Emergency Hybrid Repair of an Infected Pseudo-aneurysm of an Axillary Dialysis Necklace Graft
Smith G, Dunne J, Singh N, Fowler O, Wilkinson D, Mercer K and Bhasin N
DOI10.21767/2573-4482.100031
Smith G1*, Dunne J2, Singh N2, Fowler O3, Wilkinson D2, Mercer K2 and Bhasin N4
1Academic Vascular Surgery Unit, Hull York Medical School, UK
2Department of Vascular Surgery, Hull York Medical School, UK
3Vascular Radiology, Bradford Teaching Hospitals NHS Foundation Trust, Bradford Royal Infirmary, UK
4Department of Vascular Surgery, Calderdale and Huddersfield NHS Trust, UK
- *Corresponding Author:
- George Smith
Academic Vascular Surgery Unit, Hull York Medical School, UK.
Tel: +44 (0) 7951217396
E-mail: georgeedsmith@gmail.com
Received Date: May 16, 2016; Accepted Date: November 29, 2016; Published Date: December 07, 2016
Citation: Smith G, Dunne J, Singh N, et al. Emergency Hybrid Repair of an Infected Pseudo-aneurysm of an Axillary Dialysis Necklace Graft. J Vasc Endovasc Surg. 2016, 1:4. doi: 10.21767/2573-4482.100031
Abstract
Excision of infected synthetic haemodialysis grafts with arterial repair can be extremely challenging due to friable vessels. We present a case of an infected pseudo-aneurysm of a synthetic necklace dialysis graft, where surgical repair of the axillary artery was attempted but not technically feasible. Emergency endovascular covered stenting was performed and the patient has now been free of complications for 4 years. Placing covered stents at infected sites remains controversial but we support endovascular treatment as a viable alternative in the emergency management of infected pseudo-aneurysms related to synthetic grafts and report long term good results in this case.
Keywords
Necklace graft; Infected pseudo-aneurysm; Endovascular treatment; Axillary artery; AV fistula
Introduction
Synthetic grafts are placed for haemodialysis access in patients when other access options have been exhausted [1]. These synthetic grafts may act as a nidus for infection and ideal management is by excision and vessel repair [2]. Surgical repair may be challenging due to friable vessels secondary to the infection, and conventional practice avoids stent placement in an infected field. We report a case of a beta-haemolytic streptococcus group B infected pseudoaneurysm of an axillary arteriovenous dialysis necklace graft, managed by emergency endovascular covered stenting of the artery where surgery became complicated peri-operatively.
Report
A 41-year old lady was admitted acutely with a painful, tender swelling causing pain and numbness in the right arm at the site of a previously partially excised infected polytetrafluoroethylene (PTFE) necklace graft in the subclavicular region. She had a past medical history of spina bifida, stroke, end-stage renal failure including a failed renal transplant, and had a working right sapheno-popliteal AV fistula. She was apyrexial and haemodynamically stable with no signs of acute limb ischaemia. Laboratory results showed a raised neutrophil count of 9.62 × 109/L (normal range: 2.00–7.50 × 109/L) and elevated C-reactive protein count of >160 mg/L (normal range: <10). Emergency duplex scanning revealed a pseudo-aneurysm and emergency surgery was undertaken.
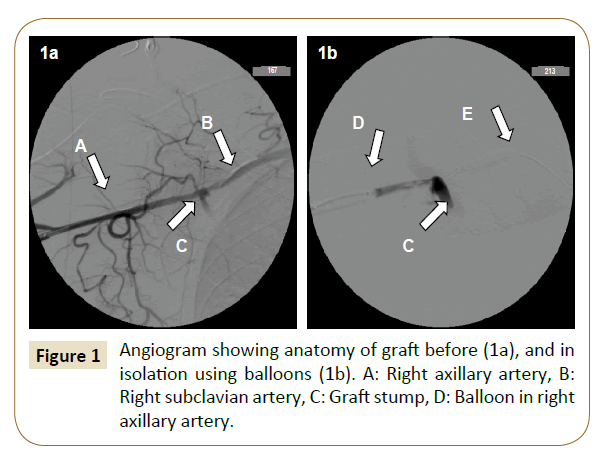
At operation the remnant stump of the necklace graft had detached from the native axillary artery and a pseudo-aneurysm was present. The stump and infected thrombus were removed and sent for microbiological investigation. Surgical repair of the axillary artery was attempted but was unsuccessful due to the artery being extremely friable. The sutures cut through the artery wall preventing the application of a vein patch. As an emergency salvage option, an endovascular approach was used. Angiography confirmed extravasation and the axillary artery were controlled with balloons, proximally via the right subclavian artery, through a femoral puncture, and distally via the right brachial artery (Figure 1).
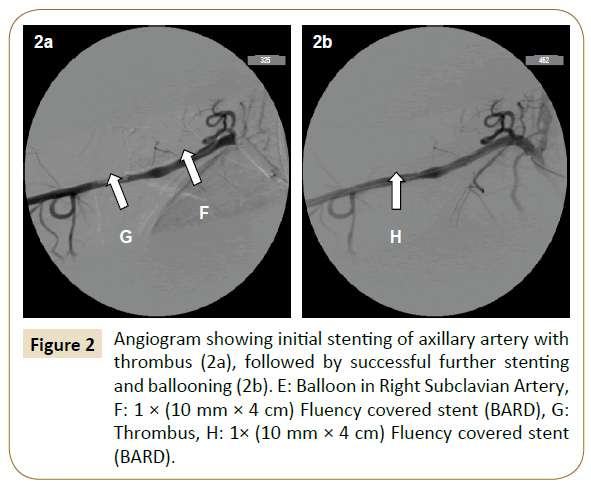
A 10 mm × 4 cm Fluency covered stent (BARD) was placed across the arterial defect. Check angiography confirmed significant intra-luminal stenosis distal to the stent, thought to be organized thrombus and therefore a second 10 mm × 4 cm Fluency covered stent was placed distal to, and overlapping the first (Figure 2). The overlapping area was dilated with an 8 mm × 4 cm balloon to give a good radiographic result, with good radial and ulnar pulses post-operatively.
Concerns of infection relating to the stent graft prompted a ten day course of intravenous benzyl-penicillin antibiotics postoperatively. At 4 years follow-up, no evidence of infective or other complications have been encountered.
Discussion
Infections of PTFE grafts implanted for vascular access may affect up to 35% of patients [3] and routine management is surgical excision. The repair of infected pseudo-aneurysms conventionally avoids implanting synthetic material due to the risk of persistent infection. A surgical approach has the advantage of debridement, and for this reason, employing a covered stent in repair is controversial.
Wong et al. recently published a series of 37 elective stent graft repair procedures for non-infected pseudo-aneurysms in access grafts with very respectable secondary patency rates despite relatively high rates of thrombosis (37.1%) post procedure [4]. Although their results did show safety and efficacy of stent graft repair of pseudo-aneursym repair in access grafts these were not placed in infected fields. It is recognized that patients requiring explanations of synthetic grafts may have poor vessel wall structure [5] making arterial repair extremely challenging. When surgical repair is not feasible in an emergency setting, endovascular repair represents an alternative, in spite of the risk of implanting foreign material in an infected field.
Previous reports of stenting in infected fields have yielded variable results. In a systematic review of 48 cases of stentgraft repair of mycotic aortic aneurysms, Kan et al. reported that a fifth of patients had persistent infection [6]. However, both this systematic review and other reports suggest there is potential for endovascular repair without complications of infection. Fu et al. reported a series of 15 intravenous drug users with pseudo-aneurysm relating to the femoral vessels treated with stent grafting with 10 of the 13 followed up not suffering infective complications [7]. Semba et al. published three cases of mycotic thoracic aortic aneurysm stent-graft repair without reinfection [8]. Stent grafting across an infected external iliac artery pseudoaneurysm has also been reported to be free of complications at 18 months [9] and coeliac pseudoanerysm due to tuberculosis has also been successfully treated in this fashion [10].
Another case report suggested much less favorable results stenting an infected coeliac axis pseudoanerysm which resulted in severe sepsis requiring operative intervention to retrieve the graft [11] though this case did involve an immune suppressed patient post organ transplant.
The case presented here supports the majority finding in related evidence in favor of the use of stent grafts in treating infected pseudo-aneurysms, not amenable to surgical repair, as a viable option in an emergency situation. Fears relating to future infective complications with this strategy do not seem to be borne out in the limited evidence currently available.
References
- Sidawy AN, Spergel LM, Besarab A (2008) The Society for Vascular Surgery: clinical practice guidelines for the surgical placement and maintenance of arteriovenous hemodialysis access. J Vasc Surg 48: 2S-25S.
- Kilic A, Arnaoutakis DJ, Reifsnyder T (2016) Management of infected vascular grafts. Vascu med (London, England) 21: 53-60.
- Anderson JE, Chang AS, Anstadt MP (2000) Polytetrafluoroethylene hemoaccess site infections. Asaio J 46: S18-S21.
- Wong WK, Su TW, Cheng WL (2016) Endovascular Stent Graft Repair is an Effective and Safe Alternative Therapy for Arteriovenous Graft Pseudoaneurysms. Eur J Vasc Endovasc Surg.
- Schutte WP, Helmer SD, Salazar L (2007)Surgical treatment of infected prosthetic dialysis arteriovenous grafts: total versus partial graft excision. Am J Surg 193:385-388.
- Kan CD, Lee HL, Yang YJ (2007) Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: a systematic review. J Vasc Surg 46:906-912.
- Fu Q, Meng X, Li F (2015) Stent-graft placement with early debridement and antibiotic treatment for femoral pseudoaneurysms in intravenous drug addicts. Cardiovasc Intervent Radiol 38:565-572.
- Semba CP, Sakai T, Slonim SM (1998) Mycotic aneurysms of the thoracic aorta: repair with use of endovascular stent-grafts. J Vasc Interv Radiol 9:33-40.
- Thrower AJ, Bhasin N, Kessel D (2004) Endovascular treatment of a MRSA infected left external iliac artery pseudoaneurysm. Eur J Vasc Endovasc Surg 27:673-675.
- Shu C, He H, Li QM (2010) Endovascular percutaneous treatment of tuberculosis pseudo-aneurysm involving the coeliac artery: a case report. Eur J Vasc Endovasc Surg 40:230-233.
- Akhtar MZ, Jones A, Sideso E (2011) Management of a ruptured mycotic pseudo-aneurysm following pancreas-kidney transplantation. Annal Transplant16:122-125.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences