angina Grading Scale stage | |
| I | 17 (39.5) |
| II | 7 (16.2) |
| III | 12 (27.9) |
| IV | 7 (16.2) |
Table 4: Clinical characteristics of 43 patients with Coronary Artery Disease.
Comparison of HRQOL in PAD and CAD
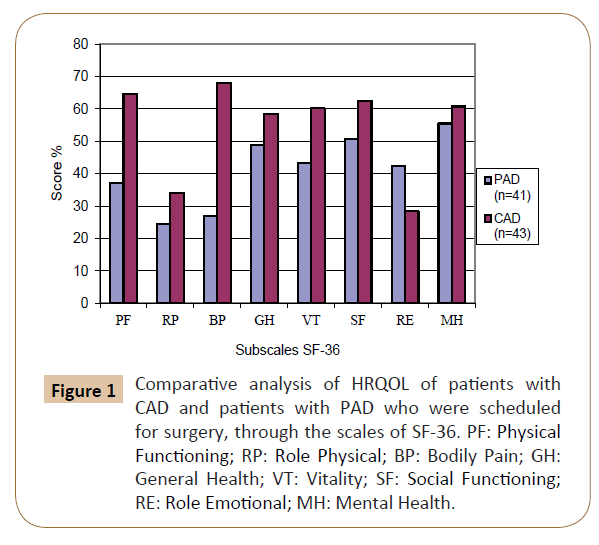
In order to investigate the impact of CAD and PAD on HRQOL, the results of SF-36 questionnaires of the 43 patients with CAD who were scheduled for CABG, were compared with the corresponding results of the 41 patients with PAD who were scheduled for peripheral bypass revascularization. In three domains the group of patients with PAD scored significantly lower than CAD patients. Overall, PAD patients had lower scores on physical functioning (37.19% versus 64.75%; p<0.001), bodily pain (26.92% versus 67.97%; p<0.001) and vitality (43.29% versus 60.24%; p<0.001). The scores of all SF-36 domains for both, scheduled for surgical revascularization, CAD and PAD patients are listed in Figure 1.
Figure 1: Comparative analysis of HRQOL of patients with CAD and patients with PAD who were scheduled for surgery, through the scales of SF-36. PF: Physical Functioning; RP: Role Physical; BP: Bodily Pain; GH: General Health; VT: Vitality; SF: Social Functioning; RE: Role Emotional; MH: Mental Health.
Discussion
The present study shows the significant reduction of HRQOL in both PAD and CAD patients. The total PAD sample was 125 patients and the vast majority of them were men (n=110, percentage 88%). Although, based on the international literature the prevalence of the disease presents a relationship men-woman 3:1, our 9:1 finding is found in many other similar studies [14-16]. The average age of PAD patients in the sample was 68.2 years and the largest concentration occurred in the age group 75- 79 years old, matching the bibliographic data and confirming the incidence and prevalence increase of the disease by age [6,17].
The positive correlation with risk factors such as smoking, hypertension, diabetes mellitus and hyperlipidemia, is confirmed by the presence of high levels of these factors in PAD patients. At the same time, the coexistence of other cardiovascular diseases is evident in patients with peripheral artery disease and rates of co-morbidity comply with the corresponding figures of other studies. The high percentage of patients with PAD and CAD was shown in several studies such as the REACH study, which included 8273 patients with PAD, half of them also having CAD [18]. The findings of our study also agree with the research paper of Bekos et al., which involved 556 Cypriot patients of whom 41,8% had both PAD and CAD [19].
The results of the health survey SF-36, for the sample of 125 patients with peripheral artery disease, are extremely low. The scales that reflect physical, functional status of patients, i.e. the scales of Physical Function, Bodily Pain and Role limitation by physical problems presented more influenced, indicating the great effect of the disease in these areas of HRQOL.
Comparing the results of the sample with the general population of Attica (Greece) [13], patients with PAD show consistently lower scores at all 8 scales of SF-36. Statistical analysis proves the existence of statistically significant differences in the comparison groups, with the p-value less than 0.001 for all scales. The results are expected, as based on the international literature, the quality of life of patients with PAD is affected in all areas [3]. The heterogeneity of various researches in this field, with regard to the questionnaire used, but also to the population of each sample, makes direct comparisons difficult. For the comparison of quality of life scales’ scores, corresponding studies using SF-36 questionnaire were selected, enabling numerical comparison of different scales. The existence of differences in studies’ populations was inevitable, as some studies included only patients with intermittent claudication, others only patients with critical ischaemia, some included patients who underwent surgery or angioplasty and some included both symptomatic and asymptomatic patients with PAD. The main conclusions of these studies, demonstrate the relevance of the results and their variation at roughly the same levels [14,20-23]. The results show the serious impact of PAD in all areas of quality of life and mainly at scales that describe the physical state. The differences in the scores of various studies are due to the diversity of samples, particularly regarding the severity and stage of disease.
In this study the Ankle-Brachial Index of patients with PAD shows a moderate correlation with the 8 scales of the SF-36. The above findings agree with the majority of similar studies that investigated the relationship of objective criteria of PAD with quality of life in this group of patients. Izquierdo-Porrera et al., [20] showed the existence of statistical significance in correlation of ABI and quality of life, at 3 of the 8 scales of SF-36 relating to physical health, demonstrating moderate rank correlations. Long et al., [21] investigated the relationship of ABI with the 2 Summary scales of SF-36. Physical Component Summary (PCS) showed moderate correlation, while Mental Component Summary (MCS) didn’t have any correlation. Freiglass et al. [24], recorded even less correlation of ABI with the scale of Physical Function of SF-36. Muller-Buhl et al. [4] in their own study, concluded that there is a small correlation of ABI with quality of life and the existence of statistically significant correlation, regarding only the scale of pain. As can be seen from the comparison of findings of various studies, the relationship between ABI and quality of life is not strong neither absolute. The degree of correlation is low or moderate and often do not cover all scales. In this study, although values of Pearson coefficient vary within the limits of moderate correlations, however presented higher than other published studies. Differences in the composition of sample of each study can warrant the small diversification of results. All the above studies involved patients with intermittent claudication (Fontaine IIa and IIb), while the present study also includes patients with critical lower limb ischaemia (Fontaine III and IV).
PAD and CAD Patients who were Scheduled for Surgery
PAD and CAD are chronic cardiovascular diseases with common pathogenesis and almost absolute correlation with the process of atherosclerosis. In the context of this study, patients with PAD and patients with CAD who were scheduled for surgery, considered comparable populations, with the use of the general quality of life measurement tool SF-36. The results demonstrate that both categories of patients show significant decline in the quality of life in its entirety. Patients with PAD have even more reduced levels of HRQOL than patients with CAD. These results are consistent with the literature, although contradict the general perception of greater impact of CAD on QOL, which is based on the fact that it is more life-threatening.
The small difference in mean age between PAD and CAD patients might have affected the results, despite the fact that differences between groups remain when age differences are statistically controlled. However, unlike patients with PAD, patients with CAD showed relatively high scores on the scale of physical function, that is an objective parameter, while in contrast exhibit remarkably low score on the scale of body role limitations due to physical problems. Obviously, these patients believed that CAD constrains them physically, although objectively their natural condition is not much affected. These findings agree with those of De Graff et al. [22] who suggested that patients with PAD have a reduced HRQOL in comparison with patients with CAD. Statistically significant differences exist mostly in the scales of Physical Function, Bodily Pain and General Health with PAD group scoring lower values. Similar results are noted at scales not emerging statistical significance, except for Emotional Role that shows the lower value in the group of patients with CAD, unlike the results of De Graff et al. The fact that our comparison concerned patients who were scheduled for surgery affected their emotional status and created anxiety and concern. Although the group of patients with PAD was also scheduled for surgery, CABG is a long, risky operation, with more complications and higher mortality. These parameters are reflected in limiting the role due to emotional problems, especially in this group of CAD patients.
Study Limitations
One limitation of the study was the small number of patients in the sample which limited the potentiality for statistical analysis, particularly with regard to socio-economic and demographic characteristics. In addition, the lack of available information about the quality of life of general population restricted validity of the results. Another limitation was the non-existence of translated and standardized specific questionnaire on the quality of life of patients with PAD, in Greek, that could be used in parallel with SF-36 for the fullest representation of the quality of life in this group of patients.
Conclusion
Peripheral artery disease has a negative impact and causes significant decrease in the quality of life of patients, in all aspects of both physical and mental health. The clinical features of the disease and the laboratory measurements only partially reflect the quality of life of these patients. Compared with patients with CAD who are scheduled for surgery, patients with PAD have similar or even greater negative impact on HRQOL. The findings of this study agree with previous studies, indicating that the quality of life is an important aspect of treatment in patients with peripheral artery disease and may be a new therapeutic target, apart from classical established standards. Health-related quality of life in patients with peripheral artery disease will continue to be used and gradually established as an endpoint therapeutic outcome. The continuous and systematic assessment of the quality of life will help doctors better understand the effects of the disease, promoting the adoption of best clinical decisions and applying more effective therapeutic approaches.
References
- Meijer WT, Grobbee DE, Hunink MG, Hofman A, Hoes AW (2000) Determinants of peripheral arterial disease in the elderly: The Rotterdam study. Arch Intern Med 160: 2934-2938.
- York JW, Taylor SM (2010) Lower Extremity Arterial Disease: Decision Making and Medical Treatment. In: Cronenwett JL, Johnston KW, Rutherford’s Vascular Surgery. (7th Edn), Saunders Elsevier, Philadelphia pp: 1593-1612.
- Liles D, Kallen M, Petersen L, Bush R (2006) Quality of Life and Peripheral Arterial Disease. J Surg Res 136: 294-301.
- Muller-Buhl U, Engeser P, Klimm HD, Wiesemann A (2003) Quality of life and objective disease criteria in patients with intermittent claudication in general practice. Family Practice 20: 36-40.
- Nehler M, McDermott M, Treat-Jacobson D, Chetter I, Regensteiner J (2003) Functional outcomes and quality of life in peripheral arterial disease: current status. Vasc Med 8: 115-126.
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, et al. (2007) Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Sur.
- Regensteiner JG, Hiatt WR, Coll JR (2008) The impact of peripheral arterial disease on health related quality of life in the Peripheral Arterial Disease Awareness, Risk, and Treatment: New Resources for Survival (PARTNERS) Program. Vasc Med 13: 15-24.
- Beattie DK, Golledge J, Greenhalgh RM (1997) Quality of life assessment in vascular disease: towards a consensus. Eur J Vasc Endovasc Surg 13: 9-13.
- Ware JE (1995) The status of health assessment 1994. Annu Rev Public Health 16: 327-354.
- Ware JE, Gandek B (1998) Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 51: 903-912.
- Kontodimopoulos N, Fragouli D, Pappa E, Niakas D (2004) Statistical tests of the validity and reliability of the Greek SF-36. Archives of Hellenic Medicine 21: 451-462.
- Pappa E, Kontodimopoulos N, Niakas D (2005) Validating and norming of the Greek SF-36 Health Survey. Quality of Life Research 14: 1433-1438.
- Pappa E, Kontodimopoulos N, Niakas D (2006) Psychometric evaluation and normative data for the Greek SF-36 health survey using a large urban population sample. Archives of Hellenic Medicine 23: 159-166.
- Tretinyak A, Lee E, Kuskowski M, Caldwell M, Santilli S (2001) Revascularization and Quality of life for patients with limb-threatening ischemia. Ann Vasc Sur 15: 84-88.
- Seabrook GR, Cambria RA, Freischlag JA, Towne JB (1999) Health-related quality of life and functional outcome following arterial reconstruction for limb salvage. Cardiovasc Surg 7: 279-286.
- Falnita L, Cocora M, Nechifor D, Socoteanu I, Bordos D (2004) Quality of life in patients with peripheral arterial disease before and after surgical treatment. TMJ 54: 346-353.
- Muir LR (2009) Peripheral arterial disease: Pathophysiology, risk factors, diagnosis, treatment, and prevention. J Vasc Nurs 27: 26-30.
- Bhatt DL, Steg PG, Ohman EM (2009) International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 295: 180-189.
- Bekos C, Pieri L, Angelides N, Moros I (2008) Prevalence of multifocal atherosclerosis and comorbidity on symptomatic Cypriot inpatients. International Angiology 27: 419-425.
- Izquierdo-Porrera AM, Gardner AW, Bradham DD (2005) Relationship between objective measures of peripheral arterial disease severity to self-reported quality of life in older adults with intermittent claudication. J Vasc Surg 41: 625-630.
- Long J, Modrall JG, Parker BJ, Swann A, Welborn MB, et al. (2004) Correlation between ankle-brachial index, symptoms, and health-related quality of life in patients with peripheral vascular disease. J Vasc Surg 39: 723-727.
- De Graff CJ, Ubbink TD, Kools JC, Chamuleau S, Jacobs M (2002) The impact of peripheral and coronary artery disease on health related quality of life. Ann Vasc Surg 16: 495-500.
- De Vries M, Ouwendijk R, Kessels GA (2005) Comparison of generic and disease-specific questionnaires for the assessment of quality of life in patients with peripheral arterial disease. J Vasc Surg 41: 261-268.
- Feinglass J, McCarthy WJ, Slavensky R, Manheim LM, Martin GJ (1996) Effect of lower extremity blood pressure on physical functioning in patients who have intermittent claudication. The Chicago Claudication Outcomes Research Group. J Vasc Surg 24: 503-511.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences