Superior Mesenteric and Hepatic Artery Percutaneous Intervention by Left Radial Artery Approach in a Cachectic Patient with Severe Mesenteric Ischemia
Rafael Moguel Ancheita, Samaniego Mendez Virginia and Rosa Cristina Valencia Velazquez
DOI10.21767/2573-4482.18.03.9
Rafael Moguel Ancheita1*, Samaniego Méndez Virginia1 and Rosa Cristina Valencia Velazquez2
1The Clinics of the Heart, Cardiology, Cozumel, Quintana Roo, Mexico
2Internal Medicine Department, Hospital Costamed Tulum, Tulum, Quintana Roo, Mexico
- *Corresponding Author:
- Rafel Moguel Ancheita
The Clinics of the Heart, Cardiology, Cozumel, Quintana Roo, Mexico.
Tel: 525520684305
E-mail: cathboss@gmail.com
Received date: April 24, 2018; Accepted date: May 08, 2018; Published date: May 18, 2018
Citation: Ancheita RM, Virginia SM, Velazquez RCV (2018) Superior Mesenteric and Hepatic Artery Percutaneous Intervention by Left Radial Artery Approach in a Cachectic Patient with Severe Mesenteric Ischemia. J Vasc Endovasc Therapy. 3:9. doi: 10.21767/2573-4482.100079
Abstract
Chronic mesenteric ischemia is an under-recognized condition with every time more frequent diagnostic consideration due to improved imaging tools; its current treatment strategy includes surgical and percutaneous revascularization. The radial approach has not yet been published for the percutaneous modality.
A clinical case is presented with a 53 years old male with recent history of intense pain at swallowing with weight loss up to evident caquexia and prostration in bed; the patient had history of smoking, dyslipidemia, systemic arterial hypertension and, chronic systolic aortic murmur and family history of premature cardiac death.
He was hospitalized due to intense abdominal pain and the physical examination rendered an abdominal bruit; the abdominal arterial CT scan revealed complete ostial occlusion of the superior mesenteric artery (SMA); the hepatic branch of the coeliac trunk had severe stenosis and gave collateral circulation through the superior pancreaticoduodenal branch.
The treatment was performed through left radial artery approach with a 5 x 30 mm bare metal stent implantation in the origin of the SMA and angioplasty of the hepatic artery with the 5 x 30 mm balloon of the stent; the angiographic result obtained was good and was followed by immediate pain relief, complete tolerance to swallowing and feeding plus fast clinical recovery and weight gain.
The present case illustrates the feasibility of the percutaneous mesenteric revascularization through the access of the left radial artery.
Keywords
Mesenteric ischemia; Mesenteric artery; Superior hepatic artery; Celiac artery; Radial artery; Angioplasty
Introduction
The chronic mesenteric ischemia is a condition that has being considered rare in the past, but it has become more frequent as long as the diagnostic imaging is capable of demonstrate the obstruction of the mesenteric vessels; it is recognized as cause of death since 1875 [1].
Although it is not clear the incidence of this potentially lethal disease, the current concept is that it may be not so rare, yet it has been found in 6.8/100,000 persons per year in autopsies in Malmo Sweden [2]; in this publication it was found an incidence of 217/100,000 person per year in individuals aged 85 or older and that the clinical suspicion was only in 33% of the cases. The Minnesota population-based cohort study disclosed 22.9/100,000 persons per year with this problem [3].
It is known that the mesenteric circulation is very efficient, with a system that is supplied by three major arteries called the coeliac trunk, the superior mesenteric artery (SMA) and the Inferior mesenteric artery. The arterial net and the connections are so rich that the mesenteric perfusion is guaranteed in most cases and the appearance of ischemic symptoms needs at least two of these major vessels obstructed [4].
The etiology of the chronic mesenteric ischemia includes atherosclerosis in 95% of cases, with the same risk factors than atherosclerosis in other arterial segments but a minority may be secondary to vasculitis, coeliac trunk compression, fibrodysplasia, surgical removal of collateral vessels and external causes like hypovolemic conditions and heart failure; the diagnosis is sometimes difficult and is based in the symptoms that may include postprandial abdominal pain, fear to eat (sitophobia), weight loss, nausea, vomiting, bowel disorders (diarrheaconstipation) and the presence of atherosclerosis in other areas; the differential diagnosis includes many pathologies in and out the digestive system such as pyelonephritis, diverticulitis, gastric cancer, hiatal hernia, peptic ulcer, etcetera [5].
The laboratory tests are non-specific but may be related to malnutrition and the definitive diagnosis should be made by noninvasive image; the duplex-ultrasound can recognize high velocity Doppler signal [6] but the computed tomography angiography is a more reliable method when compared to ultrasound and magnetic resonance, with a described 96% sensitivity and 94% specificity [7,8].
The treatment of the chronic mesenteric ischemia is classically by surgical revascularization, but the recent endovascular treatment is feasible, and its less invasive modality gives the opportunity to the sicker patients due to long standing malnutrition as well as the patient with concomitant morbidities such as the very frequent coronary and cerebrovascular involvement. The surgical and endovascular revascularization has been compared in several reports that were analyzed by Pecoraro et al. they found significant less mortality and morbidity in the patients treated by endovascular revascularization but the same 5-year survival [9].
Case Report
We present a male patient that came to the hospital on May/2017 due to intense abdominal pain at rest; the patient had alternating intestinal constipation and diarrhea during the last month as well as severe abdominal pain at swallowing with fear to eat (sitophobia) and 9 Kg weight loss in the last month with caquexia and postration in bed; he was hospitalized three weeks before due to severe hypertension with pulmonary edema and was discharged with lisinopril and amlodipine.
The patient had clinical history of chronic bilateral claudication with progressive decline in the walking distance, severe systemic arterial hypertension, aortic sclerosis and heavy smoking (40 cigarettes per day); his father and grandfather had lethal myocardial infarction at young age.
The physical exam disclosed 57x’ heart rate, 21x’ respiratory rate, 178/57 mmHg blood pressure, 1.64 m height, 53 Kg weight, 19.7 body mass index, caquexia, aortic ejective murmur, evident abdominal bruit and bilateral absence of femoral pulses; the relevant laboratory results rendered leukocytosis (19.3K/μL), 32 mm/h globular sedimentation rate, 136 mg/L C-reactive protein and positive stools for Entamoeba hystolytica.
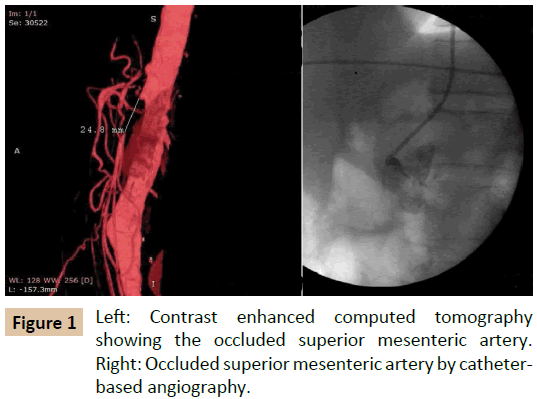
A contrast enhanced computer tomography showed chronic total occlusion in the origin of the SMA (Figure 1 left) and significant stenosis in the origin of the hepatic artery from the celiac trunk; it was found also bilateral common iliac artery stenosis and severe stenosis of the left renal artery.
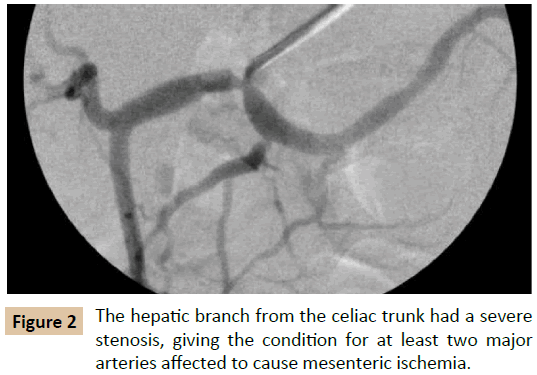
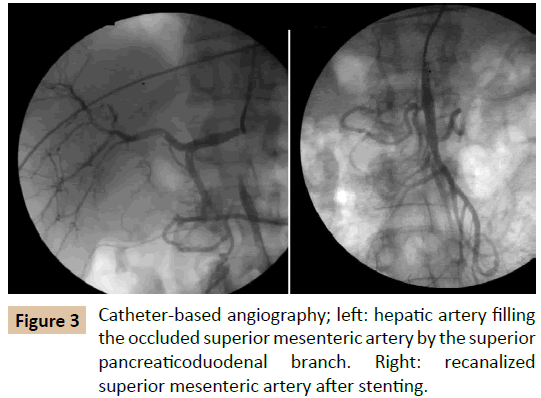
The case was discussed, and it was decided to treat the current life threatening condition namely the severe mesenteric ischemia; due to the critical affectation of the general aspect of the patient, it was considered the percutaneous approach as first choice; it was done through puncture of the left radial artery; the angiogram confirmed the ostial occlusion of the SMA that was filled by collaterals coming from the superior pancreaticoduodenal artery, branch of the hepatic artery (Figures 2 and 3 left); the study also confirmed severe stenosis of the left renal artery and triple coronary vessel disease.
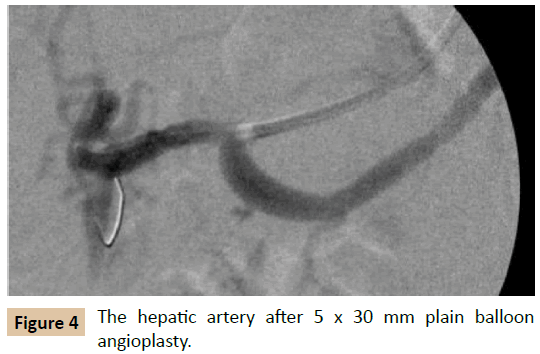
The SMA was recanalized using a 6F Radial guiding catheter (Boston Scientific), a 0.014” intermediate wire and a 2 x 20 mm balloon followed by a 5 x 30 mm bare metal stent at 16 atmospheres (PRO-Kinetic, Biotronik) with good result (Figure 3 right); then the balloon of the stent was utilized to dilate the hepatic artery with success and “stent-like” result (Figure 4); the right renal artery was stented during the same event.
The patient tolerated a complete dinner one hour after the procedure and was discharged from the hospital the other day; it was confirmed an immediate recovery of the life quality and significant weight gain in less than a week. As the patient is foreign on temporary stay in the Mayan Riviera, he lives in France, he went to his country, and where four months later the treatment was completed with double iliac artery stenting and percutaneous coronary intervention.
Discussion
The presented case is an example of the frequent concurrence of different areas of affectation during a global atherosclerosis that obligates the approach for diverse endovascular diagnostic and therapeutic approach; the chronic mesenteric ischemia a devastating condition whose frequency is still not well recognized but may be major than previously suspected and may become still more frequent as the population ages.
The recognition an early diagnosis of this entity may be lifesaving and must include the detection of other atherosclerosis affections such as the coronary tree. The radial approach is a very good option that allows rapid recovery and return to the usual life; when the left radial artery is accessed it permits to reach more distal arteries.
Conclusion
This case report encourages interventionalists for the early diagnosis of the mesenteric vascular syndromes and the percutaneous solution through the radial or ulnar artery.
Acknowledgment
We want to thank the invaluable collaboration of the personnel from The Clinics of the Heart and COSTAMED Group.
References
- Litten M (1875) Uber die Folgen Verschlusses der Arteria Mesaraica Superior. Arch Pathol Anat 63: 289.
- Acosta S, Ogren M, Sternby NH, Bergqvist D, Bjorck M (2004) Incidence of acute thrombo-embolic occlusion of the superior mesenteric artery - a population-based study. Eur J Vasc Endovasc Surg 27: 145-150.
- Yadav S (2014) A population-based study of incidence, risk factors, clinical spectrum and outcomes of ischemic colitis. Clin Gastroenterol Hepatol.
- Rosenblum JD, Boyle CM, Schwartz LB (1997) The mesenteric circulation. Anatomy and physiology. Surg Clin North Am 77: 289-306.
- Hohenwalter EJ (2009) Chronic mesenteric ischemia: diagnosis and treatment. Semin Intervent Radiol 26: 345-351.
- Oliva (2013) ACR Appropriateness Criteria imaging of mesenteric ischemia. Abdom Imaging 38: 714-719.
- Schaefer (2013) Comparison of non invsive imaging modalities for stenosis grading in mesenteric arteries. Rofo 185: 628-634.
- Kirkpatrick ID, Kroeker MA, Greenberg HM (2014) Biphasic CT with Mesenteric CT Angiography in the Evaluation of Acute Mesenteric Ischemia: Initial Experience.
- Pecoraro F, Rancic Z, Lachat M, Mayer D (2012) Chronic Mesenteric Ischemia: Critical Review and Guidelines for Management. Ann Vasc Sur.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences