Total Endovascular Repair by Sandwich Technique Thoracoabdominal Aortic Dissecting Aneurysm with Aneurysm Related Disseminated Intravascular Coagulation (DIC)
Zhi-Yuan Wu, Zuo-Guan Chen, Yong-Peng Diao, Sheng Yan, Yong-Jun Li and Yue-Xin Chen
DOI10.21767/2573-4482.100015
1Department of Vascular Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Science, Beijing, China
2Department of Vascular Surgery, Beijing Shijitan Hospital, Capital Medical University, Beijing, China
- *Corresponding Author:
- Yong-Jun Li
Department of Vascular Surgery
Peking Union Medical College Hospital
Chinese Academy of Medical Science, Beijing, China
Tel: + 01069152502
E-mail: yongjun.li@foxmail.com
Received date: June 21, 2016; Accepted date: July 21, 2016; Published date: July 28, 2016
Citation: Wu ZY, et al. Total Endovascular Repair by Sandwich Technique Thoracoabdominal Aortic Dissecting Aneurysm with Aneurysm Related Disseminated Intravascular Coagulation (DIC). Journal of Vascular & Endo Surgery. 2016, 1:3. doi: 10.21767/2573-4482.100015
Abstract
Purpose: To present a rare case of thoracoabdominal aortic dissecting aneurysm combined with aneurysm related disseminated intravascular coagulation (DIC) and the novel treatment of total endovascular aneurysm repair (EVAR) with Sandwich technique.
Case Report: A 78-year-old man was admitted with thoracoabdominal aortic dissecting aneurysm (TAADA) combined with bilateral iliac artery aneurysm (BIAA) accompanied by aneurysm related DIC. With adequate transfusion of blood components and a continuous subcutaneous injection of low molecular weight heparin, surgical repair of the multiple aortic lesions was carried out successfully. He received a total endovascular repair by sandwich technique to reconstruct all visceral branches. Postoperative laboratory evaluation demonstrated resolution of the coagulopathy. The optimal quality of life were achieved without any coagulopathy, paraplegia, pelvic organs ischemia or claudication and with an ideal blood pressure control during the 2-years’ following-up.
Conclusion: Total endovascular aneurysm repair by sandwich technique appears to be a feasible, safe, and effective treatment for the management of thoracoabdominal aortic dissecting aneurysm. Confidential conclusion needs more cases to be done.
Keywords
Endovascular aneurysm repair; Sandwich technique; Thoracoabdominal aortic aneurysm; Disseminated intravascular coagulation
Introduction
Since Parodi first reported the endovascular aneurysm repair (EVAR) in the management of abdominal aortic aneurysm (AAA) in 1991 [1], endovascular treatment has become the predominant method for Standford B dissection or infrarenal abdominal aneurysm [2]. However, some areas still pose a challenge to this technique, such as ascending aorta, aortic arch and suprarenal abdominal aorta.
Here we reported a rarely complicated case presenting with multiple aortic lesions including thoracoabdominal aortic dissecting aneurysm (TAADA) and bilateral iliac artery aneurysm (BIAA) accompanied by aneurysm related disseminated intravascular coagulation (DIC) in a 76-year-old male. Aorta lesions were repaired by total endovascular techniques. Superior mesenteric artery (SMA), celiac trunk and left renal artery (LRA) were reconstructed by sandwich technique and bilateral iliac artery aneurysms (BIAA) were excluded with coils of bilateral internal iliac artery.
Case Report
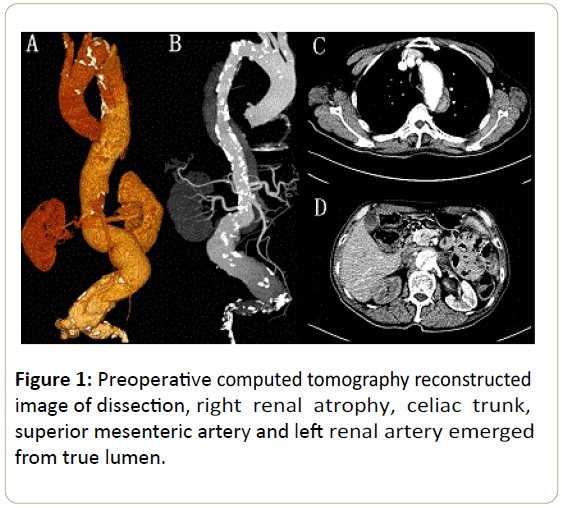
A 76-year-old male was transferred to our institution from another clinic, complaining of back pain for 7 months. Physical examination indicated an abdominal pulsatile midline mass about 7 cm. Blood test indicated DIC with prothrombin time (PT), 14.3s; activated partial thromboplastin time (APTT), 43.2s; prothrombin time international normalized ratio (INR), 1.25; platelet count (PLT), 89*109/L; fibrinogen (Fbg), 0.72 g/L; fibrinogen degradation products (FDP), 154.7 mg/L; D-Dimer 51.37 mg/L. He had a history of hypertension, coronary atherosclerotic heart disease, chronic renal dysfunction and smoking. Computed tomography angiography (CTA) indicated thoracoabdominal aortic dissecting aneurysm (TAADA) and bilateral iliac artery aneurysm (BIAA). The aneurysm diameter was 65 mm in the abdominal artery, 32 mm in the left common iliac artery and 23 mm in the right internal iliac artery (Figure 1). SMA, celiac trunk and LRA emerged from the true lumen and right renal artery stemmed from false lumen (Figure 1). Radionuclide dynamic renal imaging indicated the left glomerular filtration rate (GFR) was 24.5 ml/min, while 4.2 ml/min in the right.
Preoperative Management
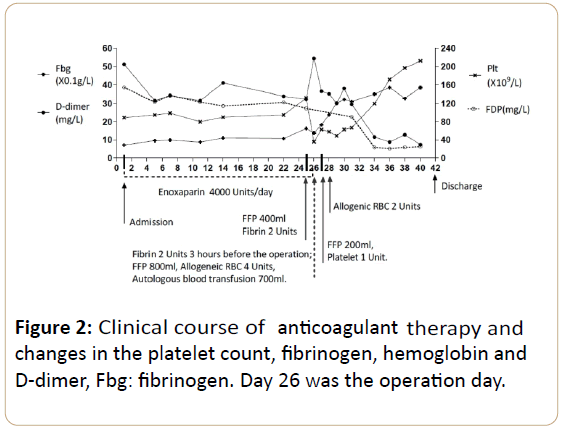
Due to his poor health situation, we attempted a total endovascular repair for all lesions; and due to the very complicated lesions, we made a deliberate plan by depicting the sketch of all lesions and calculating every size of lesion carefully before the intervention. After multidisciplinary consultation, DIC was attributed to the subsequent clot formation in aortic dissecting aneurysm and the patient was given subcutaneous injection of 4000U enoxaparin per day until the operative day. Four hundreds milliliter plasma and 2U fibrin were given on the day before operation. At that time, his laboratory data were as follows: PT, 13.2s; APTT, 37.1s; INR1.15; PLT, 133*109/L; Fbg, 1.63 g/L; FDP, 109.3 mg/L; DDimer 32.37 mg/L. Another 2U fibrin was injected 3 h before the operation (Figure 2).
To reduce the risk of paraplegia, cerebrospinal fluid drainage was performed one day before operation.
Procedure
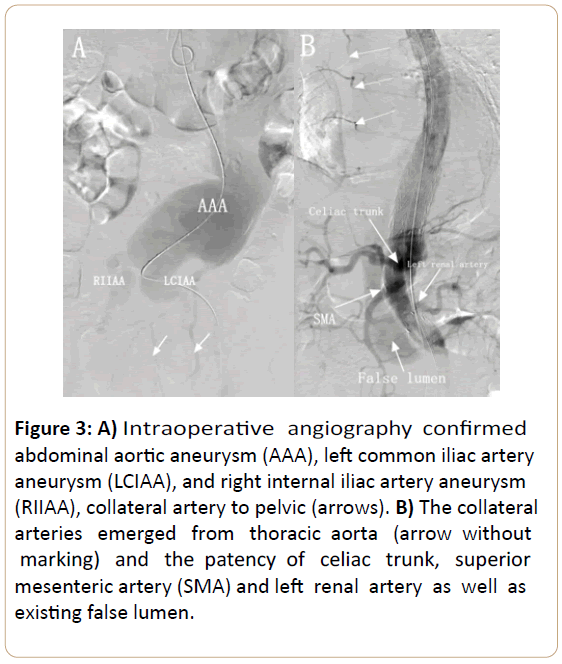
The patient was placed in supine position under general anesthesia. Then bilateral common femoral artery and left subclavian artery were exposed. After systemic heparinization, detailed angiography was made to confirm all lesions (Figure 3). Then three steps were done sequently to finish all lesions repair.
Figure 3: A) Intraoperative angiography confirmed abdominal aortic aneurysm (AAA), left common iliac artery aneurysm (LCIAA), and right internal iliac artery aneurysm (RIIAA), collateral artery to pelvic (arrows). B) The collateral arteries emerged from thoracic aorta (arrow without marking) and the patency of celiac trunk, superior mesenteric artery (SMA) and left renal artery as well as existing false lumen.
First, abdominal aneurysm and bilateral iliac aneurysm were excluded. Briefly, after bilateral internal iliac arteries were occluded with coils, a bifurcated main body of Gore Excluder (26-14-18; W. L. Gore & Associates, PXT) was deployed just below the left renal artery; and then both iliac limbs were extended to external iliac artery with extension graft (12-14-00; PXC in right; 12-10-00 and 12-12-00; PXC in left).
Second, dissection on the descending thoracic aorta was repaired. Two TAGs (28-15-00; W.L. Gore & Associates, TAG) was sequently deployed above the ostium of celiac artery to the distal of left subclavian artery.
Finally, the area of visceral arteries was bridged and all visceral arteries were reconstructed with Sandwich Technique. Due to a type III arch, three 8F sheaths (IMWCE-38-5-8. Cook) were advanced through the exposed left subclavian artery with 3 punctures in a 5 mm distances each. The 3 sheaths were accessed into celiac trunk, SMA and left renal artery individually. One 8-50 mm self-expandable stent graft (Viabahn; W.L. Gore & Associates), one 8-100 mm Viabahn, and one 6-100 mm Viabahn were ready to recannulate the celiac trunk, SMA and left renal artery separately. And then, another thoracic excluder (31-10-00; W.L. Gore & Associates, TAG) was used to bridge thoracic aortic and abdominal grafts, which already deployed. The joint of aortic graft were ballooned with Tri-Lobe Balloon Catheter (W.L. Gore & Associates, BCL2654). In the area of visceral arteries, grafts and VIABAHANs were ballooned simultaneously. Final angiography suggested a type II endoleak around the area of visceral branches. We decided to follow up.
The whole procedures lasted 472 m, including 157 m fluoroscopy. A total volume of 300 ml contrast was used. During the operation, 2,500 ml blood was lost, and 700 ml was received with Cell Saver. Another 800 ml fresh frozen plasma (FFP), and 4 units allogeneic red blood cell (RBC) were transfused. On the first postoperative day, 200ml plasma and 1 unit platelet were transfused; another 2 units allogeneic RBC were transfused on the second postoperative day, according to his blood examination (Figure 2).
The patient stayed in the Intensive Care Unit for 4 days after the operation and was discharged on 16th day postoperation. On the discharged day, his laboratory data turned back to a related normal level as follows: PT, 13.4s; APTT, 38.0s; INR, 1.17; PLT, 213*109/L; Fbg, 3.86 g/L; FDP,14.8 mg/L; D-Dimer 7.34 mg/L.
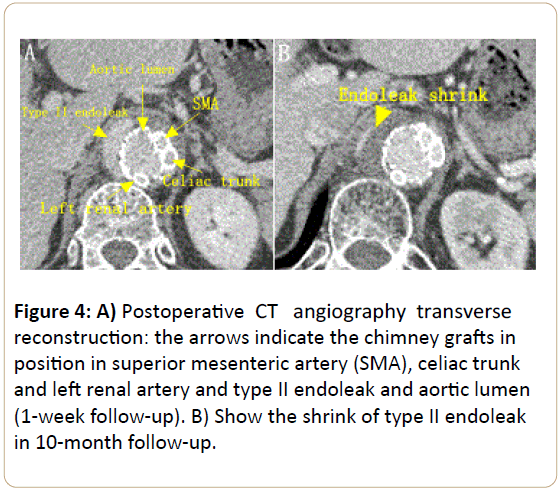
One week’s follow-up with CTA showed patency of the grafts and a persistent type II endoleak without deterioration (Figure 4A). Ten-month’s follow-up also showed adequate patency of all three branches, and the thrombosis in the descending false lumen as well as the shrink of the type II endoleak (Figure 4B).
Figure 4: A) Postoperative CT angiography transverse reconstruction: the arrows indicate the chimney grafts in position in superior mesenteric artery (SMA), celiac trunk and left renal artery and type II endoleak and aortic lumen (1-week follow-up). B) Show the shrink of type II endoleak in 10-month follow-up.
In the following 2 years’ follow-up, the optimal quality of life was achieved without any paraplegia, pelvic organs ischemia or claudication.
Discussion
Technical choice and success
The proximal or distal extension of aortic disease to visceral branches increases the complexity of EVAR and its consequent morbidity and mortality [3]. Because of ideal midterm outcome, branched and fenestrated stent grafts offer an attractive treatment option patients who are high risk for surgery [4], although fenestrated thoracic endovascular aortic repair was associated with higher mortality compared with the branched [5]. However, an important limitation regarding to these stent grafts is that they are custom made. Moreover, 20% to 30% of patients are thought unsuitable for these stent grafts because of tortuosity, angulation and calcification of the aorta [6]. The chimney, snorkel, periscope and sandwich grafts are cheaper than the fenestrated graft, require limited endovascular tools for implantation, and have immediate availability and broader applicability in the acute setting; these are suitable for patients who cannot withstand the time required for device customization [7]. The sandwich technique allows the revascularization of up to four side branches, comparing to the two permitted by the chimney technique. What’s more, sandwich technique holds potential for patients with difficult anatomy, especially given that they do not require customizations opposed to the branched and fenestrated stent grafts [8]. Lobato et al. reported that sandwich techniques a safe, well-tolerated, feasible alternative using ready-to-use endoprosthesis to provide efficient visceral revascularization in 15 patients with TAAAs [9]. Considering the tortuosity, calcification of the aorta, the multiple lesions and the complexity of the EVAR in this patient, we decided to adopt sandwich technique to reconstruct the visceral arteries. This technique is outside the standard instructions for use, therefore careful planning and long-term follow-up are mandatory [10]. In this case, we made a deliberate plan and a long-term follow-up. The patient got a satisfied quality of life. We decrease the risk of a possible type I endoleak by overlapping 2-3 cm between the branch stent and the aortic endograft to guarantee a correct seal as well as durability, and sacrificing the right renal artery. Finally, we got technique success and a satisfied clinical effect.
Management of DIC
Disseminated intravascular coagulation (DIC) secondary to aortic dissection was first described by Fine et al. [11]. It is a life-threatening complication and is rarely reported [12]. The precise pathogenesis of DIC related to aortic dissection remains unclear. The treatment for DIC caused by an aortic dissecting aneurysm, involves lesion removal and infusion of coagulation factors during the operation to minimize blood lose [13]. Low molecular weight heparin, oral direct Factor Xa inhibitor, heparin, recombinant human soluble thrombomodulin were alternative options for controlling the DIC [14-17]. In this case, subcutaneous enoxaparin injection of 4000 units per day was taken for this patient until the operation. FFP, fibrin, platelet and RBC were transfused during the perioperative period as mentioned above. As shown in Figure 2 there is a clear change in coagulation patterns after surgery. The D-dimer changed from 54.66 mg/L to 36.59, and gradually to 7.34 mg/L. The platelet count turned up from 36*109/L to 63*109/L and climbed to 213*109/L. Changes can also be observed both on Fbg and FDPs. Except for transfusion of blood components and the anticoagulant, surgical correction contributed much to the solution of aneurysm related DIC. Platelets, hemoglobin and fibrinogen were all consumed by clot formation in false lumen in the postoperative 2 days. Finally, we managed the coagulopathy as all values gradually turned back to a related normal level. This patient was free of aneurysm related DIC when he was discharged home.
Postoperative complications
This patient was free from ischemic complications from both Bilateral Internal Iliac Artery Occlusion and Spinal Cord artery exclusion. Although bilateral internal iliac artery occlusion may leave patients with significant life-limiting issues postoperatively including buttock claudication up to 35%, impotence up to 24%, and colon or spinal cord ischemia [18]. However, in this case there are several collateral artery from visceral vessel to pelvis may keep off complications. Meanwhile, this patient might encounter high risk of spinal cord ischemia and paraplegia as long aortic lesion was repaired by graft. Cerebrospinal fluid drainage was applied and thoracic aortic segment artery (SAs) above Th4 and partial collateral arteries drive from aortic were tried to be preserved as far as possible (Figure 3B).
Conclusion
In our case, total endovascular aneurysm repair by sandwich technique appears to be a feasible, safe, and effective treatment for the management of thoracoabdominal aortic dissecting aneurysm and bilateral iliac artery aneurysm. Meanwhile, endovascular stent-grafting is an acceptable way for aneurysm accompanied by DIC. More information will be provided regarding patency and durability in further follow-up.
References
- Parodi JC, Palmaz JC, Barone HD (1991) Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Annals of Vascular Surgery 5:491-499.
- Jongkind V, Yeung KK, Akkersdijk GJ, Heidsieck D, Reitsma JB, et al. (2010) Juxtarenal aortic aneurysm repair. Journal of Vascular Surgery 52:760-767.
- Hobo R, Sybrandy JE, Harris PL, Buth J, Collaborators E (2008) Endovascular repair of abdominal aortic aneurysms with concomitant common iliac artery aneurysm: outcome analysis of the EUROSTAR Experience. Journal of Endovascular Therapy: An Official Journal of the International Society of Endovascular Specialists15:12-22.
- Haulon S, Amiot S, Magnan PE, Becquemin JP, Lermusiaux P, et al. (2010) An analysis of the French multicentre experience of fenestrated aortic endografts: medium-term outcomes. Annals of Surgery 251:357-362.
- Tsilimparis N, Debus ES, von Kodolitsch Y, Wipper S, Rohlffs F, et al. (2016) Branched versus fenestrated endografts for endovascular repair of aortic arch lesions. Journal of Vascular Surgery.
- De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, et al. (2010) Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. The New England Journal of Medicine 362:1881-1889.
- Georgiadis GS, van Herwaarden JA, Antoniou GA, Giannoukas AD, Lazarides MK, et al. (2016) Fenestrated stent grafts for the treatment of complex aortic aneurysm disease: A mature treatment paradigm. Vascular Medicine 21:223-238.
- Buck DB, van Herwaarden JA, Schermerhorn ML, Moll FL (2014) Endovascular treatment of abdominal aortic aneurysms. Nature Reviews Cardiology11:112-123.
- Lobato AC, Camacho-Lobato L (2012) A new technique to enhance endovascular thoracoabdominal aortic aneurysm therapy--the sandwich procedure. Seminars in Vascular Surgery 25:153-160.
- Kim HK, Song I, Huh S (2016) The Upside-Down Gore Excluder Limb and Double-Barrel Sandwich Technique for Penetrating Aortic Ulcer and Iliac Aneurysm Exclusion. Vascular Specialist International 32:17-21.
- Fine NL, Applebaum J, Elguezabal A, Castleman L (1967) Multiple coagulation defects in association with dissecting aneurysm. Archives of Internal Medicine 119:522-526.
- Aboulafia DM, Aboulafia ED (1996) Aortic aneurysm-induced disseminated intravascular coagulation. Annals of Vascular Surgery 10:396-405.
- Yoon SH, Cho YS, Park CY, Chung CH (2004) Disseminated intravascular coagulation associated with aortic dissecting aneurysm. The Korean Journal of Internal Medicine 19:134-136.
- Perry JH, Lazar HL, Quillen K, Sloan JM (2012) Successful long-term management of aneurysm-associated chronic disseminated intravascular coagulation with low molecular weight heparin. Journal of Cardiac Surgery 27:730-735.
- Kawano H, Hata T, Uda A, Maemura K (2015) Use of rivaroxaban for the effective management of disseminated intravascular coagulation associated with abdominal aortic aneurysm. Internal Medicine 54:2625-2628.
- Miyahara S, Yasu T, Yamada Y, Kobayashi N, Saito M, et al. (2007) Subcutaneous injection of heparin calcium controls chronic disseminated intravascular coagulation associated with inoperable dissecting aortic aneurysm in an outpatient clinic. Internal Medicine 46:727-732.
- Hoshina K, Shigematsu K, Hosaka A, Okamoto H, Miyata T, et al. (2014) The effect of recombinant human soluble thrombomodulin on disseminated intravascular coagulation in an abdominal aortic aneurysm. Blood Coagulation &Fibrinolysis: an International Journal in Hemostasis and Thrombosis 25:389-391.
- Rayt HS, Bown MJ, Lambert KV, Fishwick NG, McCarthy MJ, et al. (2008) Buttock claudication and erectile dysfunction after internal iliac artery embolization in patients prior to endovascular aortic aneurysm repair. Cardiovascular and Interventional Radiology 31:728-734.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences